- Spine Services, Indian Spinal Injuries Centre, New Delhi, India.
DOI:10.25259/SNI_435_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vikas Tandon, Abhinandan Reddy Mallepally, Ashok Reddy Peddaballe, Nandan Marathe, Harvinder Singh Chhabra. Mini-open thoracoscopic-assisted spinal thoracotomy for traumatic injuries: A technical note. 29-Aug-2020;11:265
How to cite this URL: Vikas Tandon, Abhinandan Reddy Mallepally, Ashok Reddy Peddaballe, Nandan Marathe, Harvinder Singh Chhabra. Mini-open thoracoscopic-assisted spinal thoracotomy for traumatic injuries: A technical note. 29-Aug-2020;11:265. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10229
Abstract
Background: Mini-open thoracoscopic-assisted thoracotomy (MOTA) has been introduced to mitigate disadvantages of conventional open anterior or conventional posterior only thoracoscopic procedures. Here, we evaluated the results of utilizing the MOTA technique to perform anterior decompression/fusion for 22 traumatic thoracic fractures.
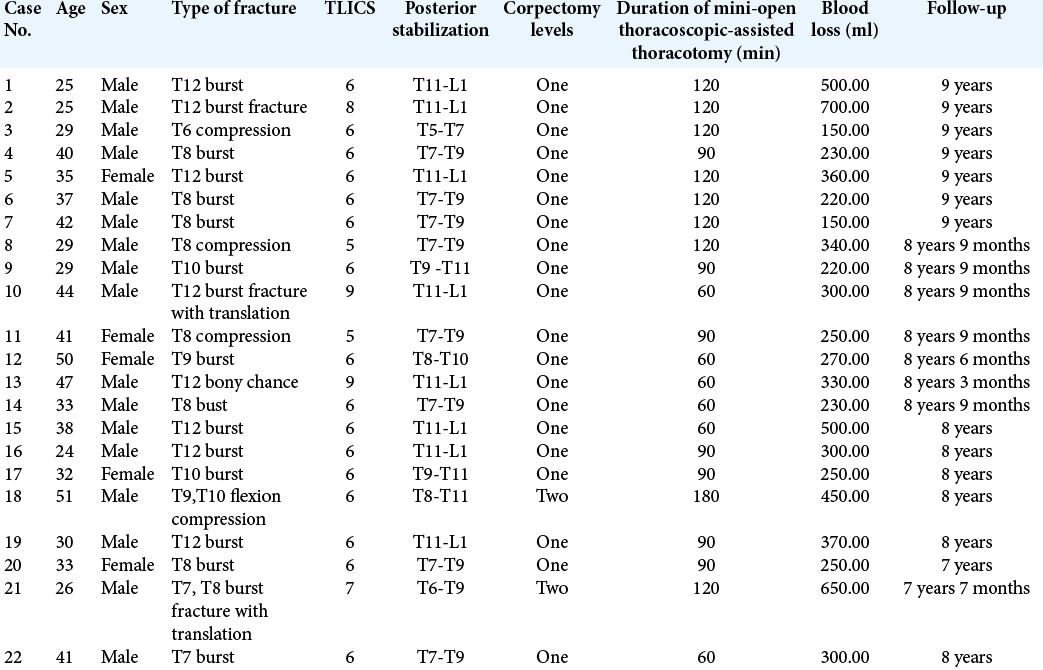
Methods: There were 22 patients with unstable thoracic burst fractures (TBF) who underwent surgery utilizing the MOTA thoracotomy technique. Multiple variables were studied including; the neurological status of the patient preoperatively/postoperatively, the level and type of fracture, associated injuries, operative time, estimated blood loss, chest tube drainage (intercostal drainage), length of hospital stay (LOS), and complication rate.
Results: In 22 patients (averaging 35.5 years of age), T9 and T12 vertebral fractures were most frequently encountered. There were 20 patients who had single level and 2 patients who had two-level fractures warranting corpectomies. Average operating time and blood loss for single-level corpectomy were 91.5 ± 14.5 min and 311 ml and 150 ± 18.6 min and 550 ml for two levels, respectively. Mean hospital stay was 5 days. About 95.45% of cases showed fusion at latest follow-up. Average preoperative kyphotic angle corrected from 34.2 ± 3.5° to 20.5 ± 1.0° postoperatively with an average correction of 41.1% and correction loss of 2.4%.
Conclusion: We concluded that utilization of the MOTA technique was safe and effective for providing decompression/fusion of traumatic TBF.
Keywords: Burst fracture, Mini-open, Thoracic, Thoracoscopic, Thoracotomy
INTRODUCTION
Management of acute traumatic fractures of thoracic and thoracolumbar spine has varied widely with time and individual surgeon preferences. Previous operations have included posterior only surgery versus anterior only surgery versus combined anterior/posterior surgical stabilization.[
Mini-open thoracoscopic-assisted thoracotomy (MOTA) spine surgery has been introduced to mitigate the complications of anterior only, posterior only, or 360 procedures. It also has advantages of being minimally invasive while providing a direct vision of the pathological site in three dimensions rather than two-dimensional images of thoracoscopy. There is, however, a paucity of literature regarding the safety and efficacy of MOTA thoracotomy for treating unstable thoracic burst fracture (TBF). Here, we evaluated the results of utilizing the MOTA technique in anterior decompression and fusion of 22 traumatic TBFs.
