- Department of Neurosurgery, University of Tsukuba,
- Department of Neurosurgery, Tsukuba Memorial Hospital, Tsukuba, Japan.
Correspondence Address:
Eiichi Ishikawa, Department of Neurosurgery, University of Tsukuba, Tsukuba, Japan.
DOI:10.25259/SNI_112_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Atsushi Tsukada1, Kiyoyuki Yanaka2, Eiichi Ishikawa1. Midbrain hemorrhage presenting with isolated downward gaze palsy: A case report. 07-Apr-2023;14:132
How to cite this URL: Atsushi Tsukada1, Kiyoyuki Yanaka2, Eiichi Ishikawa1. Midbrain hemorrhage presenting with isolated downward gaze palsy: A case report. 07-Apr-2023;14:132. Available from: https://surgicalneurologyint.com/surgicalint-articles/12237/
Abstract
Background: Diseases presenting with only downward gaze palsy are extremely rare particular in cerebral hemorrhage.
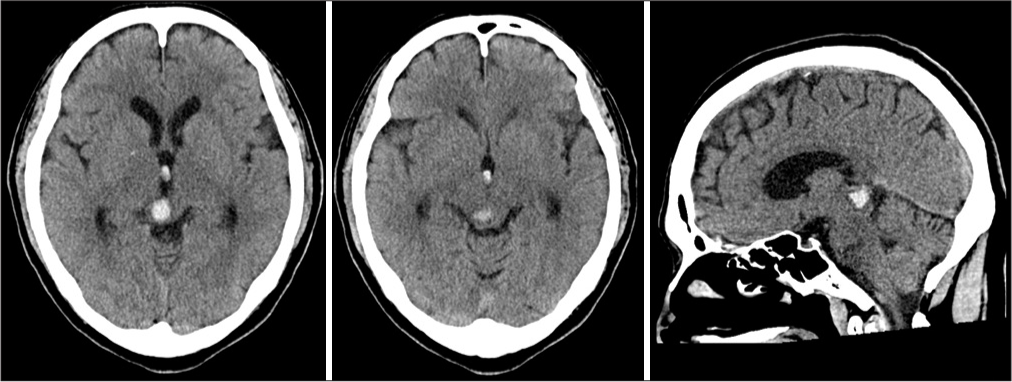
Case Description: A 63-year-old man with no medical history developed a downward-dominant vertical gaze paralysis with a convergence disorder. Computed tomography and magnetic resonance imaging showed a small hemorrhage of 13 mm in diameter in the right midbrain tegmental area. The patient was conservatively treated. His symptoms showed a gradual improvement from upward gaze paralysis and convergence disorder followed by downward gaze paralysis. All symptoms disappeared in 3 weeks after the onset. The center of vertical eye movement was thought to be the rostral interstitial nucleus of medial longitudinal fasciculus (riMLF) and posterior commissure (PC).
Conclusion: In this case, bilateral riMLF and PC were impaired, resulting in bilateral vertical ocular motility disorder with upward gaze paralysis. Brainstem hemorrhage rarely presents with vertical gaze palsy. Most are cerebral infarctions, and few are due to cerebral hemorrhage. This case was important for better understanding the pathophysiology of an ocular motility disorder. We also summarized the characteristics of isolated vertical gaze palsy caused by cerebral hemorrhage.
