- Department of Neurological Surgery, Feinberg School of Medicine, Northwestern University, Chicago, Illinois,
- Faculty of Medicine, American University of Beirut, Riad El-Solh,
- Department of Neurosurgery, Neuroscience Research Center, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon.
Correspondence Address:
Jawad Fares
Department of Neurosurgery, Neuroscience Research Center, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon.
DOI:10.25259/SNI_538_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jawad Fares, Mohamad Y. Fares, Youssef Fares. Medical schools in times of war: Integrating conflict medicine in medical education. 03-Jan-2020;11:5
How to cite this URL: Jawad Fares, Mohamad Y. Fares, Youssef Fares. Medical schools in times of war: Integrating conflict medicine in medical education. 03-Jan-2020;11:5. Available from: https://surgicalneurologyint.com/surgicalint-articles/9829/
Abstract
Amid the rise in conflict and war and their ensuing repercussions, traumatic injuries, psychological distress, and communicable diseases spread widely. Today, health-care providers in the Middle East are faced with new and unfamiliar cases resulting from the use of new and advanced types of weapons. In addition, there has not been enough emphasis on hands-on experiences in medical school, which can be imperative in times of war. Lack of academia is another inadequacy that limits the transmission of knowledge onto the newer generations. Here, we will shed light on the inadequacies in medical curricula in the Middle East when it comes to addressing patients of war. We also call for action to advance medical education in war-ridden areas by incorporating “conflict medicine” as an integral module in medical curricula.
Keywords: Conflict medicine, Medical education, Middle East, War
INTRODUCTION
War is a major contributor to traumatic injuries and psychological distress. The Middle East, being one of the most conflict-ridden regions in the world today, continues to be an unfortunate site for traumatic events. Across the region, outbreaks of infection have occurred as a direct result of recent wars, compounded by food and water shortages, displacement, and damage to infrastructure and health services.[
Several initiatives highlighted the importance of improving health care in times of conflict. Nevertheless, not much has been done to integrate “conflict” as part of the core of medical education. Here, we call for action to advance medical education in war-ridden areas by incorporating “conflict medicine” in medical curricula.
CONFLICT-RELATED INJURIES: A RISING CHALLENGE
Conflict-related injuries can be varied and complex; resulting pathologies can be classified into war related and nonwar related. War-related illnesses include victims of blasts and burns, who present acutely, or those with chronic conditions like PTSD. This category also includes those affected by communicable diseases as a result of conflict and migration. Nonwar-related diseases include patients with noncommunicable diseases who have lost access to adequate health care and those who suffer the deterioration of health systems and facilities.[
CONFLICT MEDICINE: DEFINITION AND CURRENT STATUS
Conflict medicine is an area that specializes in delivering health care to conflict and war survivors and providing medical preparation, planning, response, and recovery throughout the conflict’s life cycle. Its specialists provide insight, guidance, and expertise on the principles and practice of medicine in the acute settings of the conflict zone. Unlike all other areas of specialization, the conflict medicine specialist only practices the full scope of the specialty in conflict-related emergencies.[
The current medical education systems in the Middle East guarantee that medical graduates, at best, are competent in reaching a diagnosis and planning a treatment. Nevertheless, there has not been enough emphasis on hands-on experiences, which can be imperative in times of war. Basic invasive skills such as suturing and placing intravenous lines are not mastered by the end of medical school. In addition, the over-reliance on advanced diagnostic tools decreases the physician’s effectiveness in acute situations and unequipped zones. Furthermore, the rigidity in following set guidelines and the inability to adjust guidelines as per presenting cases present a limitation.
Comprehensive care of patients in conflict requires coordination of medical, social, and public health sectors. Therefore, the development and integration of modules on conflict/disaster medicine in medical education must become a priority for medical schools and health-care centers in the region to better equip the medical personnel in the Middle East with skills and knowledge that can benefit their communities in times of need.
