- Department of Neurosurgery, Kansai Rosai Hospital, Hyogo, Japan.
Correspondence Address:
Shingo Toyota, Department of Neurosurgery, Kansai Rosai Hospital, Hyogo, Japan.
DOI:10.25259/SNI_1272_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tomoaki Murakami, Shingo Toyota, Kanji Nakagawa, Tatsuya Hagioka, Yuhei Hoshikuma, Takuya Suematsu, Takeshi Shimizu, Maki Kobayashi, Takuyu Taki. Midline suboccipital approach to a vertebral artery–posterior inferior cerebellar artery aneurysm from the rostral end of the patient using ORBEYE. 11-Mar-2022;13:87
How to cite this URL: Tomoaki Murakami, Shingo Toyota, Kanji Nakagawa, Tatsuya Hagioka, Yuhei Hoshikuma, Takuya Suematsu, Takeshi Shimizu, Maki Kobayashi, Takuyu Taki. Midline suboccipital approach to a vertebral artery–posterior inferior cerebellar artery aneurysm from the rostral end of the patient using ORBEYE. 11-Mar-2022;13:87. Available from: https://surgicalneurologyint.com/surgicalint-articles/11435/
Abstract
Background: The midline suboccipital approach with the patient in the prone position is safe and effective for clipping vertebral artery–posterior inferior cerebellar artery (VA–PICA) aneurysms. Using a conventional surgical microscope from the rostral end of the patient for this approach without an extreme head-down position requires the surgeon to overhang the visual axis of the microscope and perform surgical manipulations in an uncomfortable posture. We report performing the midline suboccipital approach from the rostral end with slight head-down position using ORBEYE, a new high-definition (4K) three-dimensional exoscope.
Case Description: A 65-year-old woman was admitted for clipping of a right unruptured VA–PICA aneurysm (maximum diameter, 5mm) located medially and ventral to the hypoglossal canal. After induction of general anesthesia, the patient was placed in the prone position with the head titled slightly downward. A midline suboccipital approach was performed from the rostral end of the patient using ORBEYE. Clipping was safely accomplished in a comfortable posture. No operative complications occurred. Postoperative computed tomography angiography showed complete aneurysmal obstruction.
Conclusion: Exoscopic surgery using ORBEYE is feasible for a midline suboccipital approach to VA–PICA aneurysms from the rostral end of the patient with the patient in the prone with slight head-down position.
Keywords: Clipping, Exoscope, Midline suboccipital approach, Posterior inferior cerebellar artery aneurysm, ORBEYE
INTRODUCTION
Vertebral artery–posterior inferior cerebellar artery (VA–PICA) aneurysms account for 0.5–3.0% of all intracranial aneurysms.[
When the midline suboccipital approach is performed using a conventional surgical microscope in the prone position, the visual axis looking down from the rostral end of the patient is suitable for manipulation of a caudal VA–PICA aneurysm. In addition, the visual axis looking up from the caudal end is suitable for manipulation of a rostral lesion.[
Recently, multiple exoscope systems are available for neurosurgical use, including the KINEVO (Carl Zeiss AG Carl Zeiss Meditec AG, Oberkochen, Germany), VITOM 3-dimensional (3D) (KARL STORZ SE & Co. KG, Tuttlingen, Germany), Synaptive Modus V (Synaptive Medical, Toronto, Canada), Aeos 3D Digital Exoscope (Aesculap Inc.), and ORBEYE (Sony Olympus Medical Solutions Inc., Tokyo, Japan). These exoscopes contain 4K-3D displays, light filters for 5-aminolevulinic acid and indocyanine green video angiography, flexible arms, adjustable operative settings, multiscreen output, longer focus distance, and a greater magnification power. The ORBEYE (Olympus, Tokyo, Japan), which was the first to have 4K HD clarity concurrently with 3D visualization, provides high magnification function that can range from 1.1 to 25.8 times and high zooming ratio of 1:12 times (6 times through optical zooming and 2 times through digital zooming).[
We report a patient who underwent VA–PICA aneurysm clipping using the midline suboccipital approach from the rostral end using ORBEYE.
