- Department of Neurosurgery, Fann National University Hospital, Dakar, Senegal
- Neurosurgery Unit, Department of Surgery, Edward Francis Small Teaching Hospital (EFSTH), Banjul, The Gambia
Correspondence Address:
Ebrima Kalilu Manneh, Department of Surgery, Edward Francis Small Teaching Hospital, (EFSTH), Banjul, The Gambia.
DOI:10.25259/SNI_410_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fatou Sène1, Ebrima Kalilu Manneh1,2, Job Manneh2, Fansu F. N. Jatta2, Fatoumatta S. Jallow2, John Nute Jabang2. Meningiomas of the parieto-occipital convexity mimicking a hematoma: A case report in a third-world country. 04-Oct-2024;15:365
How to cite this URL: Fatou Sène1, Ebrima Kalilu Manneh1,2, Job Manneh2, Fansu F. N. Jatta2, Fatoumatta S. Jallow2, John Nute Jabang2. Meningiomas of the parieto-occipital convexity mimicking a hematoma: A case report in a third-world country. 04-Oct-2024;15:365. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13127
Abstract
Background: Meningiomas are benign, slow-growing tumors of the central nervous system (CNS) that arise from the arachnoid matter. It comprises one of the most common primary tumors of the CNS, occurring mostly in and after the fifth decade of life with a female gender predilection. Diagnosis is facilitated by imaging computed tomography (CT) or magnetic resonance imaging (MRI); however, atypical forms exist which augments the risk of missing the diagnosis. This is a case of a meningioma that mimics a hematoma on imaging, the diagnosis of which was only confirmed following histopathology.
Case Description: A 36-year-old patient presented with a 9-month history of intermittent moderate-intensity headaches associated with photophobia, tinnitus, and dizziness. There was no previous history of trauma. There were no focal neurological deficits on examination. Both contrast-enhanced and noncontrast-enhanced brain CT scans showed features suggestive of an intraparenchymal hematoma. She had a control CT scan 2 months and 9 months later due to the persistence of symptoms despite remaining stationary, which revealed no changes in the lesion as seen in the previous CT scans. The patient did not benefit from an MRI scan due to the socioeconomic status of the country and the patient herself. A decision to operate was made, and the sample was sent for histopathology. Histopathology confirmed the lesion to be a psammomatous meningioma.
Conclusion: Although CT findings of meningiomas are quite often typical, it is important to note that atypical forms exist as well. Knowledge of the atypical forms, such as lesions that look like an intraparenchymal hemorrhage initially but remain unchanged over a period of time, would decrease the risk of missing the diagnosis in such instances.
Keywords: Brain, Hemorrhage, Hematoma, Meningioma, Tomography
INTRODUCTION
Meningiomas are central nervous system (CNS) tumors, generally benign, arising from arachnoid cells located on the inner surface of the dura mater. They usually appear after the age of 50 and affect women predominantly with a sex ratio of 2:1.[
We hereby report a case of a meningioma with an atypical presentation on imaging, where we discuss the clinical presentation, imaging, and treatment of these tumors.
CASE DESCRIPTION
This is a 36-year-old female patient with no reported personal or family medical history. In February 2022, she was seen in the emergency department for headaches of moderate intensity lasting for 9 months, associated with photophobia, tinnitus, and dizziness. There was a notion of loss of consciousness which was not well documented. However, there was no reported history of vomiting, visual disturbances nor weakness of the limbs. There was no previous history of trauma. On examination, she had a Glasgow Coma Scale of 15/15, and her pupils were isochoric and reactive to light. There were no motor deficits, cranial nerve palsies, or sensory disturbances.