Lack of academia is another inadequacy that limits the transmission of knowledge onto the newer generations. Often, physicians who are mostly exposed to conflict-related injuries work in primary care centers and hospitals that are close to zones of conflict and thus are not academic, meaning they do not work in academic medical centers.[
EMBRACING CONFLICT MEDICINE
With the rising conflict-related challenges in the Middle East, embracing conflict medicine seems imminent to ensure the appropriate delivery of health care in acute settings and war zones. Medical schools in the Middle East by adopting or copying curricula present in developed countries lack the ingredients needed to address the new health challenges in such conflict-ridden societies. Although universal medicine ensures the learning of the basic principles of medicine, it does not target the needs of society. In addition, the lack of proper planning and governmental strategies to implement curricular changes and to address health needs exacerbates the problem.[
THE CONFLICT MEDICINE MODULE
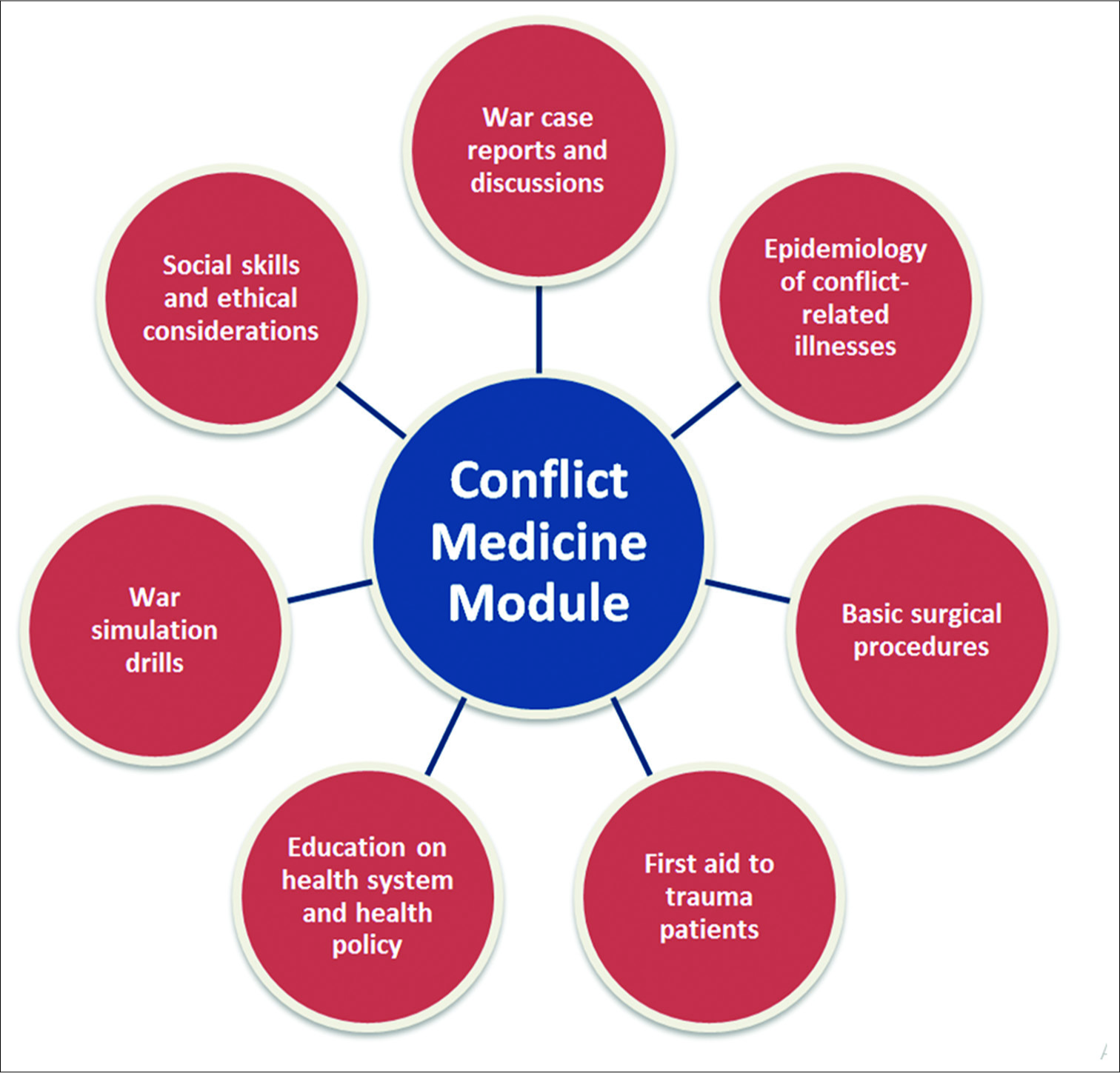