CASE PRESENTATION
The patient provided written informed consent for publication of her information and related images.
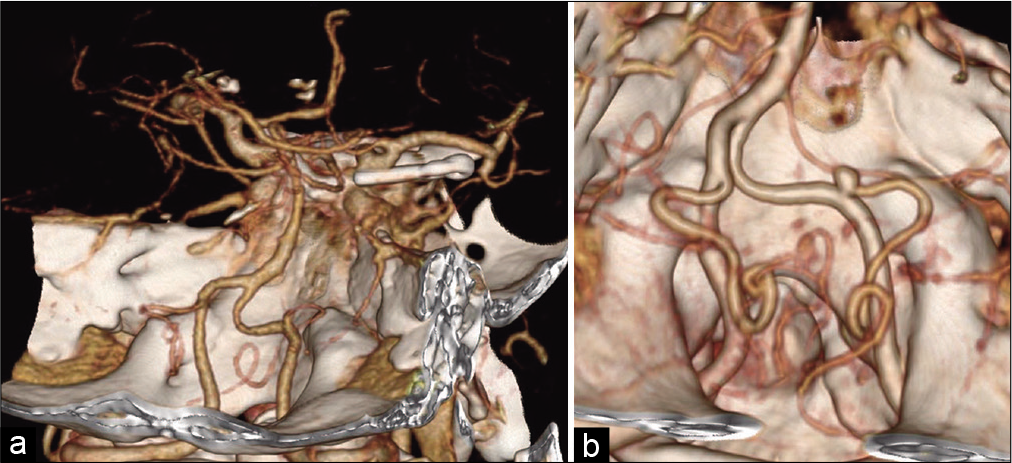
A 65-year-old woman who had previously undergone clipping of a right internal carotid artery–posterior communicating artery bifurcation aneurysm [
Figure 1:
Preoperative imaging. (a) The patient had previously undergone clipping of a right internal carotid artery–posterior communicating artery bifurcation aneurysm. (b) Preoperative computed tomography angiography showed an unruptured right-sided vertebral artery aneurysm (maximum diameter, 5 mm) located medially and ventral to the hypoglossal canal.
Figure 2:
Intraoperative views. (a) The patient was placed in the prone position with her neck slightly flexed and head slightly bent forward, rotated 10° to the right, and fixed in a Sugita surgical head frame (Mizuho, Tokyo, Japan). (b) Overhanging the visual axis of ORBEYE, the aneurysm was visible caudal to cranial nerves (CNs) IX, X, and XI. CN XII was attached to the distal neck of the aneurysm. The AICA was found on the ventral side of the aneurysm but the structures were not in contact. (c) A 7 mm mini straight titanium Yasargil® titanium clip (Aesculap, Center Valley, PA, USA) was applied to the aneurysm neck from beneath the lower CNs using forceps with a 15° downward bend. (d) Clipping achieved complete aneurysmal obstruction. (e) Intraoperative indocyanine green angiography showed no blood flow within the aneurysm and preservation of flow in the VA and PICA.
After the visual axis of ORBEYE was set to overhang, rostral retraction of the lateral cerebellum revealed CNs IX, X, and XI. Caudal to the nerves, the right VA and PICA were visible. The aneurysm was found slightly anterior to the origin of the PICA and its distal neck was adherent to CN XII. Using the high magnification function of ORBEYE, CN XII was detached from the aneurysm neck. Although the anterior inferior cerebellar artery (AICA) was found on the ventral side of the aneurysm, the structures were not in contact [
All microsurgical procedures were performed from the rostral end of the patient using ORBEYE. Adjusting the visual axis of ORBEYE enabled surgery to be performed with the surgeon in a comfortable posture. In addition, an extreme head-down position was not required.
