- Department of Neurosurgery, Kushiro Rosai Hospital, Kushiro, Hokkaido, Japan.
- Department of Neurosurgery, Nippon Medical School, Chiba Hokuso Hospital, Inzai, Chiba, Japan.
Correspondence Address:
Juntaro Matsumoto
Department of Neurosurgery, Kushiro Rosai Hospital, Kushiro, Hokkaido, Japan.
DOI:10.25259/SNI_167_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Juntaro Matsumoto1, Toyohiko Isu1, Kyongsong Kim2, Koichi Miki1, Masanori Isobe1. Middle cluneal nerve entrapment neuropathy attributable to lumbar disc herniation. 30-Mar-2021;12:132
How to cite this URL: Juntaro Matsumoto1, Toyohiko Isu1, Kyongsong Kim2, Koichi Miki1, Masanori Isobe1. Middle cluneal nerve entrapment neuropathy attributable to lumbar disc herniation. 30-Mar-2021;12:132. Available from: https://surgicalneurologyint.com/surgicalint-articles/10677/
Abstract
Background: Middle cluneal nerve entrapment neuropathy (MCN-EN) is a known cause of low back pain (LBP). Here, we succeeded in treating a patient with a lumbar disc herniation who actually had MCN-EN with a nerve block and neurolysis.
Case Description: A 52-year-old female presented with severe left lower back and lateral thigh pain making it difficult to walk. The lumbar MRI revealed a disc herniation on the left at the L5/S1 level. On palpation, we identified a trigger point on the buttock where the MCN penetrates the long posterior sacroiliac ligament between the posterior superior and inferior iliac spine. Two left-sided MCN blocks, followed by the left MCN neurolysis procedure, were performed under local anesthesia. At the last follow-up, 10 months after surgery, the LBP has not recurred, and she requires no medications for pain control.
