- Department of Neurosurgery, Iwate Prefectural Chubu Hospital, Kitakami, Iwate, Japan
Correspondence Address:
Hiroshi Kashimura
Department of Neurosurgery, Iwate Prefectural Chubu Hospital, Kitakami, Iwate, Japan
DOI:10.4103/2152-7806.158515
Copyright: © 2015 Takeda M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Takeda M, Kashimura H, Chida K, Murakami T. Microsurgical clipping for the true posterior communicating artery aneurysm in the distal portion of the posterior communicating artery. Surg Neurol Int 10-Jun-2015;6:101
How to cite this URL: Takeda M, Kashimura H, Chida K, Murakami T. Microsurgical clipping for the true posterior communicating artery aneurysm in the distal portion of the posterior communicating artery. Surg Neurol Int 10-Jun-2015;6:101. Available from: http://surgicalneurologyint.com/surgicalint_articles/microsurgical-clipping-true-posterior-communicating-artery/
Abstract
Background:Aneurysms arising from the posterior communicating artery (PCoA) itself are rare in which aneurysms usually located in the proximal portion of the PCoA. The authors report a case of the true PCoA ruptured aneurysm in the distal portion of the PCoA.
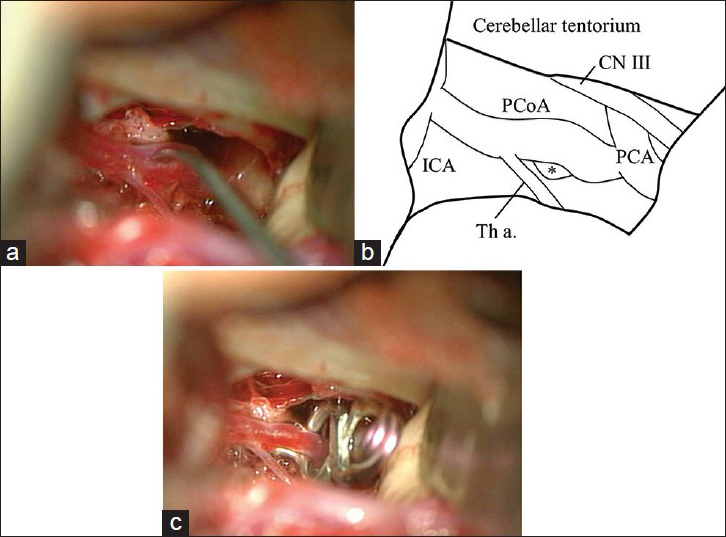
Case Description:The patient was an 83-year-old man who suffered subarachnoid hemorrhage. Cerebral angiography revealed a saccular aneurysm arising on the fetal type right PCoA itself in the distal portion of the PCoA. 2 days after the onset of symptoms, the patient underwent right interfascial pterional craniotomy, with anterior temporal approach. The aneurysm was successfully clipped with the preservation of both the PCoA and the thalamoperforating artery.
Conclusion:We speculated that blood flow into the PCoA gradually increased after occlusion of the left vertebral artery, which induced tortuosity of the PCoA. As a result, hemodynamic stress might increase near the curvature and cause aneurysm formation.
Keywords: Anterior temporal approach, microsurgical clipping, true posterior communicating artery aneurysm
INTRODUCTION
The true posterior communicating artery (PCoA) aneurysms can be defined as aneurysms, which arise from the PCoA itself and are attached to neither the internal carotid nor the posterior cerebral artery (PCA). Aneurysms usually located within a few millimeters from the carotid artery. Among the true PCoA, the aneurysms in the distal portion of the PCoA were rare.[
CASE REPORT
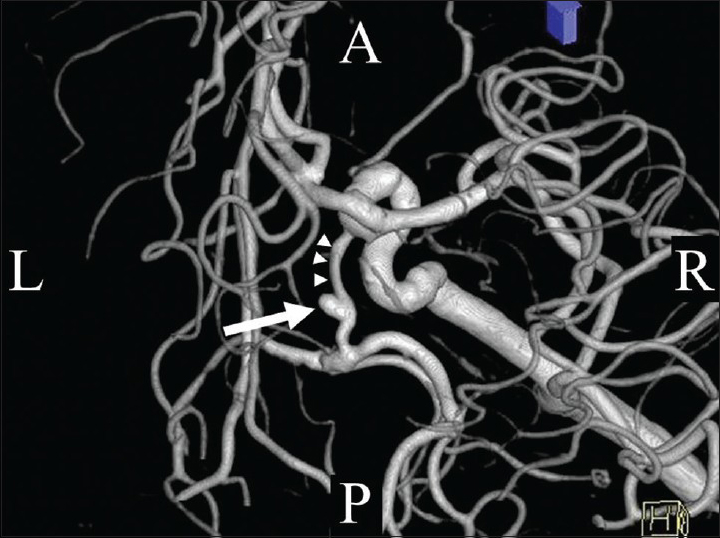
An 83-year-old man suffered severe headache and subsequent loss of consciousness and was admitted to our hospital. There was no focal neurological abnormality. Initial computed tomography (CT) showed typical findings of subarachnoid hemorrhage in the basal cistern. Three-dimensional digital subtraction angiography revealed a saccular aneurysm arising on the right PCoA itself in the distal portion of the PCoA [
Two days after the onset of symptoms, the patient underwent right interfascial pterional craniotomy in the manner described by Yasargil et al., with anterior temporal approach.[
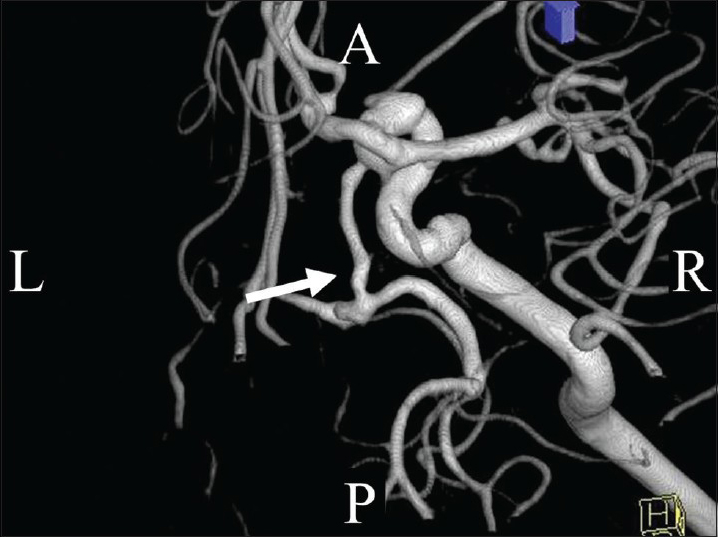
Postoperatively, the patient experienced no cerebral ischemic events. Follow-up cerebral angiography 23 days after the operation showed disappearance of the aneurysm [
DISCUSSION
The true PCoA aneurysms are among the rarest intracranial aneurysms. Although scant, the literature suggests that these aneurysms comprise between 0.1% and 3.6% of all aneurysms and ~4.6% and 13.0%, of all PCoA aneurysms.[
It has been generally considered that hemodynamic factor plays an important role in the formation, the growth, and the rupture of the cerebral aneurysm.[