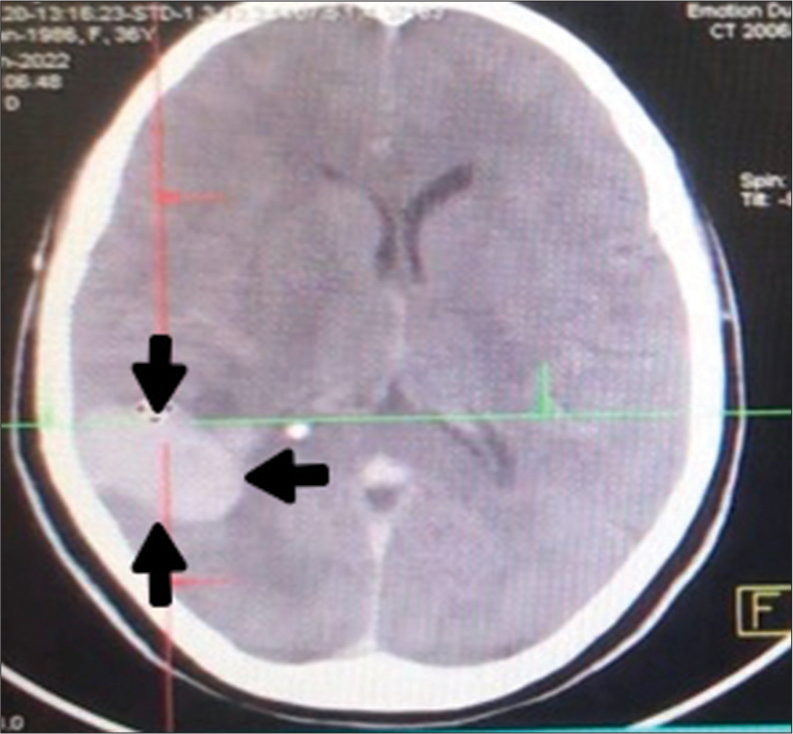
She came with a brain CT scan (both contrast enhanced and noncontrast enhanced) [
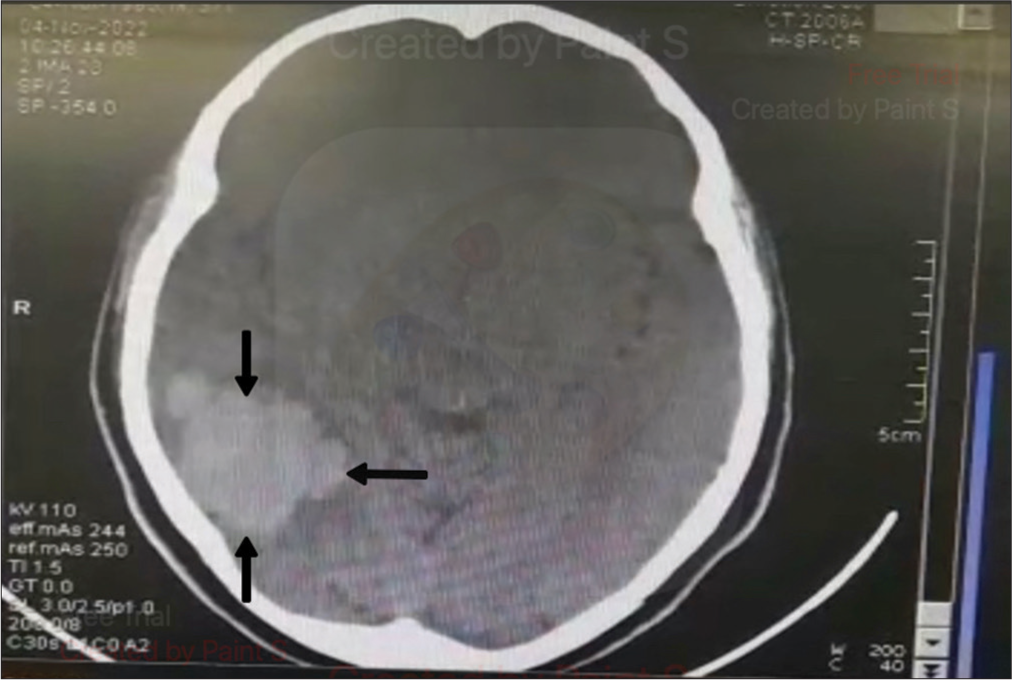
A control CT scan was done 2 months after the initial visit which showed the same lesion as seen earlier while the clinical picture remains static. Another CT scan was done seven months later [
The patient did not benefit from an MRI scan, which may have facilitated the diagnosis and, hence, the realization of an early excision for the following reasons: first, the country, being a third-world country, had only one MRI scanner and at the time had a breakdown and had been so for a little over a year. Second, the patient’s financial status did not allow her to be able to travel out of the country to do the MRI scan.
To the time of writing this article, there was only one Neurosurgeon in the entire country, this explains the irregular follow-up of the patient pre-operatively. This coupled with the fact that during the period of follow-up for this patient, he was also appointed as the head of the department for surgery, thereby complicating matters by increasing his engagements and hence decreasing his clinical work time.
