- Department of Neurosurgery, Otsu City Hospital, Otsu, Shiga, Japan,
- Department of Neurosurgery, Biwako Ohashi Hospital, Otsu, Shiga, Japan.
Correspondence Address:
Motohiro Takayama, Department of Neurosurgery, Otsu City Hospital, Otsu, Shiga, Japan.
DOI:10.25259/SNI_1228_2021
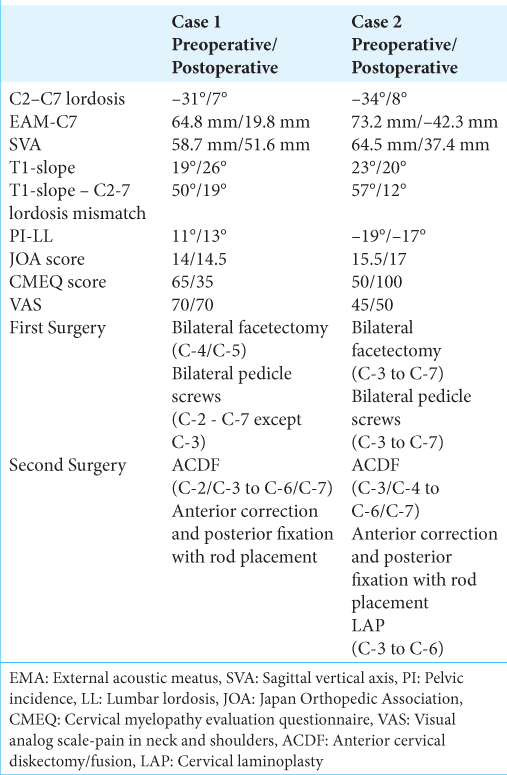
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Motohiro Takayama1, Yoshinori Maki2. Management of two patients with dropped head syndrome utilizing anterior-posterior cervical surgery. 18-Feb-2022;13:56
How to cite this URL: Motohiro Takayama1, Yoshinori Maki2. Management of two patients with dropped head syndrome utilizing anterior-posterior cervical surgery. 