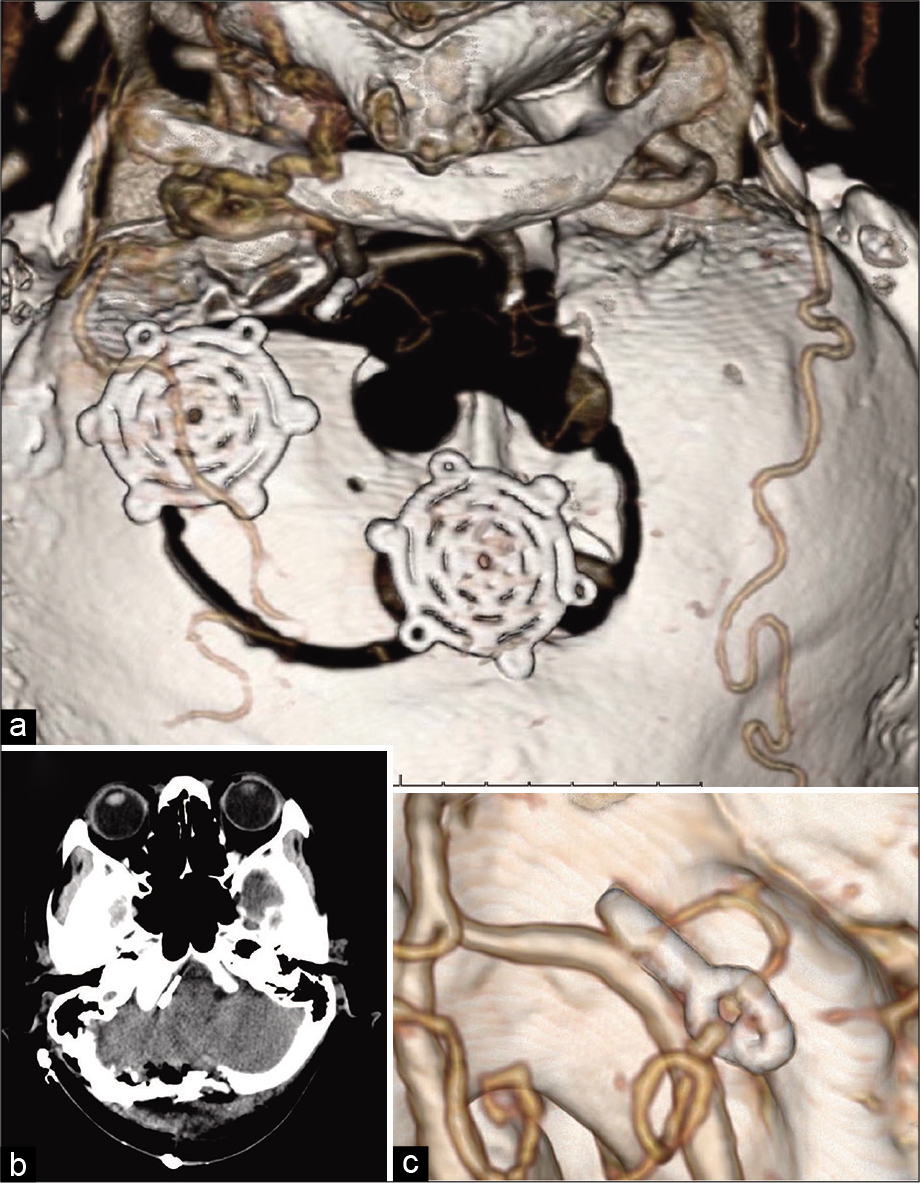
No operative complications occurred. Postoperative computed tomography angiography showed complete obliteration of the VA–PICA aneurysm and preservation of the VA and PICA [
Figure 3:
Postoperative imaging. (a) Three-dimensional computed tomography (CT) reconstruction showed the paramedian craniotomy, foramen magnum craniectomy, and resection of the right occipital bone out to the level of the condylar fossa. (b) Postoperative plain CT showed no bleeding or cerebral infarction. (c) Postoperative CT angiography showed complete obliteration of the aneurysm and preservation of the vertebral and posterior inferior cerebellar arteries.