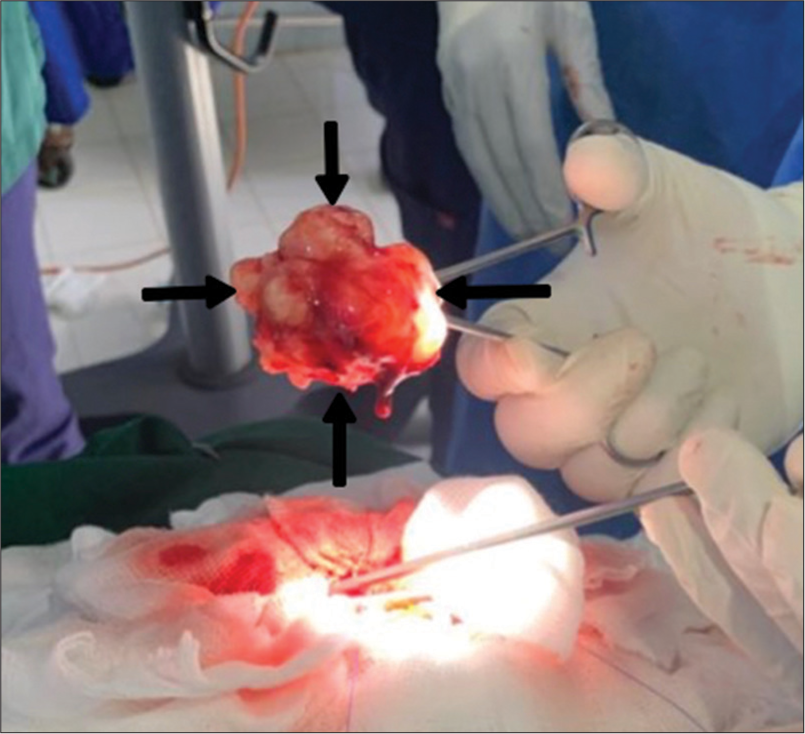
A right parieto-occipital craniotomy was realized, making it possible to perform a Simpson 1 excision. There were no intra-operative complications, the tumor was removed bloc, and the recovery from anesthesia was smooth. The lesion was pearly white, of firm consistency, hemorrhagic [
The postoperative course was unremarkable, with no neurological deficits, and the patient was placed on preventive antiepileptic and analgesic treatment. A postoperative contrast-enhanced CT scan was done and shown in
DISCUSSION
Meningiomas are classified into three grades with 15 subtypes according to the 5th edition of the WHO classification of tumors of the nervous system. These subtypes combine histological and molecular criteria (SMARCE1, BAP1, KLF4/TRAF7, and CDKN2A/B), making it possible to define the anaplastic or atypical character of meningiomas.[
Their incidence increases with age, with a median age of diagnosis estimated at 66 years.[
The diagnostic suspicion of meningiomas is most often high on the basis of characteristic imaging with a globular, homogeneous, circumscribed, well-enhanced mass of extra-axial location.[
However, even grade I meningiomas can present atypical imaging features such as hemorrhage, cyst, or metaplastic transformation that can be misleading.[
Our clinical case corresponds to a spontaneously hyperdense meningioma on CT, reminiscent of a hematoma, whose histopathology is in favor of a psammomatous meningioma. This benign histological subtype is rare, representing approximately 1.05–3.84% of all intracranial meningiomas.[
MRI combined with spectroscopy can help confirm the diagnosis by showing an alanine peak at 1.48 ppm specific for meningiomas and high contrast on perfusion imaging.[
Unfortunately, our patient did not benefit from an MRI, and this was one of the barriers to making an early diagnosis. In fact, a study looking at barriers to neurosurgical care of brain tumors in low- and middle-income countries showed delays in neuroimaging as well as a lack of advanced diagnostic facilities as some of the barriers.[
As for that which concerns the management of spontaneous supratentorial hematomas, evidence suggests no benefit of early evacuation of the hematoma through craniotomy as compared to conservative management pertaining to functional outcomes or mortality.[
However, in the case of a large hematoma, with mass effect and midline shift causing disturbances in the level of consciousness, then there is an indication for craniotomy and evacuation as a lifesaving procedure.[
Minimally invasive techniques for evacuation of hematomas were suggested by some studies to have prospects for better outcomes when compared to conservative management;[
As for infratentorial hematomas, where there is a high risk for brain stem compression, early evacuation is recommended, and indications include hematomas >3 cm, signs of brain stem compression, or evidence of hydrocephalus.[
The treatment of a meningioma is decided on a case-by-case basis and includes the following modalities: radio-clinical monitoring, surgical excision, conventional or stereotactic radiotherapy, and, more rarely, chemotherapy.[
Adjuvant radiotherapy is a treatment option for recurrent and inoperable tumors [
Chemotherapy has a limited role in the treatment of meningiomas both in Africa and at large; studies suggest no benefit of chemotherapy in the treatment of refractory or recurrent meningiomas.[
CONCLUSION
CT imaging of meningiomas is most often typical; however, less common features, such as a simple, spontaneous hyperdense appearance suggestive of hemorrhage, may be present and wrongly suggest another diagnosis. MRI, combined with spectroscopy, can help correct the diagnosis and avoid errors. However, in our context of developing countries where this examination is not always at hand, knowledge of these particular atypical imaging characteristics is necessary for any practitioner.
