- Departments of Neurosurgery, National Hospital Organization Mito Medical Center, Sakura No Sato, Higashiibaraki,
- University of Tsukuba, Amakubo, Tsukuba, Ibaraki, Japan.
Correspondence Address:
Koji Hirata
University of Tsukuba, Amakubo, Tsukuba, Ibaraki, Japan.
DOI:10.25259/SNI_76_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Koji Hirata, Tomosato Yamazaki, Noriyuki Kato, Susumu Yasuda, Akira Matsumura. Mechanical thrombectomy for occlusion near a ruptured intracranial aneurysm: A case report. 23-May-2020;11:120
How to cite this URL: Koji Hirata, Tomosato Yamazaki, Noriyuki Kato, Susumu Yasuda, Akira Matsumura. Mechanical thrombectomy for occlusion near a ruptured intracranial aneurysm: A case report. 23-May-2020;11:120. Available from: https://surgicalneurologyint.com/surgicalint-articles/10038/
Abstract
Background: While recent randomized clinical trials have shown the efficacy of mechanical thrombectomy for acute large vessel anterior cerebral occlusion, cases in patients with a subarachnoid hemorrhage (SAH) were excluded from the study.
Case Description: A 58-year-old man presented with a SAH as a result of a ruptured middle cerebral artery aneurysm. Coil embolization was performed, and a right intracranial angiography showed remnants of an aneurysmal neck. However, the following angiography also revealed a thromboembolic complication that occurred in the same territory as the ruptured aneurysm. The patient underwent a rescue mechanical thrombectomy under the working projection. We deployed a retrieval stent without covering the aneurysmal neck. The occluded vessel was recanalized without any hemorrhagic complication. Due to minimal intracerebral infarction, the patient had good outcomes.
Conclusion: Mechanical thrombectomy is a useful option to retrieve a clot from an occluded intracranial vessel located near a ruptured aneurysm. Approaching the clot at the working projection is important to ensure safety in the setting of a ruptured aneurysm.
Keywords: coil embolization, Mechanical thrombectomy, Ruptured aneurysm, Thromboembolic complication
BACKGROUND
While recent randomized clinical trials have demonstrated the efficacy of mechanical thrombectomy for acute large vessel anterior cerebral occlusion, patients with a subarachnoid hemorrhage (SAH) were excluded from the study.[
CASE DESCRIPTION
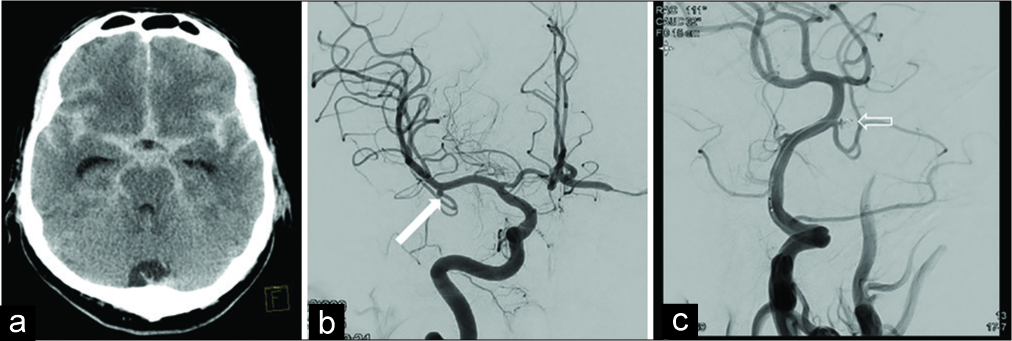
A 58-year-old man was admitted to our emergency department with an acute onset of headache. Computed tomography (CT) showed a diffused SAH [
Figure 1:
(a) A computed tomography revealing a subarachnoid hemorrhage. (b) A digital subtraction angiography revealing a right-sided middle cerebral aneurysm. (arrow: aneurysm). (c) A right internal carotid angiography after coil embolization revealing that the aneurysm became neck remnant (open arrow: coil).