Keywords: Downward gaze palsy, Midbrain hemorrhage, Posterior commissure, Rostral interstitial nucleus of medial longitudinal fasciculus (riMLF)
INTRODUCTION
Diseases presenting with vertical gaze palsy are rare and occur with vascular disorders or tumors in the dorsal midbrain.[
CASE DESCRIPTION
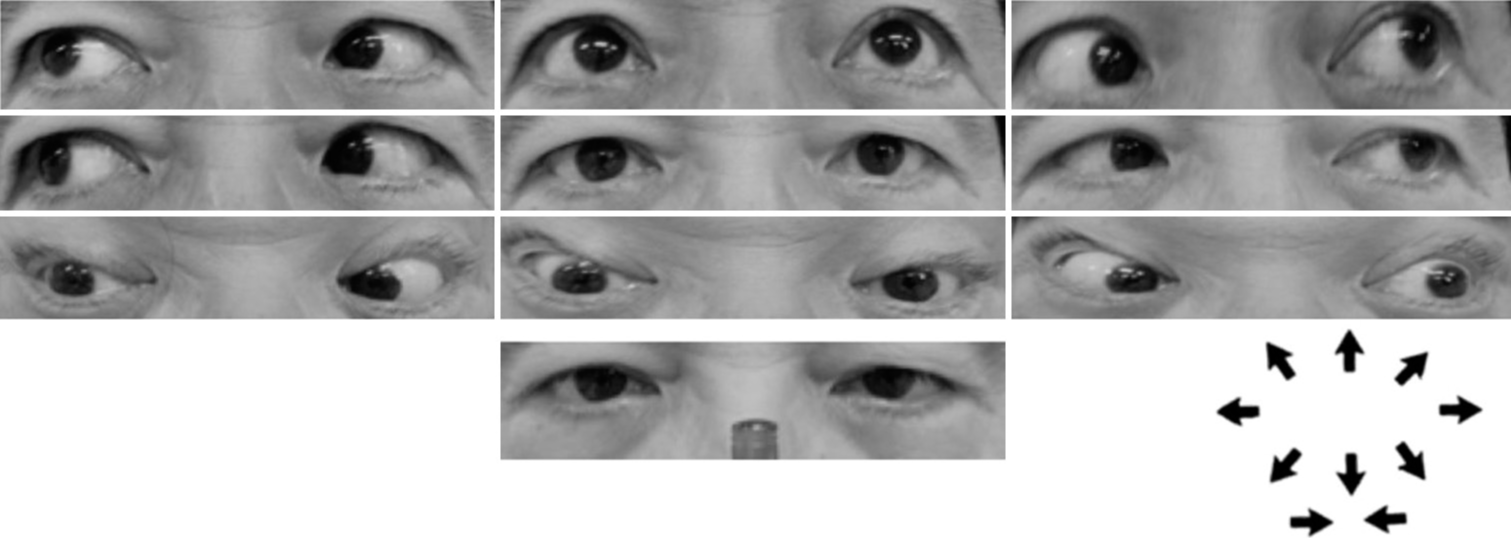
A 63-year-old man referred to our hospital with a sudden onset of generalized headache and diplopia that worsened in all directions, especially looking downward. On admission, there were no abnormalities in vital signs and blood tests. Neurological findings showed clear consciousness. Vertical gaze palsy, convergence disorder, bilateral light reflex loss, and diplopia, which worsened with downward gaze, were observed. Horizontal eye movements were maintained [
Figure 3:
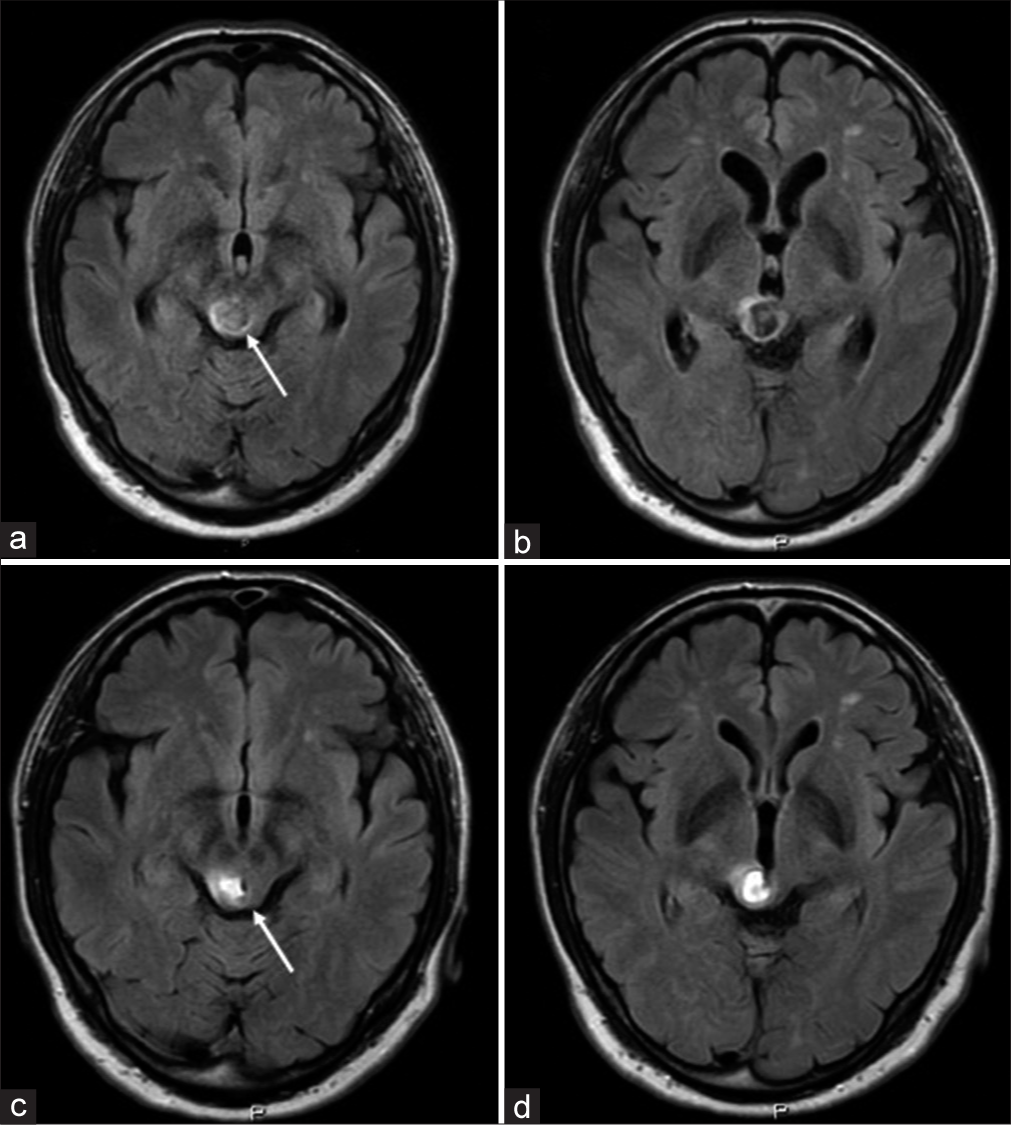
Time course of magnetic resonance imaging ([a and b] on admission [c and d] after 11 days). (a and c) are slice of the level of pineal gland, and (b and c) are slice of the upper level of pineal gland. The hematoma remained in the right cover and the edematous change of the posterior commissure disappeared (arrow).
DISCUSSION
This is an extremely rare case of vertical gaze palsy presenting with isolated downward gaze palsy due to cerebral hemorrhage. We considered the mechanism.
The center of vertical eye movement is said to be associated with the rostral interstitial nucleus of medial longitudinal fasciculus (riMLF), the Cajal nucleus, the PC, and the Darkschewitsch nucleus.[
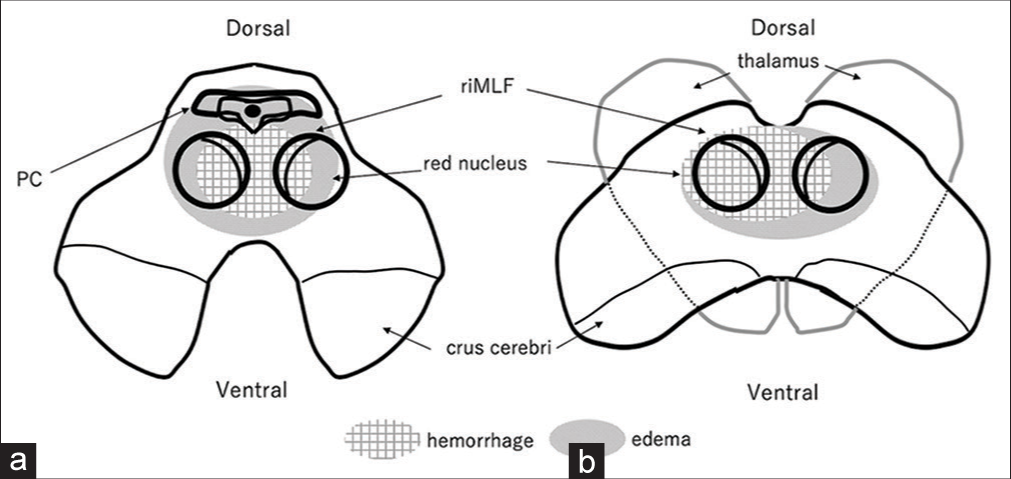
