- Division of Neurosurgery, Department of Surgery, McMaster University, Hamilton, Canada
Correspondence Address:
Ahmed Al Jishi
Division of Neurosurgery, Department of Surgery, McMaster University, Hamilton, Canada
DOI:10.4103/sni.sni_351_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Al Jishi, Naresh Murty. Massive lumbar spine hematoma post-spinal tap. 06-Dec-2017;8:293
How to cite this URL: Ahmed Al Jishi, Naresh Murty. Massive lumbar spine hematoma post-spinal tap. 06-Dec-2017;8:293. Available from: http://surgicalneurologyint.com/surgicalint-articles/massive-lumbar-spine-hematoma-post%e2%80%91spinal-tap/
Abstract
Background:Lumbar puncture is a well-known procedure. The indications for lumbar puncture vary among different medical and surgical disciplines, though obtaining a sample for cerebrospinal fluid analysis is the most common one. A normal coagulation profile is crucial prior to pursing the procedure. Occasionally, an urgent sample is needed to guide an appropriate treatment while the patient's coagulation status is suboptimum. In those specific critical situations, some may accept suboptimal correction owing to the urgency of the case.
Case Description:We report a case for a patient with Burkitt lymphoma who presented with mild neuroaxial symptoms. An urgent cerebrospinal fluid sample was required which was taken after correcting his platelets count to 53.4 × 109/L. He developed a massive multi-compartmental thoracolumbar hematoma with acute cauda equine syndrome requiring surgical intervention. Despite aggressive management, he remained permanently paraplegic with functional status that negatively affected his overall outcome.
Conclusion:Lumbar puncture is a useful diagnostic and treatment tool. Although serious events are seldom, they can be detrimental. A precaution not to underestimate such events in practicing lumbar, especially in patients with suboptimum coagulation state. Image-guided procedure can be useful and should be considered in appropriately selected patients.
Keywords: Lumbar puncture, spinal tap, spinal hematoma
INTRODUCTION
Spinal hematoma is an important radiological diagnosis requiring immediate clinical correlation. It commonly occurs because of trauma. Other etiologies include vascular anomaly, bleeding, diathesis, or anticoagulant therapy. Spinal hematomas are usually treated conservatively unless patients present with neurological compromise. One cause for spinal hematoma is lumbar puncture (LP), which often goes without close follow up unless the patient reports issues. LP is a commonly practiced procedure and usually done as a day procedure with low incidence of complications. However, certain cases should be handled with exceptional care such as immunocompromised and coagulopathic patients. In this article, we discuss a serious lumbar spinal hematoma that occurred after a LP to illustrate its implication on the overall clinical outcome along with a brief literature review.
CASE DESCRIPTION