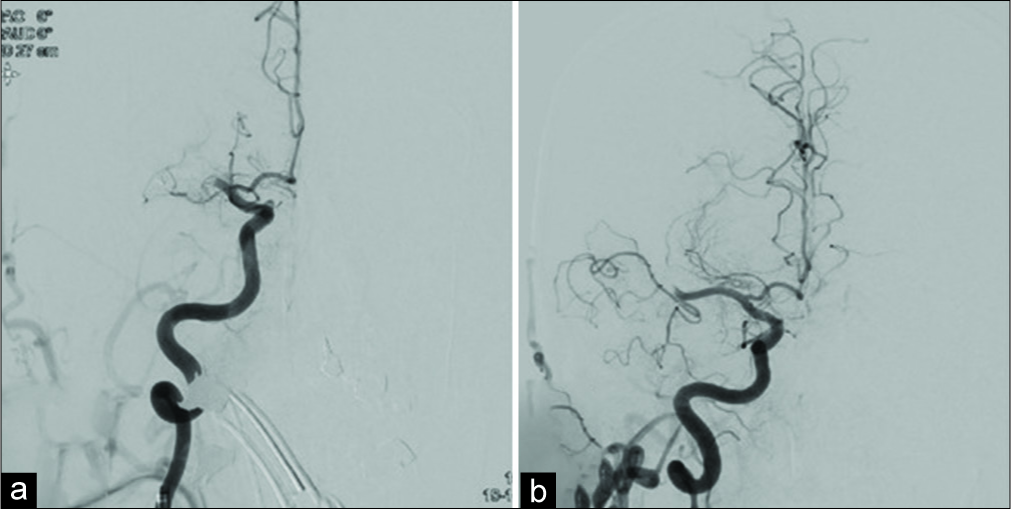
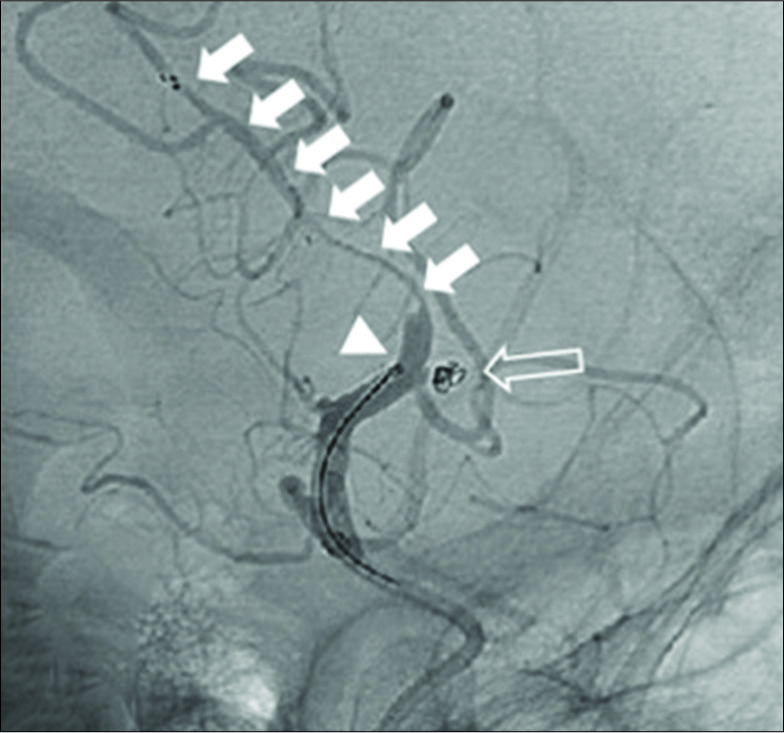
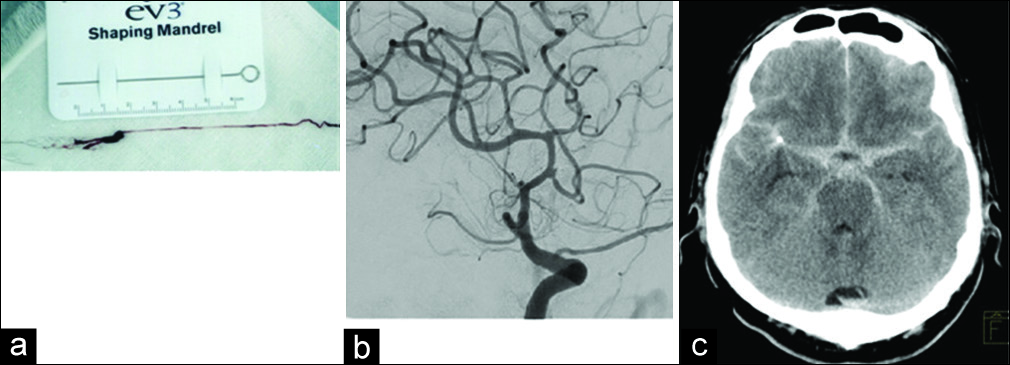
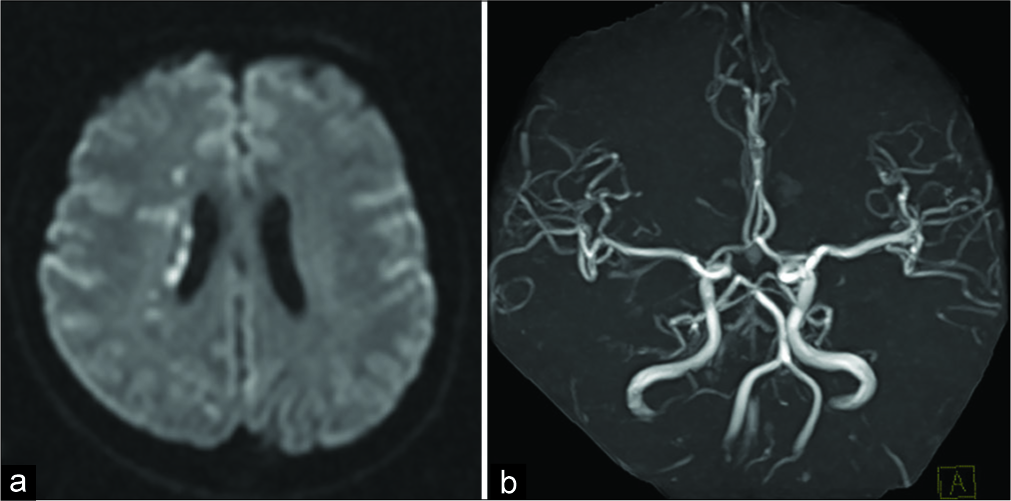
After removing the microcatheter, a right internal carotid angiography (ICAG) revealed an occlusion at the proximal right MCA M1 segment [
DISCUSSION
Our case demonstrates two major findings. First, clots occurring near a ruptured aneurysm during thromboembolic complications can be retrieved using a mechanical thrombectomy. Thromboembolism is major complication of coil embolization for a ruptured aneurysm, with an incidence rate of 6–10%.[
Second, using the working projection for coil embolization is important to ensure safety while performing a mechanical thrombectomy. When the clot is located at the same territory as the ruptured aneurysm, care needs to be taken to ensure that the aneurysm does not rebleed during the mechanical thrombectomy maneuver. Initially, as the shorter time for recanalization took priority, the working projection was not obtained. The working projection could show the position of the aneurysm in relation the clot. When the micro- guidewire penetrated the distal segment of the aneurysm, the maneuver would be safer under a working projection than under a general angle. Furthermore, the wall of the aneurysmal vessel was fragile and therefore needed less pressure on the aneurysmal neck to prevent rerupture. A previous report showed that high-resolution MRI of the vessel wall could detect vessel damage and that the segmental enhancement was found at the site of the retrievable stent placement.[
CONCLUSION
This case highlighted two important findings. Mechanical thrombectomy for thromboembolic complications when a ruptured aneurysm is in the same vascular territory should be considered for revascularization and using the working projection for coil embolization is required for safely undergoing this procedure, when the ruptured aneurysm is near the clot.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahn JH, Jun HS, Song JH, Cho BM, Lee HK, Kim BC. Rescue mechanical thrombectomy using a retrievable stent for thromboembolic occlusion occurring during coil embolization of ruptured intracranial aneurysms. J NeuroInterv Surg. 2017. 9: 244-9