In treating these aneurysms, it is critical to preserve the patency of both the PCoA and the thalamoperforating arteries arising from it. The aneurysms in the proximal portion of the PCoA were easily visualized and clipped by using a standard pterional approach, because the aneurismal fundus projects to the laterally within the carotid cistern and most of the aneurysms are unrelated to perforating arteries.[
References
1. Abiko S, Orita T. A case of “true” posterior communicating artery aneurysm (author's transl). No Shinkei Geka. 1981. 9: 1181-5
2. Burleson AC, Strother CM, Turitto VT. Computer modeling of intracranial saccular and lateral aneurysms for the study of their hemodynamics. Neurosurgery. 1995. 37: 774-82
3. Hashimoto N, Handa H, Nagata I, Hazama F. Experimentally induced cerebral aneurysms in rats: Part V. Relation of hemodynamics in the circle of Willis to formation of aneurysms. Surg Neurol. 1980. 13: 41-5
4. He W, Hauptman J, Pasupuleti L, Setton A, Farrow MG, Kasper L. True posterior communicating artery aneurysms: Are they more prone to rupture? A biomorphometric analysis. J Neurosurg. 2010. 112: 611-5
5. Heros RC, Lee SH. The combined pterional/anterior temporal approach for aneurysms of the upper basilar complex: Technical report. Neurosurgery. 1993. 33: 244-50
6. Kondo S, Hashimoto N, Kikuchi H, Hazama F, Nagata I, Kataoka H. Cerebral aneurysms arising at nonbranching sites. An experimental Study. Stroke. 1997. 28: 398-403
7. Krayenbühl HA, Yasargil MG, Flamm ES, Tew JM. Microsurgical treatment of intracranial saccular aneurysms. J Neurosurg. 1972. 37: 678-86
8. Muneda K, Yoshizu H, Terada H. True posterior communicating artery aneurysm. No Shinkei Geka. 2001. 29: 163-8
9. Nakano Y, Saito T, Yamamoto J, Takahashi M, Akiba D, Kitagawa T. Surgical treatment for a ruptured true posterior communicating artery aneurysm arising on the fetal-type posterior communicating artery: Two case reports and review of the literature. J UOEH. 2011. 33: 303-12
10. Nakatani H, Hashimoto N, Kang Y, Yamazoe N, Kikuchi H, Yamaguchi S. Cerebral blood flow patterns at major vessel bifurcations and aneurysms in rats. J Neurosurg. 1991. 74: 258-62
11. Ogasawara K, Numagami Y, Kitahara M. A case of ruptured true posterior communicating artery aneurysm thirteen years after surgical occlusion of the ipsilateral cervical internal carotid artery. No Shinkei Geka. 1995. 23: 359-63
12. Takahashi A, Kamiyama H, Houkin K, Abe H, Nomura M. Anterior temporal approach as a modification of extended trans-sylvian approach. Surg Cereb Stroke. 1994. 22: 307-10
13. Takahashi A, Kamiyama H, Imamura H, Kitagawa M, Abe H. True posterior communicating artery aneurysm - Report of two cases. Neurol Med Chir (Tokyo). 1992. 32: 338-41
14. Tanikawa R, Wada H, Ishizaki T, Izumi N, Fujita T, Hashimoto M. Anterior temporal approach for basilar bifurcation aneurysms as a modified distal transsylvian approach. Surg Cereb Stroke. 1998. 26: 259-64
15. Timothy J, Sharr M, Doshi B. Perils of a ‘true’ posterior communicating artery aneurysm. Br J Neurosurg. 1995. 9: 789-91
16. Tognetti F, Limoni P, Testa C. Aneurysm growth and hemodynamic stress. Surg Neurol. 1983. 20: 74-8
17. Yasargil MG, Reichman MV, Kubik S. Preservation of the frontotemporal branch of the facial nerve using the interfascial temporalis flap for pterional craniotomy. Technical article. J Neurosurg. 1987. 67: 463-6
18. Yasargil MG, Smith RD, Youmans JR.editors. Management of aneurysms of anterior circulation by intracranial procedures. Neurological Surgery. Philadelphia: Saunders; 1982. 3: 1663-96