To satisfy these conditions, the lesion must be extremely localized toward the midline, so it is extremely rare for downward gaze paralysis to appear alone. In this case, the main locus of hemorrhage was in the right midbrain tegmentum, right riMLF, and edematous changes extended to the PC and contralateral riMLF. In the downward direction, it was thought that the edematous change partially extended to the vicinity of the dorsolateral oculomotor nucleus, which is considered to be the center of convergence. It is presumed that the upper gaze palsy was associated with the PC, and the lower gaze palsy was associated with dysfunction associated with bilateral riMLF and dorsolateral oculomotor nuclei due to hemorrhage and edematous changes [
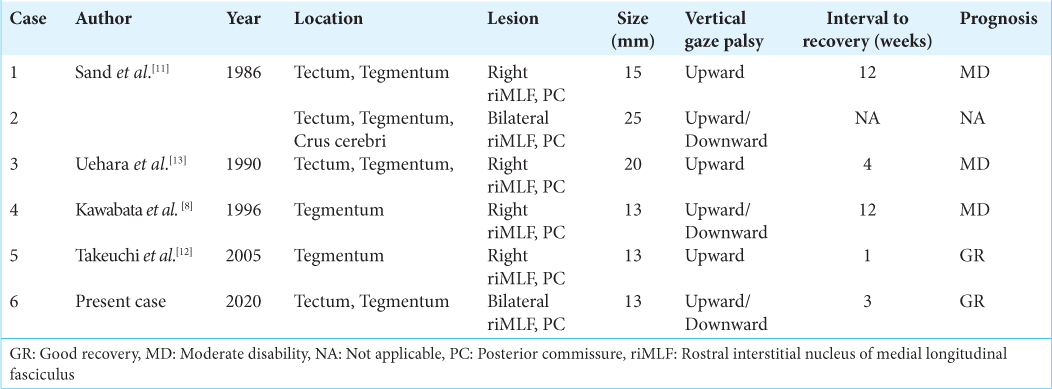
Most of the cerebrovascular diseases that cause vertical gaze palsy are caused by cerebral infarction, and cerebral hemorrhage has so far occurred in only six cases, including this case [
CONCLUSION
We report a case of cerebral hemorrhage in the midbrain tegmentum presenting with isolated downward gaze paralysis. Anatomically, the bilateral riMLF and the PC were presumed to have been disturbed to the right, and this case contributed to the understanding of oculomotor disorders. We also investigated the characteristics of vertical eye movement disorders caused by cerebral hemorrhage.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bender MB. Brain control of conjugate horizontal and vertical eye movements. A survey of the structural and functional correlates. Brain. 1980. 103: 23-69
2. Bender MB. Comments the physiology and pathology of eye movements in the vertical plane. J Nerv Ment Dis. 1960. 130: 456-66
3. Bhidayasiri R, Plant GT, Leigh RJ. A hypothetical scheme for the brainstem control of vertical gaze. Neurology. 2000. 54: 1985-93