DISCUSSION
Although VA–PICA aneurysms are generally clipped using the lateral suboccipital approach,[
The exoscope is currently being used by some surgeons as an alternative to the conventional microscope.[
The prone position is generally recommended for the midline suboccipital approach.[
When the midline suboccipital approach in the prone position is used for aneurysms located ventrally in the posterior fossa, such as distal VA and proximal PICA aneurysms, use of a conventional surgical microscope from the rostral end of the patient requires the surgeon to overhang the visual axis of the microscope and perform surgical manipulations in an uncomfortable posture.[
In other hands, we also experienced some limitations of the ORBEYE in the present case. First, it is necessary to adjust camera position frequently to focus the most deep-seated structures such as AICA on the ventral side of the aneurysm. One of the reasons may be related to depth-of-field. In general, depth-of-field was defined by the distance from subject to lens, the focal length, and the aperture. The longer focal length, the shallower the depth-of-field. ORBEYE has longer focal length (220–550 mm) without the function of aperture, compared to conventional optical microscope.[
Further studies of exoscopes and microscopes are needed.
CONCLUSION
Exoscopic surgery using ORBEYE is feasible for a midline suboccipital approach to VA–PICA aneurysms from the rostral end of the patient with the patient in the prone with slight head-down position. This technique enables the surgeon to perform stable microsurgery in a comfortable posture regardless of the operative visual axis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Khayat H, Al-Khayat H, Beshay J, Manner D, White J. Vertebral artery-posteroinferior cerebellar artery aneurysms: Clinical and lower cranial nerve outcomes in 52 patients. Neurosurgery. 2005. 56: 2-10
2. Chalouhi N, Jabbour P, Starke RM, Tjoumakaris SI, Gonzalez LF, Witte S. Endovascular treatment of proximal and distal posterior inferior cerebellar artery aneurysms. J Neurosurg. 2013. 118: 991-9
3. Depauw P, Groen RJ, van Loon J, Peul WC, Malbrain M, de Waele JJ. The significance of intra-abdominal pressure in neurosurgery and neurological diseases: A narrative review and a conceptual proposal. Acta Neurochir (Wien). 2019. 161: 855-64
4. Fiani B, Jarrah R, Griepp DW, Adukuzhiyil J. The role of 3D exoscope systems in neurosurgery: An optical innovation. Cureus. 2021. 13: e15878
5. Forget TR, Benitez R, Veznedaroglu E, Sharan A, Mitchell W, Silva M. A review of size and location of ruptured intracranial aneurysms. Neurosurgery. 2001. 49: 1322-5
6. Haeren R, Hafez A, Lehecka M. Visualization and maneuverability features of a robotic arm three-dimensional exoscope and operating microscope for clipping an unruptured intracranial aneurysm: Video comparison and technical evaluation. Oper Neurosurg (Hagerstown). 2022. 22: 28-34
7. Heros RC. Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg. 1986. 64: 559-62
8. Horowitz M, Kopitnik T, Landreneau F, Krummerman J, Batjer HH, Thomas G. Posteroinferior cerebellar artery aneurysms: Surgical results for 38 patients. Neurosurgery. 1998. 43: 1026-32
9. Iwata T, Toyota S, Kudo A, Nakagawa K, Shimizu T, Murakami T. Microsurgery “Under the Eaves” using ORBEYE: A case of dural arteriovenous fistula of the anterior cranial fossa. World Neurosurg. 2020. 138: 178-81
10. Izumo T, Ujifuku K, Baba S, Morofuji Y, Horie N, Matsuo T. Initial experience of ORBEYE™ surgical microscope for carotid endarterectomy. Asian J Neurosurg. 2019. 14: 839-42