18-Feb-2022;13:56. Available from: https://surgicalneurologyint.com/surgicalint-articles/11403/
Abstract
Background: Two elderly patients with dropped head syndromes (DHS) were successfully treated with circumferential cervical surgery.
Case Description: The two patients, respectively, 72 and 53 years of age, both underwent two-staged surgical procedures. The first surgery included the posterior placement of bilateral pedicle screws with multilevel facetectomies, followed by multilevel anterior cervical discectomy/fusion and posterior rod fixation.
Conclusion: Circumferential decompression/fusion successfully addressed chin on chest deformity in two older patients.
Keywords: Anterior fixation, Dropped head syndrome, Laminoplasty, Posterior fixation, Surgery
INTRODUCTION
Dropped head syndrome (DHS) is a chin-on-chest deformity attributed to a noninflammatory myopathy of the cervical paraspinal muscles resulting in weakness of the cervical extensor musculature.[
CASE PRESENTATION
Case 1
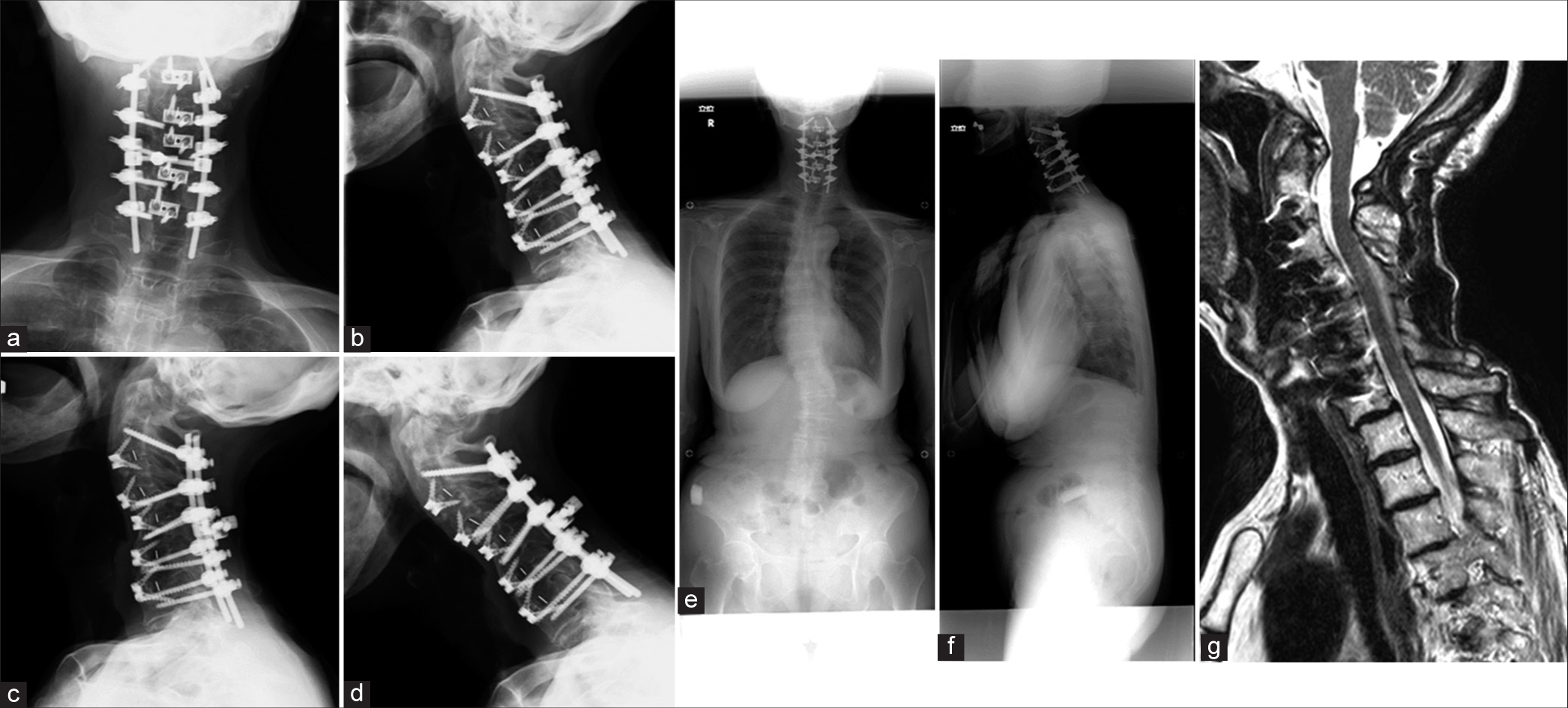
A 72-year-old female presented with a progressive DHS syndrome and mild myelopathy (i.e., bilateral C5-C7 hyperreflexia). X-rays showed DHS, while the magnetic resonance images documented posterior compression at C-2 to C-3, and stenosis from C-5 to C-7 [