2. Fransen PS, Beumer D, Berkhemer OA, van den Berg LA, Lingsma H, van der Lugt A. MR clean, a multicenter randomized clinical trial of endovascular treatment for acute ischemic stroke in the Netherlands: Study protocol for a randomized controlled trial. Trials. 2014. 15: 343-
3. Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009. 73: 1066-72
4. Nguyen TN, Malisch T, Castonguay AC, Gupta R, Sun CH, Martin CO. Balloon guide catheter improves revascularization and clinical outcomes with the solitaire device: Analysis of the North American solitaire acute stroke registry. Stroke. 2014. 45: 141-5
5. Nomura M, Mori K, Tamase A, Kamide T, Seki S, Iida Y. Thromboembolic complications during endovascular treatment of ruptured cerebral aneurysms. Interv Neuroradiol. 2018. 24: 29-39
6. Park HK, Horowitz M, Jungreis C, Genevro J, Koebbe C, Levy E. Periprocedural morbidity and mortality associated with endovascular treatment of intracranial aneurysms. Am J Neuroradiol. 2005. 26: 506-14
7. Ross IB, Dhillon GS. Complications of endovascular treatment of cerebral aneurysms. Surg Neurol. 2005. 64: 12-8
8. Seo WK, Oh K, Suh SI, Seol HY. Clinical significance of wall changes after recanalization therapy in acute stroke: High-resolution vessel wall imaging. Stroke. 2017. 48: 1077-80
9. Yoon CH, Lee HW, Kim YS, Lee SW, Yeom JA, Roh J. Preliminary study of tirofiban infusion in coil embolization of ruptured intracranial aneurysms. Neurosurgery. 2018. 82: 76-84
10. Zhang S, Hao Y, Tian X, Zi W, Wang H, Yang D. Safety of intra-arterial tirofiban administration in ischemic stroke patients after unsuccessful mechanical thrombectomy. J Vasc Interv Radiol. 2019. 30: 141-7