A 45-year-old gentleman presented with a 6-week history of progressive decline in function and easy bruising. He had mild ataxia along with binuclear horizontal diplopia. Acute lymphocytic leukemia was suspected due to high leukocytes count (79.1 × 109/L) and abnormal cells (53.4 × 109/L) on blood smear in favor of blast cells. Platelet count was low (22 × 109/L). Sugar coating along the brainstem was ruled out using MRI brain with gadolinium. Thus, an urgent LP was planned to assess tumor seeding within the CSF after correcting platelets to 51 × 109/L. A diagnosis of Burkitt lymphoma was made thereafter. Nevertheless, within 6 hours of the LP, the patient experienced initial left leg pain which was treated empirically. As bilateral numbness developed, an MRI spine was ordered and a diagnosis of spinal hematoma was made [
Figure 1
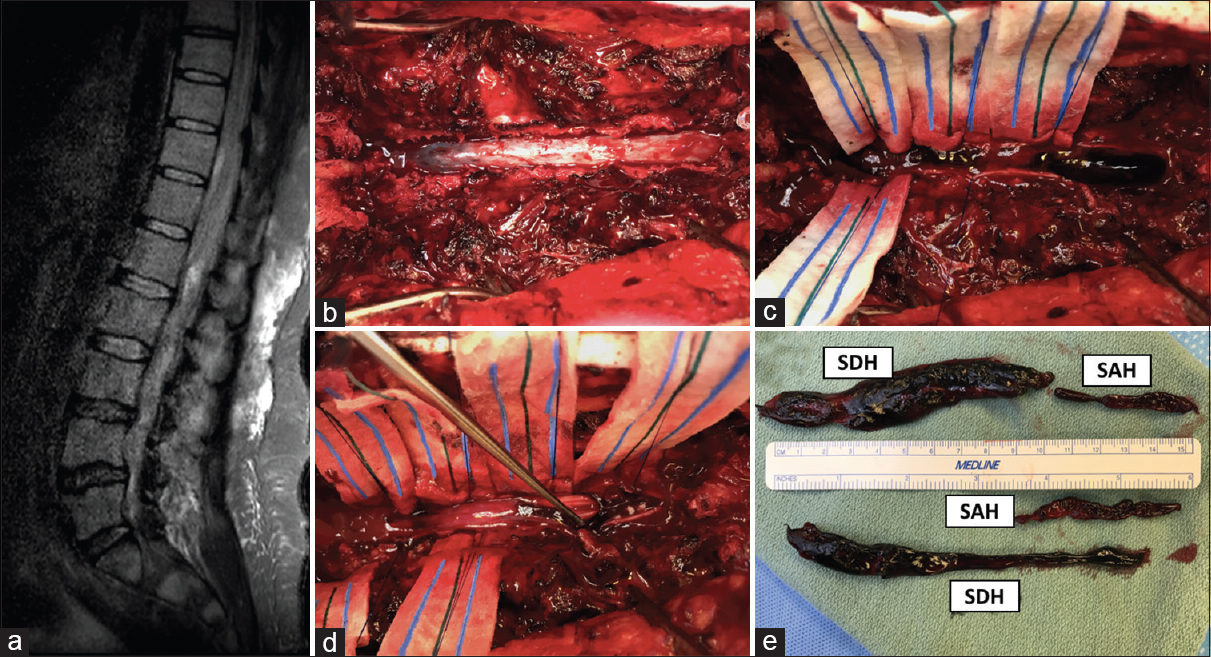
(a) Lumbar plain MRI depicts a large intraspinal hematoma which extends from T11 down to L5 with severe neural compromise. (b) Intraoperative exploration after T11–L3 laminectomy and evacuation of spinal epidural hematoma (not shown in this photo). (c) Giant spinal subdural hematoma was noticed post midline durotomy. (d) Incision of the arachnoid layer was done due to evidence of large subarachnoid clots which were retrieved successfully. (e) Multiple large and thick spinal hematomas from subdural and subarachnoid spaces
DISCUSSION
LP is a commonly practiced procedure. It is usually performed at the bedside based on anatomical surface markings. Image-guided assisted procedure is occasionally used in technically challenging cases. The simplicity of the procedure as well as the low incidence of complication other than headache has perhaps given it greater popularity among different clinical disciplines. In fact, majority of LP cases are done on the same day of the surgery or in emergency rooms.
However, LP is still associated with serious complications that are often discounted due to low incidence.[
Although the accurate incidence of spinal hematoma is unknown, it is estimated that approximately 4% of symptomatic spinal hematomas are related to traumatic LP. They are commonly located inclusively with the epidural space in 75% of the cases, whereas subarachnoid hemorrhage and spinal subdural hematoma can be found in 15.7% and 4.1%, respectively. Multi-compartmental spinal hematomas are rare and thought to present in 0.33%.[
Surgery is indicated for symptomatic patients with reported complete neurological recovery in almost 40%. The timing of surgery is vital and associated with improved neurological outcome when done in less than 36 hours.[
Informed consent
For this type of study formal consent is not required.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that they have no conflicts of interest. There was no grant support for this study.
Acknowledgements
We would like to acknowledge Christina Vandervlist for her editorial assistance in preparing the manuscript for publication.
References
1. Brown MW, Yilmaz TS, Kasper EM. Iatrogenic spinal hematoma as a complication of lumbar puncture: What is the risk and best management plan?. Surg Neurol Int. 2016. 7: S581-9
2. Evans RW. Complications of lumbar puncture. Neurol Clin. 1998. 16: 83-105
3. Groen RJ, van Alphen HA. Operative treatment of spontaneous spinal epidural hematomas: A study of the factors determining postoperative outcome. Neurosurgery. 1996. 39: 494-508
4. Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: A literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003. 26: 1-49