Case 2
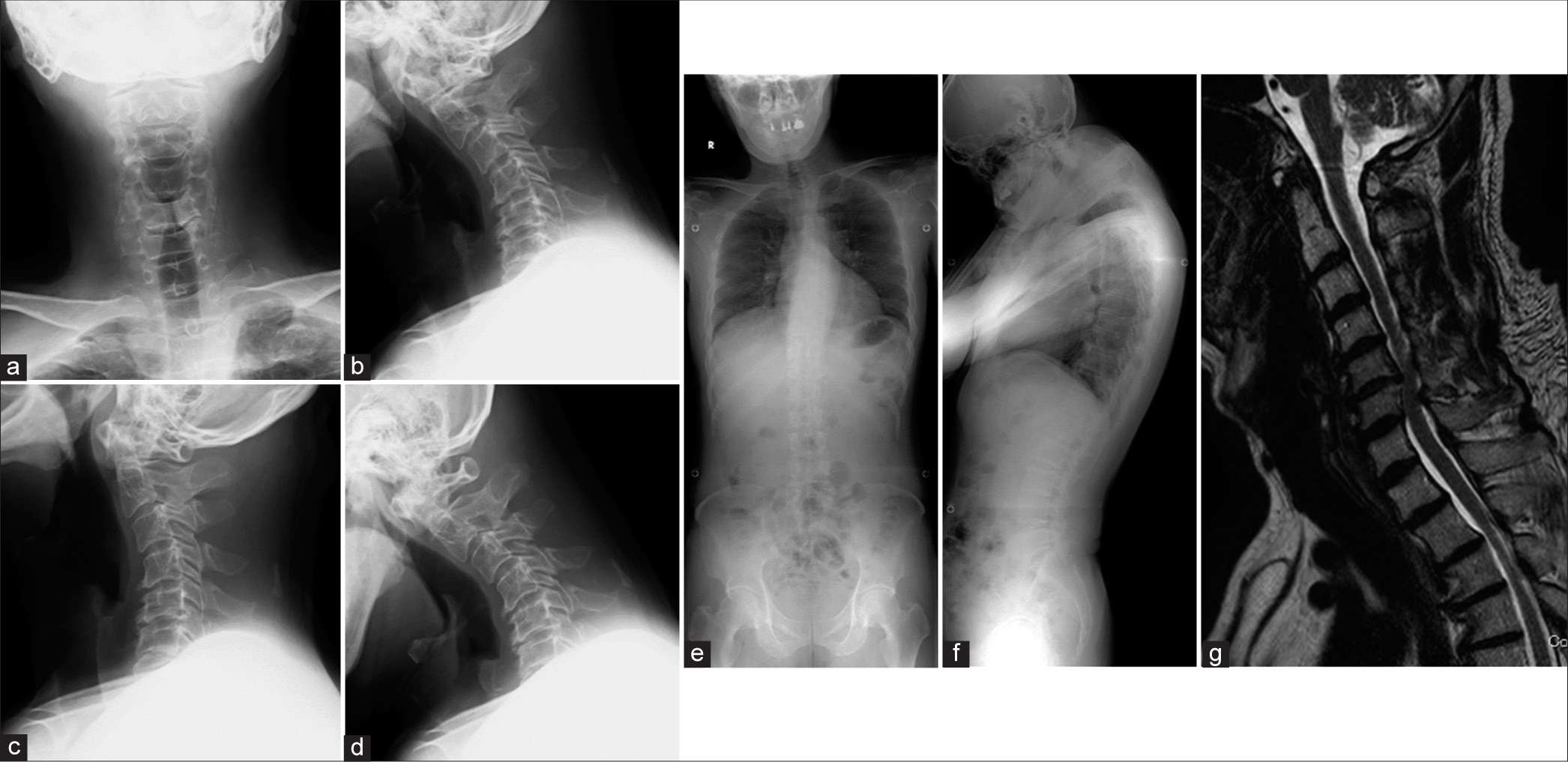
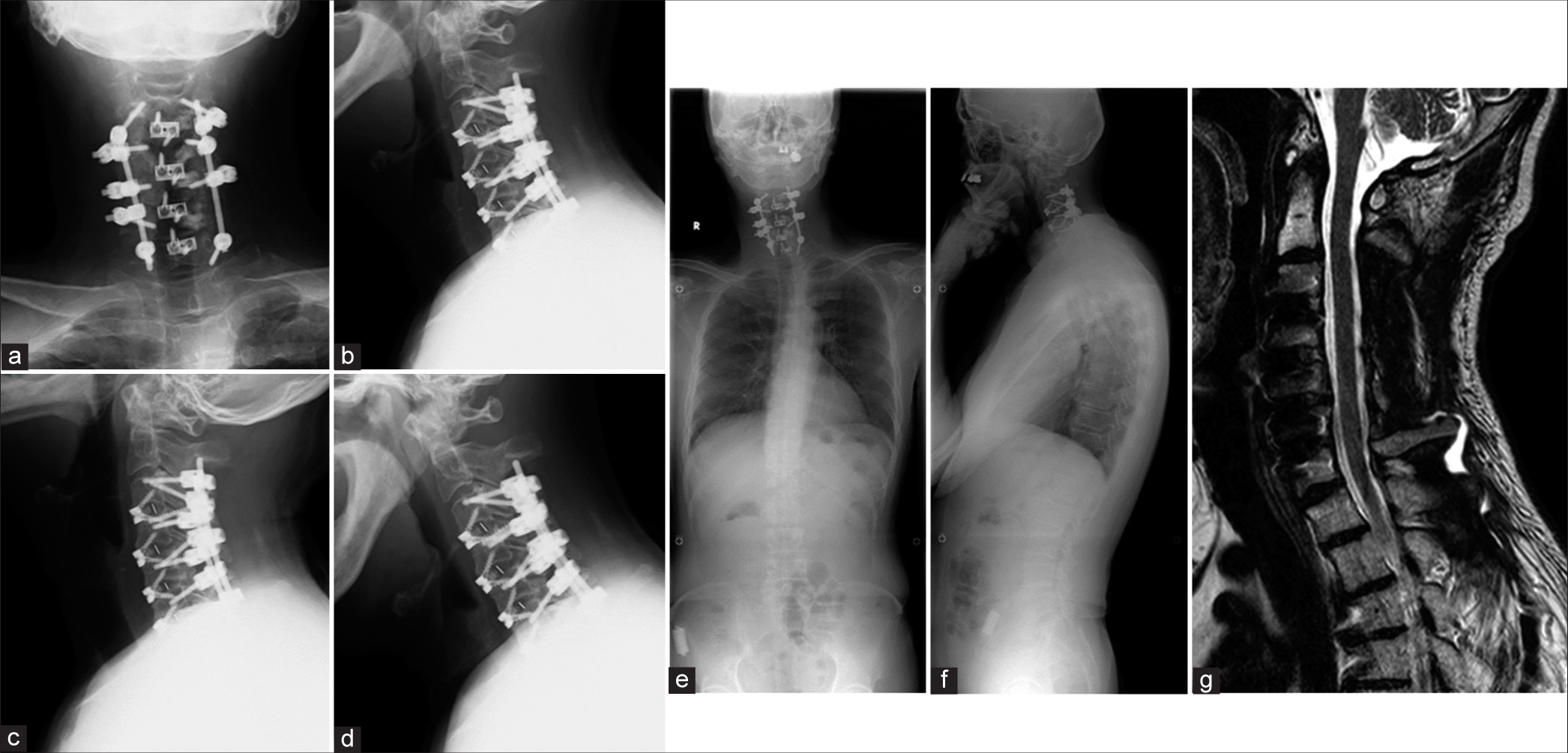
A 53-year-old male presented without myelopathy. Preoperative X-rays demonstrated DHS, while the MR showed C-5 to C-6 cord compression [
DISCUSSION
DHS can be classified into three groups based on preoperative radiological parameters; Type 1 (SVA ≤0 mm and PI-LL ≤10°), Type 2 (SVA > 0 mm and PI-LL ≤10°), and Type 3 (PI-LL >10°).[
CONCLUSION
Here, we corrected the DHS syndrome in two older patients utilizing a combined circumferential 360 degree decompression/fusion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank Dr. Ryota Ishibashi for his support of this study.