Conclusion: Here, a patient with a left-sided L5S1 disc herniation and low back/leg pain was successfully treated for MCN-EN with nerve block followed by neurolysis.
Keywords: Lumbar disc herniation, Middle cluneal nerve, Mimic
INTRODUCTION
Superior cluneal nerve entrapment neuropathy (SCN-EN) and middle cluneal nerve entrapment neuropathy (MCN-EN) are a known cause of low back pain; its’ etiology remains unknown (LBP).[
Etiology of MCN-EN
The etiologies of MCN-EN and SCN-EN[
CASE DESCRIPTION
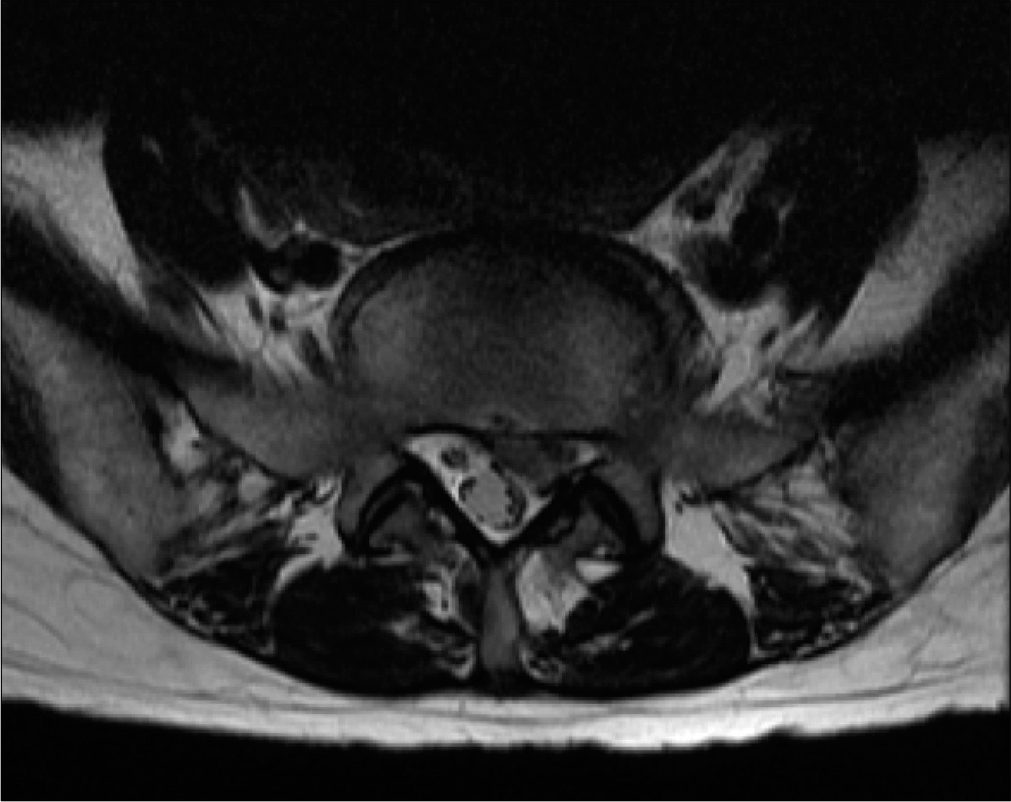
A 52-year-old female suddenly presented with the 5-day onset of the left-sided low back and left thigh pain without any focal neurological deficits. Her pain rated by multiple scoring systems (e.g., numerical rating scale [NRS] of 9, her Roland-Morris Disability Questionnaire [RDQ] score of 21, and her Japanese Orthopedic Association [JOA] score of 8). Lumbar X-rays were unremarkable, while the MR revealed a disc herniation on the left at L5/S1 level [
Treatment with nerve blocks
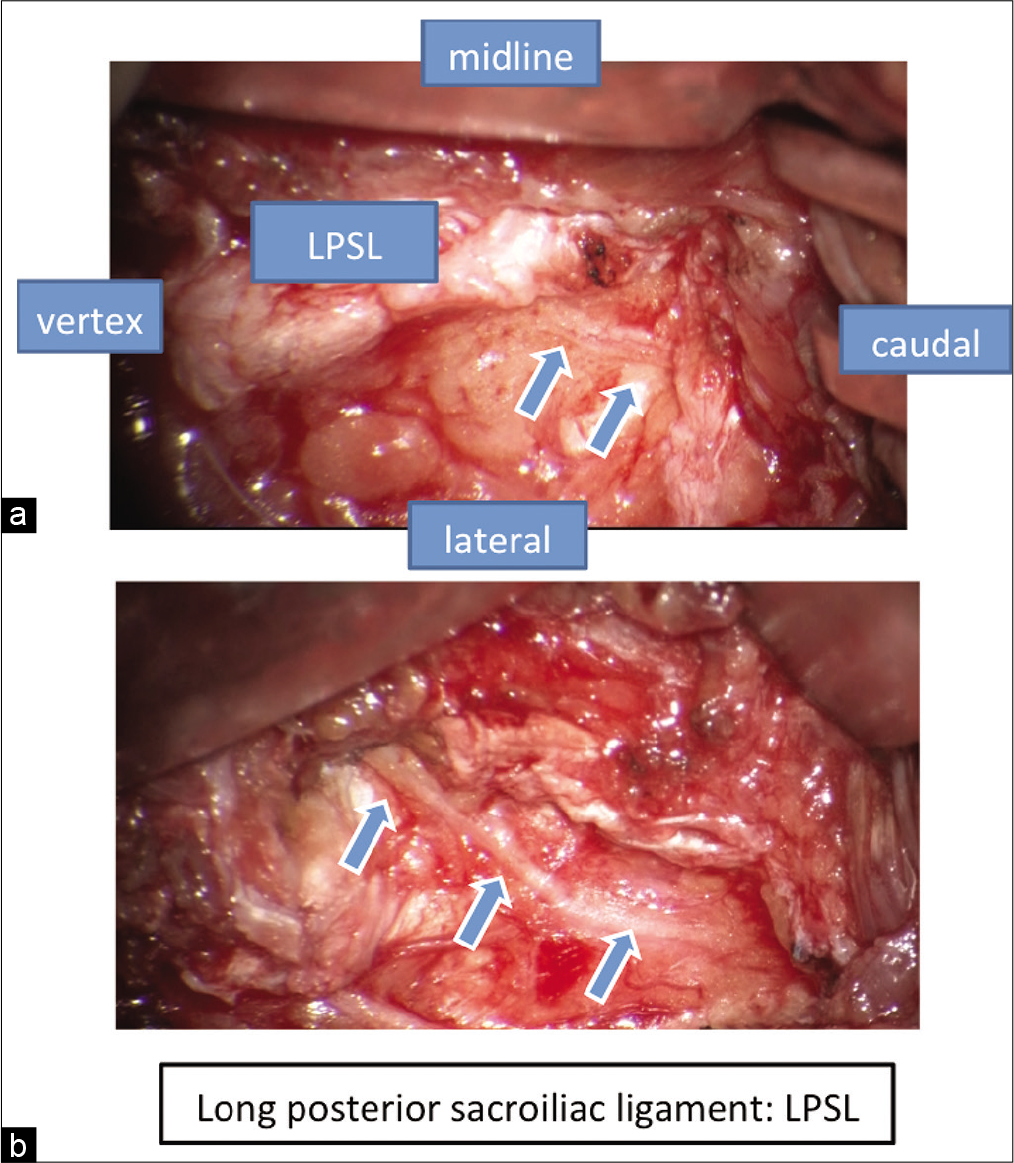
Palpation identified a trigger point located 35 mm caudal to the posterior superior iliac spine (PSIS) at a site slightly lateral at the edge of the iliac crest. This local suggested MCN-EN as the MCN penetrates the LPSL between the PSIS (define) and the posterior inferior iliac spine (PIIS define). A MCN block was performed utilizing 0.75% ropivacaine (2 ml); the pain was transiently relieved (NRS = 1). She was diagnosed with a MCN-EN associated with the lumbar disc herniation. A second MCN block (PERFORMED WHEN?) yielded pain control, and she was discharged 12 days later.
