- Department of Neurosurgery, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Ritto, Shiga, Japan.
Correspondence Address:
Shigeomi Yokoya, Department of Neurosurgery, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Ritto, Shiga, Japan.
DOI:10.25259/SNI_645_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shigeomi Yokoya. Migration of the ventriculoperitoneal shunt into the thoracic cavity: A case report and pitfalls of the rib structure. 15-Sep-2023;14:340
How to cite this URL: Shigeomi Yokoya. Migration of the ventriculoperitoneal shunt into the thoracic cavity: A case report and pitfalls of the rib structure. 15-Sep-2023;14:340. Available from: https://surgicalneurologyint.com/surgicalint-articles/12547/
Abstract
Background: Although ventriculoperitoneal shunting (VPS) is a universal treatment for hydrocephalus, it is generally well-known that the procedure often has complications. Shunt catheter migration is one such complication, but no reports of migration into the thoracic cavity are associated with the surgical technique. Herein, I present a case of thoracic cavity migration of a shunt catheter alongside anatomical pitfalls of the rib structure.
Case Description: The patient was a 62-year-old male diagnosed with subarachnoid hemorrhage due to craniocervical junction arteriovenous fistula and underwent direct surgery to occlude the fistula. We performed VPS for secondary hydrocephalus 1 month later. During VPS, the peritoneal catheter was tunneled subcutaneously over the clavicle to pass from the head to the abdomen. Several months later, the peritoneal catheter had migrated from the peritoneal cavity to the thoracic cavity. A computed tomography scan showed that the peritoneal catheter tunneled subcutaneously over the clavicle, penetrated the thoracic wall through the intercostal space between ribs 1 and 2, and entered the thoracic cavity.
Conclusion: When performing VPS, it is not enough to send the passer through the skin over the clavicle; it must also be tunneled subcutaneously over the ribs while confirming the position of the tip by touch.
Keywords: Abdominal catheter, Hydrocephalus, Peritoneal cavity, Thoracic cavity, Ventriculoperitoneal shunting
INTRODUCTION
Ventriculoperitoneal shunting (VPS) is a universal treatment for hydrocephalus. Although it is a relatively simple surgery, the overall rate of complications is high, with 33th,i of patients experiencing some form of complication after shunt placement and 2.7% of these cases leading to death.[
The most common surgical technique for VPS is to tunnel a shunt passer beneath the skin and, then, send the abdominal catheter through the passer from the head to the peritoneal cavity. The surgeon must ensure that the passer does not enter the thoracic cavity when tunneling from the head incision to the abdominal incision to prevent a complication of pneumothorax.
It is taught that the clavicle is the structure around which the most care must be taken when subcutaneously moving from the neck to the thoracic wall. If one avoids entering the thoracic cavity by tunneling the passer through the skin over the clavicle, it is often possible to tunnel the catheter subcutaneously over the ribs afterward without difficulty.
I experienced a case in which, despite passing over the clavicle, the catheter passed through the thoracic cavity on the way to the peritoneal cavity, allowing the catheter tip to migrate to the thoracic cavity from the peritoneal cavity. Herein, I present the details of this case along with the anatomical features of the rib structure.
CASE DESCRIPTION
A 62-year-old male with a history of colorectal cancer surgery and hyperlipidemia presented to our hospital with sudden-onset pain in the back of the neck. On arrival, the patient’s Glasgow Coma Scale was E3V5M6, with no focal neurologic deficits.