4. Bogousslavsky J, Miklossy J, Regli F, Janzer R. Vertical gaze palsy and selective unilateral infarction of the rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF). J Neurol Neurosurg Psychiatry. 1990. 53: 67-71
5. Buttner-Ennever JA, Buttner U, Cohen B, Baumgartner G. Vertical gaze paralysis and the rostral interstitial nucleus of the medial longtitudinal fasciculus. Brain. 1982. 105: 125-49
6. Goto F, Amano T, editors. Rinsho Notameno Shinkeikinoukaibougaku (Japanese). Singapore: Chugaiigakusya; 1992. p. 14-15
7. Hommel M, Bogousslavsky J. The spectrum of vertical gaze palsy following unilateral brainstem stroke. Neurology. 1991. 41: 1229-34
8. Kawabata K, Tanaka T. Vertical gaze palsy with a unilateral vascular lesion of the midbrain-in relation to the rostral interstitial nucleus of medial longitudinal fasciculus. J Stroke. 1996. 18: 135-42
9. Nakajima T, Nishimura H, Ukita T, Tsuji M, Miyake H, Ohmura T. A case of midbrain infarction with selective bilateral downward gaze palsy. J Stroke. 2009. 31: 317-21
10. Pierrot-Deseilligny CH, Chain F, Gray F, Serdaru M, Escourolle R. Parinaud’s syndrome; Electro-oculographic and anatomical analyses of six vascular cases with deductions about vertical gaze organization in the premotor structures. Brain. 1982. 105: 667-96
11. Sand JJ, Biller J, Corbett JJ. Partial dorsal mesencephalic hemorrhages. Report of three cases. Neurology. 1986. 36: 529-33
12. Takeuchi S, Kawaguchi T, Nakatami M, Ootani N, Ishihara H, Uozumi Y. Bilateral ptosis and upper gaze palsy with pupil sparing caused by midbrain hemorrhage. Brain Nerv. 2005. 57: 899-901
13. Uehara H, Nakano S, Maruoka ZN, Wakisaka S, Kinoshita K. A case of internal carotid artery defect caused by intracranial hemorrhage. No Shinkei Geka. 1990. 18: 77-81