Recurrent symptoms
Thirty days postdischarge, her symptoms gradually reappeared and exacerbated. She subsequently underwent a left MCN neurolysis under local anesthesia; a 6 cm linear incision performed under the surgical microscope, allowed the distal portion of the MCN to be exposed after splitting the GMaM and opening the GMaM fascia (SPELL OUT). LPSL penetration of the MCN was confirmed, and the MCN was decompressed by incising the LPSL [
Postoperative course
Postoperatively, her pain was alleviated, and she immediately returned to work. Although the MRI demonstrated an increasing lumbar disc herniation, she was able to be treated conservatively. Ten months later, her LBP had not recurred, and she required no medication (NRS 0, RDQ score 0, and JOA score 28).
DISCUSSION
MCN-EN: Pure sensory nerve branch
The SCN and MCN are pure sensory nerve branches that arise from the dorsal rami of the spinal nerve roots. The SCN originates from the lower thoracic and lumbar posterior nerve roots; its’ entrapment around the iliac crest can elicit LBP.[
Entrapment of the MCN
Entrapment of the MCN, a nerve that originates at S1–S4, between the PSIS define and the PIIS define by the LPSL, can also result in LBP.[
Diagnosis of MCN-EN shorten use tables
The diagnoses of MCN-EN and SCN-EN are based on the clinical presentations and the ability to reduce pain utilizing MCN blocks.[
CONCLUSION
We report that MCN-EN treatment with initial nerve block followed by neurolysis resulted in sufficient alleviation of LBP to avoid lumbar disc surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aota Y. Entrapment of middle cluneal nerves as an unknown cause of low back pain. World J Orthop. 2016. 7: 67-170
2. Chiba Y, Isu T, Kim K, Iwamoto N, Morimoto D, Yamazaki K. Association between intermittent low-back pain and superior cluneal nerve entrapment neuropathy. J Neurosurg Spine. 2015. 13: 1-5
3. Isu T, Kim K, Morimoto D, Iwamoto N. Superior and middle cluneal nerve entrapment as a cause of low back pain. Neurospine. 2018. 15: 25-32
4. Iwamoto N, Isu T, Kim K, Chiba Y, Kokubo R, Morimoto D. Low back pain caused by superior cluneal nerve entrapment neuropathy in patients with Parkinson disease. World Neurosurg. 2016. 87: 250-4
5. Iwamoto N, Isu T, Kim K, Chiba Y, Morimoto 4D, Matsumoto J. Treatment of low back pain elicited by superior cluneal nerve entrapment neuropathy after lumbar fusion surgery. Spine Surg Rel Res. 2017. 1: 152-7
6. Kim K, Isu T, Chiba Y, Iwamoto N, Yamazaki K, Morimoto D. Treatment of low back pain in patients with vertebral compression fractures and superior cluneal nerve entrapment neuropathies. Surg Neurol Int. 2015. 6: S619-21
7. Kim K, Isu T, Matsumoto J, Yamazaki K, Isobe M. Low back pain due to middle cluneal nerve entrapment neuropathy. Eur Spine J. 2017. 27: 309-13
8. Kim K, Shimizu J, Isu T, Inoue K, Chiba Y, Iwamoto N. Low back pain due to superior cluneal nerve entrapment-Clinicopathological study. Muscle Nerve. 2018. 57: 777-83
9. Konno T, Aota Y, Kuniya H, Saito T, Qu N, Hayashi S. Anatomical etiology of “pseudo-sciatica” from superior cluneal nerve entrapment: A laboratory investigation. J Pain Res. 2017. 10: 2539-45
10. Konno T, Aota Y, Saito T, Qu N, Hayashi S, Kawata S. Anatomical study of middle cluneal nerve entrapment. J Pain Res. 2017. 10: 1431-5
11. Kuniya H, Aota Y, Kawai T, Kaneko KI, Konno T, Saito T. Prospective study of superior cluneal nerve disorder as a potential cause of low back pain and leg symptoms. J Orthop Surg Res. 2014. 9: 139
12. Matsumoto J, Isu T, Kim K, Iwamoto N, Morimoto D, Isobe M. Surgical treatment of middle cluneal nerve entrapment neuropathy technical note. J Neurosurg Spine. 2018. 29: 208-13
13. Morimoto D, Isu T, Kim K, Chiba Y, Iwamoto N, Isobe M. Long-term Outcome of Surgical Treatment for Superior Cluneal Nerve Entrapment Neuropathy. Spine. 2017. 42: 783-8
14. Strong EK, Davila JC. The cluneal nerve syndrome: A distinct type of low back pain. Ind Med Surg. 1957. 26: 417-29







KTR
Posted April 4, 2021, 1:13 pm
Interesting case. Thank you for sharing this.