Based on imaging tests, the patient was diagnosed with subarachnoid hemorrhage due to a craniocervical junction arteriovenous fistula and underwent direct surgery to occlude the fistula. VPS was performed 1 month later because the patient developed secondary hydrocephalus. The postoperative abdominal X-ray confirmed that the shunt catheter was placed in the peritoneal cavity [
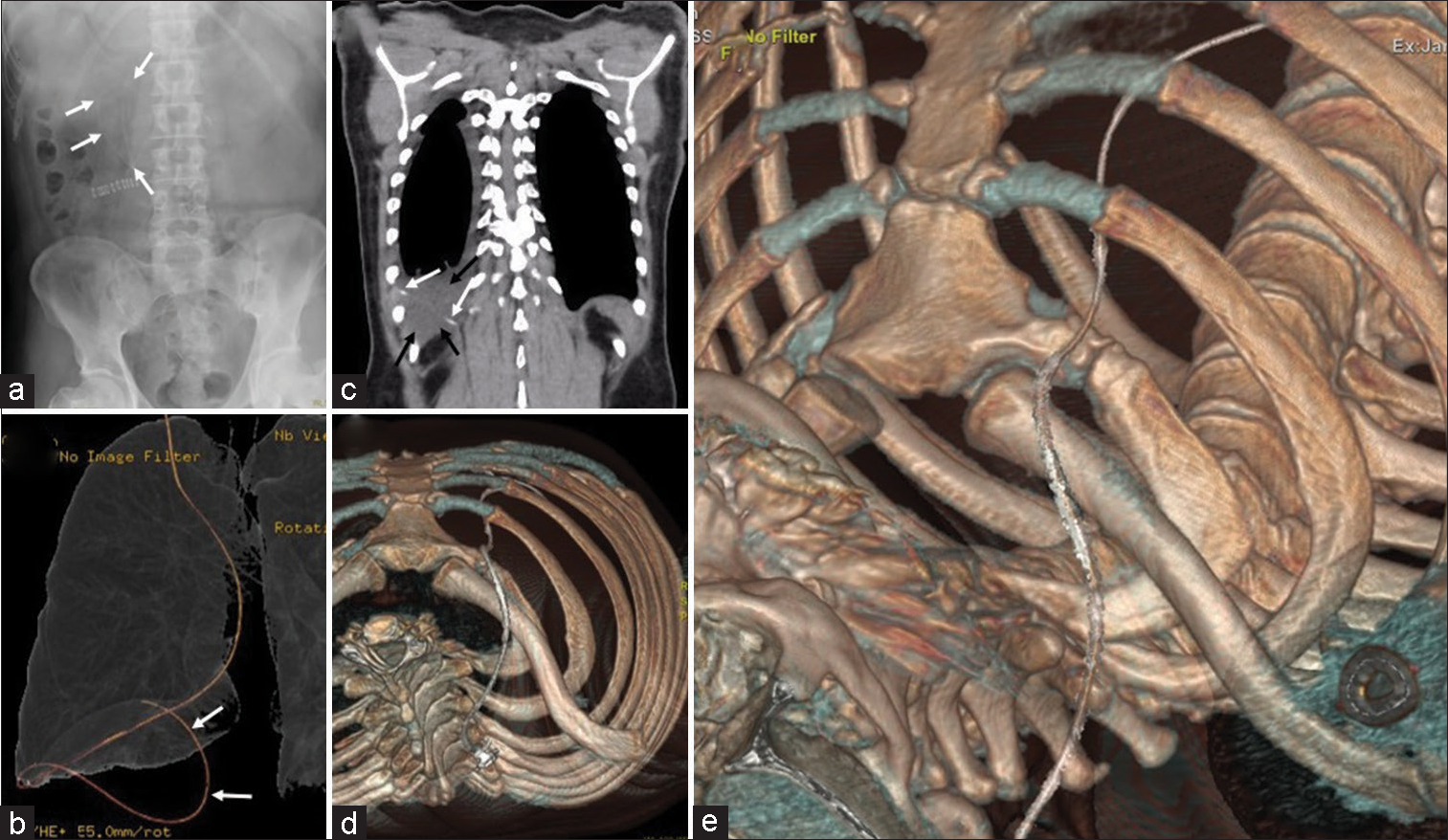
Figure 1:
Perioperative imaging findings. (a) Abdominal X-ray, taken on ventriculoperitoneal shunting postoperative day 1, showing a peritoneal catheter (white arrows) placed within the peritoneal cavity. (b) Computed tomography (CT), taken before shunt reconstruction, volume rendering of the pulmonary structure, showing the migration of the peritoneal catheter (white arrows) into the thoracic cavity. (c) Coronal chest CT image, taken before shunt reconstruction, showing pleural effusion (black arrows) around the peritoneal catheter (white arrows) in the thoracic cavity. (d and e) Volume rendering CT of the bone, cranial axial plane image and operative view, showing the peritoneal catheter entering the thoracic cavity through the intercostal space between ribs 1 and 2 despite passing over the clavicle. Note that there is a risk of mistakenly inserting the peritoneal catheter into the thoracic cavity due to the wide intercostal space between ribs 1 and 2, and ribs 2 and 3.