References
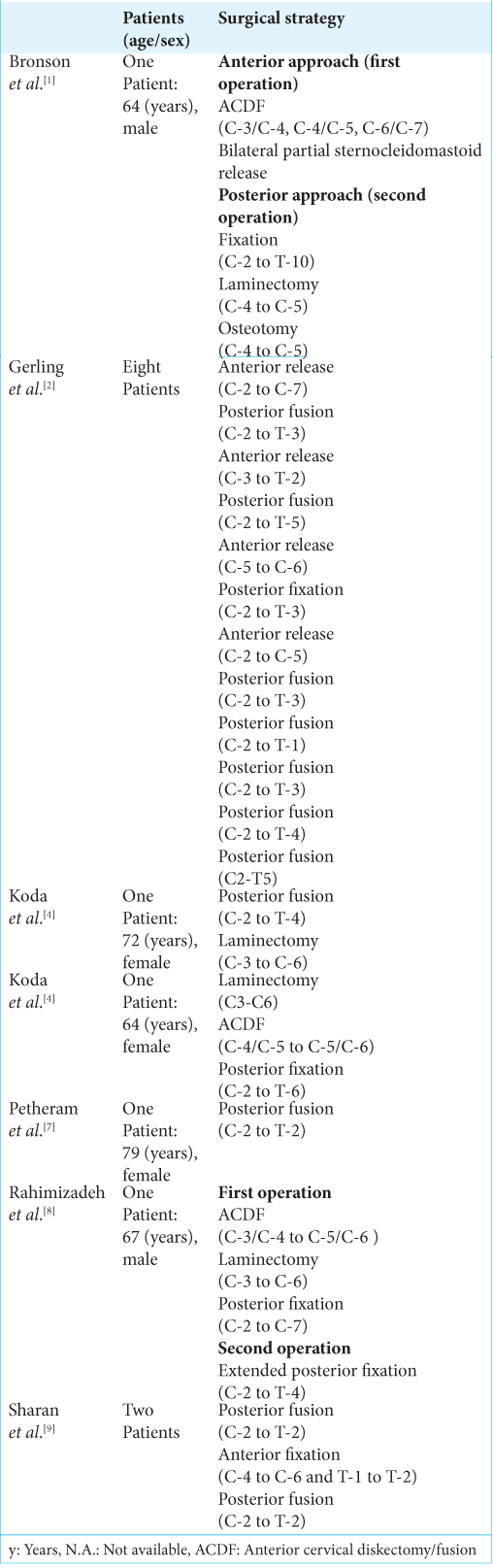
1. Bronson WH, Moses MJ, Protopsaltis TS. Correction of dropped head deformity through combined anterior and posterior osteotomies to restore horizontal gaze and improve sagittal alignment. Eur Spine J. 2018. 27: 1992-9
2. Gerling MC, Bohlman HH. Dropped head deformity due to cervical myopathy: surgical treatment outcomes and complications spanning twenty years. Spine. 2008. 33: E739-45
3. Katz JS, Wolfe GI, Burns DK, Bryan WW, Fleckenstein JL, Barohn RJ. Isolated neck extensor myopathy: A common cause of dropped head syndrome. Neurology. 1996. 46: 917-21
4. Koda M, Furuya T, Inada T, Kamiya K, Ota M, Maki S. Resolution of low back symptoms after corrective surgery for dropped-head syndrome: A report of two cases. BMC Res Notes. 2015. 8: 545
5. Kudo Y, Toyone T, Endo K, Matsuoka Y, Okano I, Ishikawa K. Impact of Spinopelvic sagittal alignment on the surgical outcomes of dropped head syndrome: A multi-center study. BMC Musculoskelet Disord. 2020. 21: 382
6. Kusakabe T, Endo K, Sawaji Y, Suzuki H, Nishimura H, Matsuoka Y. Mode of onset of dropped head syndrome and efficacy of conservative treatment. J Orthop Surg. 2020. 28: 2309499020938882
7. Petheram TG, Hourigan PG, Emran IM, Weatherley CR. Dropped head syndrome: A case series and literature review. Spine. 2008. 33: 47-51
8. Rahimizadeh A, Soufiani HF, Rahimizadeh S. Cervical spondylotic myelopathy secondary to dropped head syndrome: Report of a case and review of the literature. Case Rep Orthop. 2016. 2016: 5247102
9. Sharan AD, Kaye D, Malveaux WM, Riew KD. Dropped head syndrome: Etiology and management. J Am Acad Orthop Surg. 2012. 20: 766-74
10. Suarez GA, Kelly JJ. The dropped head syndrome. Neurology. 1992. 42: 1625-7