11. Kikuta KI, Miyamoto S, Kataoka H, Satow T, Yamada K, Hashimoto N. Use of the prone oblique position in surgery for posterior fossa lesions. Acta Neurochir (Wien). 2004. 146: 1119-24
12. Langer DJ, White TG, Schulder M, Boockvar JA, Labib M, Lawton MT. Advances in intraoperative optics: A brief review of current exoscope platforms. Oper Neurosurg (Hagerstown). 2020. 19: 84-93
13. Matsushima T, Kawashima M, Masuoka J, Mineta T, Inoue T. Transcondylar fossa (supracondylar transjugular tubercle) approach: Anatomic basis for the approach, surgical procedures, and surgical experience. Skull Base. 2010. 20: 83-91
14. Mericle RA, Reig AS, Burry MV, Eskioglu E, Firment CS, Santra S. Endovascular surgery for proximal posterior inferior cerebellar artery aneurysms: An analysis of glasgow outcome score by hunt-hess grades. Neurosurgery. 2006. 58: 619-25
15. Montemurro N, Scerrati A, Ricciardi L, Trevisi G. The exoscope in neurosurgery: An overview of the current literature of intraoperative use in brain and spine surgery. J Clin Med. 2021. 11: 223
16. Murai Y, Sato S, Yui K, Morimoto D, Ozeki T, Yamaguchi M. Preliminary clinical microneurosurgical experience with the 4K3-dimensional microvideoscope (ORBEYE) system for microneurological surgery: Observation study. Oper Neurosurg (Hagerstown). 2019. 16: 707-16
17. Murakami T, Toyota S, Suematsu T, Wada Y, Nakagawa K, Shimizu T. Four hands surgery for intracerebral hemorrhage using orbeye: Educational values and ergonomic advantages-a technical note. Asian J Neurosurg. 2021. 16: 634-7
18. Nakao K, Thavara BD, Tanaka R, Yamada Y, Joshi G, Miyatani K. Surgeon experience of the surgical safety with KINEVO 900 in vascular neurosurgery: The initial experience. Asian J Neurosurg. 2020. 15: 464-7
19. Peluso JP, van Rooij WJ, Sluzewski M, Beute GN, Majoie CB. Posterior inferior cerebellar artery aneurysms: Incidence, clinical presentation, and outcome of endovascular treatment. AJNR Am J Neuroradiol. 2008. 29: 86-90
20. Roethe AL, Landgraf P, Schröder T, Misch M, Vajkoczy P, Picht T. Monitor-based exoscopic 3D4k neurosurgical interventions: A two-phase prospective-randomized clinical evaluation of a novel hybrid device. Acta Neurochir (Wien). 2020. 162: 2949-61
21. Rösler J, Georgiev S, Roethe AL, Chakkalakal D, Acker G, Dengler NF. Clinical implementation of a 3D4Kexoscope (Orbeye) in microneurosurgery. Neurosurg Rev. 2022. 45: 627-35
22. Shimizu T, Toyota S, Nakagawa K, Murakami T, Mori K, Kishima H. Retrosigmoid approach in the supine position using ORBEYE: A consecutive series of 14 cases. Neurol Med Chir (Tokyo). 2021. 61: 55-61
23. Sugiyama T, Mizutani T, Shimizu K, Sumi K, Nakajo T, Matsumoto M. Treatment of vertebral artery aneurysm with OA-PICA bypass in the prone position. Surg Cereb Stroke. 2019. 47: 255-9
24. Sugiyama T, Mizutani T, Sumi K, Matsumoto M, Yabusaki H, Kusyamae M. Trapping of vertebral aneurysms using mid-lateral suboccipital approach, with emphasis on securing the distal end. Surg Cereb Stroke. 2016. 44: 461-8
25. Toyota S, Murakami T, Shimizu T, Nakagawa K, Taki T. Exoscopic carotid endarterectomy using movable 4K 3D monitor: Technical note. Surg Neurol Int. 2021. 12: 540
26. Vogelbaum MA, Kroll D, Etame A, Tran N, Liu J, Ford A. A prospective validation study of the first 3D digital exoscope for visualization of 5-ALA-induced fluorescence in high-grade gliomas. World Neurosurg. 2021. 149: e498-503
27. Yamaura A, Ise H, Makino H. Radiometric study on posterior inferior cerebellar aneurysms with special reference to accessibility by the lateral suboccipital approach. Neurol Med Chir (Tokyo). 1981. 21: 721-3