Six months after VPS, an abdominal computed tomography was performed as a follow-up of colorectal cancer surgery and showed that the peritoneal catheter had migrated to the thoracic cavity [
The presence of pleural effusion and associated atelectasis led us to perform reconstructive surgery. We secured the peritoneal catheter, which had migrated to the thoracic cavity, 1 cm caudal to the clavicle. We removed the peritoneal catheter which entered the thoracic cavity without resistance. After removal, we tunneled the peritoneal catheter subcutaneously over the ribs. We, then, reopened the abdominal incision from the previous surgery, opened the anterior/posterior sheath of the rectus abdominis and peritoneum, and verified the intestinal tract within the peritoneal cavity before placing the catheter.
DISCUSSION
In this case, the peritoneal catheter was tunneled through the thoracic cavity while performing VPS. Since the catheter entered the abdomen subcutaneously after passing through the wall side of the pleura (without passing through the diaphragm), it was placed within the peritoneal cavity using ordinary abdominal manipulation. However, as time passed, the peritoneal catheter withdrew from the peritoneal cavity and entered the thoracic cavity, causing pleural effusion and atelectasis, leading to reconstructive surgery.
This case showed that even when the shunt catheter is tunneled subcutaneously over the clavicle, it can pass under the rib caudal to the clavicle, in other words, through the thoracic cavity, on its way to the peritoneal cavity. This is possible due to the anatomical structure of the thoracic wall.
Furthermore, this case showed that it is possible for a peritoneal catheter that passes through the thoracic cavity on its way to the peritoneal cavity to withdraw into the thoracic cavity over time. The thoracic cavity is in a constant state of negative pressure, while the peritoneal cavity is in a constant state of positive pressure. The difference in pressure may have resulted in the migration of the peritoneal catheter to the thoracic cavity after placement.
To the best of my knowledge, there is a reported case of peritoneal catheter migration from the thoracic cavity to the peritoneal cavity after VPS in which the catheter passed through the anatomically vulnerable area where the superior epigastric vessels penetrate the diaphragm.[
CONCLUSION
Surgeons performing VPS must recognize that even when the shunt catheter is tunneled subcutaneously over the clavicle, it may pass under the rib caudal to the clavicle, in other words, through the thoracic cavity, on its way to the peritoneal cavity, and that catheters, which pass through the thoracic cavity on its way to the peritoneal cavity, can withdraw into the thoracic cavity over time.
Ethical approval
All procedures performed in this report were in accordance with the 1964 Helsinki Declaration. However, a series of treatments had been performed after obtaining appropriate written informed consent from the patients. Additional written consent for inclusion in this study was relinquished by the Ethics Committee of our Hospital because of the retrospective and observational nature of the study (Permission number: 583).
Declaration of patient consent
The Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cooper JR. Migration of ventriculoperitoneal shunt into the chest. Case report. J Neurosurg. 1978. 48: 146-7
2. Merkler AE, Ch’ang J, Parker WE, Murthy SB, Kamel H. The rate of complications after ventriculoperitoneal shunt surgery. World Neurosurg. 2017. 98: 654-8
3. Wu Y, Green NL, Wrensch MR, Zhao S, Gupta N. Ventriculoperitoneal shunt complications in California: 1990 to 2000. Neurosurgery. 2007. 61: 557-62 discussion 562-3