Ethical Approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Boetto J, Birzu C, Kalamarides M, Peyre M, Sanson M. Meningiomas: Update on current knowledge. Rev Med Interne. 2021. 43: 98-105
2. Brada GB, Ferszt R, Kendall BE, editors. Les méningiomes intracrâniens: Diagnostic - biologie - thérapeutique. Paris: Springer; 1991. p.
3. Corniola M, Lobrinus J, Lemée JM, Meling T. Intracranial meningiomas: Patient care in the neurosurgical era. Rev Med Suisse. 2020. 16: 283-8
4. Damalcheruvu PR, Mian M, Sharma S, Patro S, Vattoth S, Viswamitra S. Meningioma or mimic: Look twice and save a life. Neurographics. 2022. 12: 216-32
5. Dastur CK, Yu W. Current management of spontaneous intracerebral haemorrhage. Stroke Vasc Neurol. 2017. 2: 21-9
6. De Oliveira Manoel AL. Surgery for spontaneous intracerebral hemorrhage. Crit Care. 2020. 24: 45
7. Drappatz J. How useful is chemotherapy for atypical and anaplastic meningiomas?. Expert Opin Pharmacother. 2022. 23: 1559-61
8. Fiagbedzi E, Hasford F, Tagoe S, Nisbet A. Radiotherapy infrastructure for brain metastasis treatment in Africa: Practical guildelines for implementation of a stereotactic radiosurgery (SRS) program. Health Technol (Berl). 2023. 13: 893-904
9. Kominami S, Watanabe A, Suzuki M, Mizunari T, Kobayashi S, Teramoto A. Preoperative embolization of meningiomas with N-butyl cyanoacrylate. Interv Neuroradiol. 2012. 18: 133-9
10. Kyritsis AP. Chemotherapy for meningiomas. J Neurooncol. 1996. 29: 269-72
11. Lin Z, Zhao M, Ren X, Wang J, Li Z, Chen X. Clinical features, radiologic findings, and surgical outcomes of 65 intracranial psammomatous meningiomas. World Neurosurg. 2017. 100: 395-406
12. Mezue W, Ndubuisi C, Ohaegbulam S, Achebe D, Chikani M. Management of intracranial meningiomas in Enugu, Nigeria. Surg Neurol Int. 2012. 3: 110
13. N’Dri Oka D, Broalet Maman YE, Kakou M, Broalet P, Haidara A, Boni N’guessan R. Intracranial meningiomas in the ivorian environment: Study of a surgical series. Afr J Neurol Sci. 2008. 27: 31-5
14. Ogasawara C, Philbrick BD, Adamson DC. Meningioma: A review of epidemiology, pathology, diagnosis, treatment, and future directions. Biomedicines. 2021. 9: 319
15. Raman SG, Prakash P, Sumit J, Bikram SD, Prasanna K. Clinical outcome and recurrence after meningioma surgery: An experience from a developing country, Nepal. World Neurosurg. 2021. 148: e138-44
16. Shah A, Choudhri O, Jung H, Li G. Preoperative endovascular embolization of meningiomas: Update on therapeutic options. Neurosurg Focus. 2015. 38: E7
17. Shahbandi A, Shah DS, Hadley CC, Patel AJ. The role of pharmacotherapy in treatment of meningioma: A systematic review. Cancers (Basel). 2023. 15: 483
18. Shakir M, Shariq SF, Irshad HA, Khowaja AH, Tahir I, Rae AI. Barriers to neurosurgical care of brain tumors in low-and middle-income countries: A systematic review of the service delivery challenges. World Neurosurg. 2024. 187: 211-22.e3