We propose that conflict medicine be included in the medical curricula of war-ridden countries as a module, which will emphasize the conceptualization of hands- on experiences [
IMPLEMENTATION AND EXPERIENCES OF MEDICAL SCHOOLS
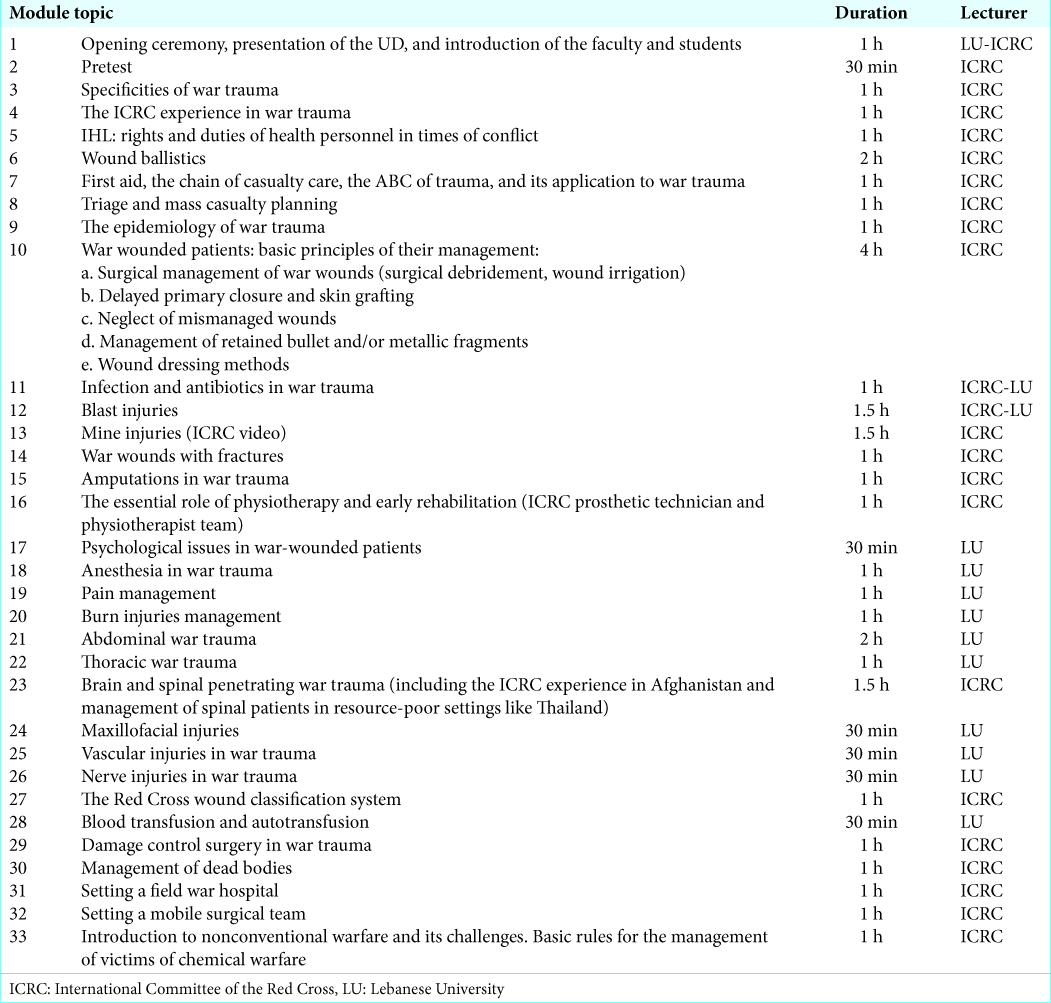
Implementing changes in medical curricula is not easy. This explains why few medical schools have adopted some form of disaster/conflict medicine training as part of their medical curriculum. In Lebanon, the Lebanese University (LU) Faculty of Medicine signed an agreement with the International Committee of the Red Cross to give a module on the clinical management of the war wounded [
CONCLUSION
Embracing conflict medicine seems imminent to ensure the appropriate delivery of health care in acute settings and war zones. We believe that investment in health care is crucial to provide cost-effective services to affected populations. Research is often forgotten in the rush to provide emergency care; nevertheless, publications from conflict settings provide better analyses of care provided to improve future care. Finally, intensifying diplomatic efforts to promote dialogue and avoid conflict and war remains the best method to prevent individual harm and societal damage.
References
1. Ayoub F, Fares Y, Fares J. The psychological attitude of patients toward health practitioners in Lebanon. N Am J Med Sci. 2015. 7: 452-8
2. Bajow N, Djalali A, Ingrassia PL, Ageely H, Bani I, Della Corte F. Proposal for a community-based disaster management curriculum for medical school undergraduates in Saudi Arabia. Am J Disaster Med. 2015. 10: 145-52
3. Bizri AR, Fares J, Musharrafieh U. Infectious diseases in the era of refugees: Hepatitis A outbreak in Lebanon. Avicenna J Med. 2018. 8: 147-52
4. Fares J, Fares Y. Cluster munitions: Military use and civilian health hazards. Bull World Health Organ. 2018. 96: 584-5
5. Fares J, Gebeily S, Saad M, Harati H, Nabha S, Said N. Post-traumatic stress disorder in adult victims of cluster munitions in Lebanon: A 10-year longitudinal study. BMJ Open. 2017. 7: e017214-
6. Fares J, Khachfe H, Fares M, Salhab H, Fares Y, Laher I.editors. Conflict medicine in the Arab world. Handbook of Healthcare in the Arab World. Cham: Springer; 2020. p.
7. Fares J, Salhab H, Fares M, Khachfe H, Fares Y, Laher I.editors. Academic medicine and the development of future leaders in healthcare. Handbook of Healthcare in the Arab World. Cham: Springer; 2020. p.
8. Fares Y, Ayoub F, Fares J, Khazim R, Khazim M, Gebeily S. Pain and neurological sequelae of cluster munitions on children and adolescents in South Lebanon. Neurol Sci. 2013. 34: 1971-6
9. Fares Y, El-Zaatari M, Fares J, Bedrosian N, Yared N. Trauma-related infections due to cluster munitions. J Infect Public Health. 2013. 6: 482-6
10. Fares Y, Fares J, Gebeily S. Head and facial injuries due to cluster munitions. Neurol Sci. 2014. 35: 905-10
11. Fares Y, Fares J, Kurdi MM, Bou Haidar MA. Physician leadership and hospital ranking: Expanding the role of neurosurgeons. Surg Neurol Int. 2018. 9: 199-
12. Fares Y, Fares J. Anatomical and neuropsychological effects of cluster munitions. Neurol Sci. 2013. 34: 2095-100
13. Fares Y, Fares J. Neurosurgery in Lebanon: History, development, and future challenges. World Neurosurg. 2017. 99: 524-32
14. Hoteit A, Fares J. Psycho-environmental tribulations arising from cluster munitions in South Lebanon. Sci Afric J Sci Issues Res Essays. 2014. 2: 469-73
15. Mheidly N, Fares J. Health communication research in the Arab world: A bibliometric analysis. Integr Healthc J. 2019. p.