MATERIALS AND METHODS
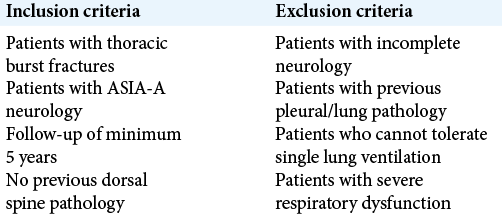
This retrospective study was conducted at a tertiary care spine center after approval from the Institutional Review Board. A total of 22 patients with unstable TBF underwent the MOTA thoracotomy technique. Patients with incomplete neurological involvement and with previous pulmonary pathologies were excluded from the study [
Surgical technique
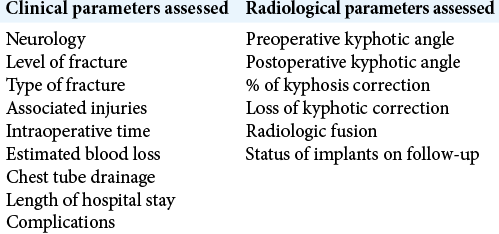
General anesthesia utilized a double-lumen tube for intubation to maintain single lung ventilation when required. All patients included in the study first underwent posterior stabilization in the prone position followed by the right lateral decubitus (i.e., left chest upwards) position [
Mini-thoracotomy portal
On a radiolucent table, the mini-thoracotomy surface was marked on the skin by noting the level of the fractured vertebrae/disc and/or adjacent vertebrae. For a single-level fracture/corpectomy, the incision line extended from the middle of the posterior wall of the proximal vertebrae to middle of the anterior wall of distal vertebrae [
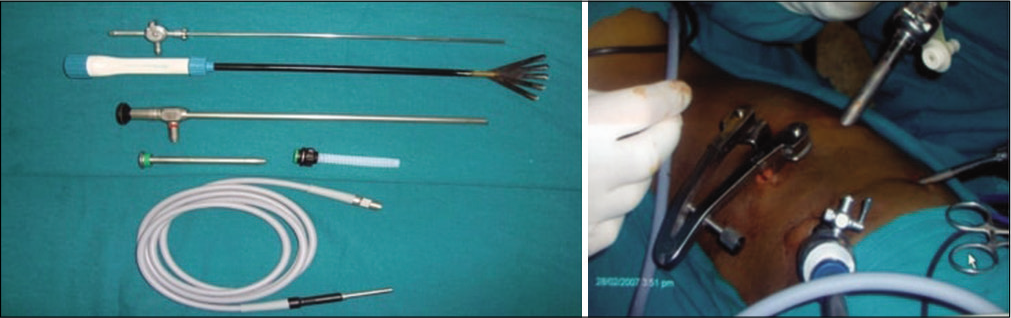
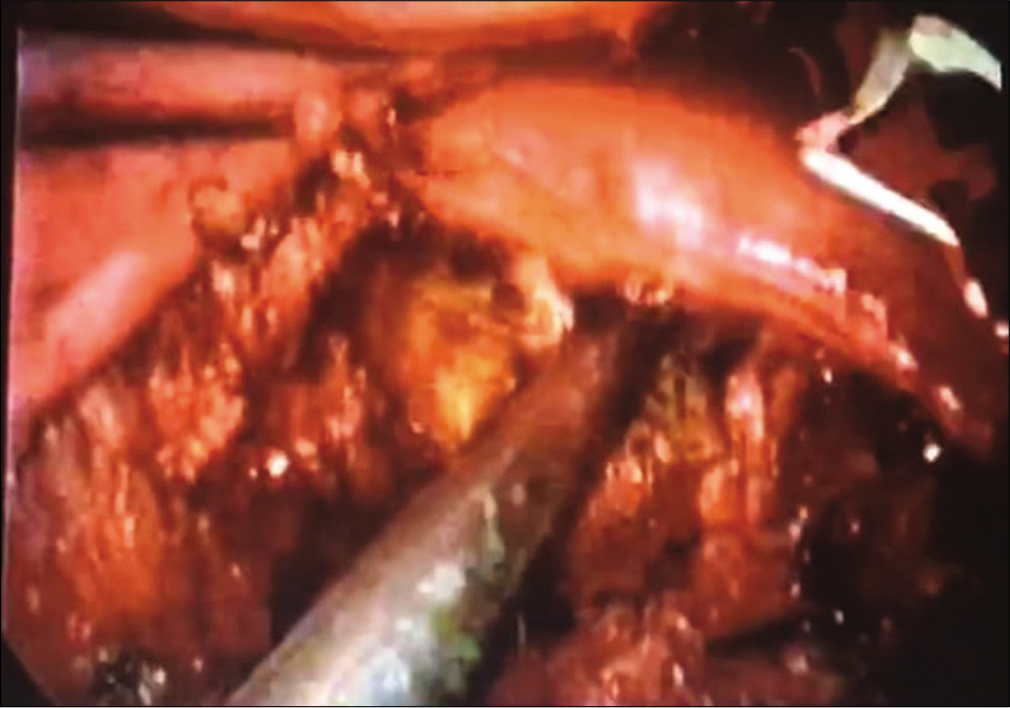
The thoracoscope was then removed from mini-thoracotomy incision and inserted through viewing portal sleeve, to the desired vertebral level. Regular spine instruments (short handle) were utilized to perform the single- or two-level corpectomy of the involved fracture vertebra, along with cord decompression [
Postoperative care
Patients were mobilized on the 1st postoperative day (e.g., sitting with or without support). The ICD drain was removed when 24 h collection in both drains together was <50 ml. Sitting radiographs were taken on the 3rd postoperative day and at every follow-up examination [
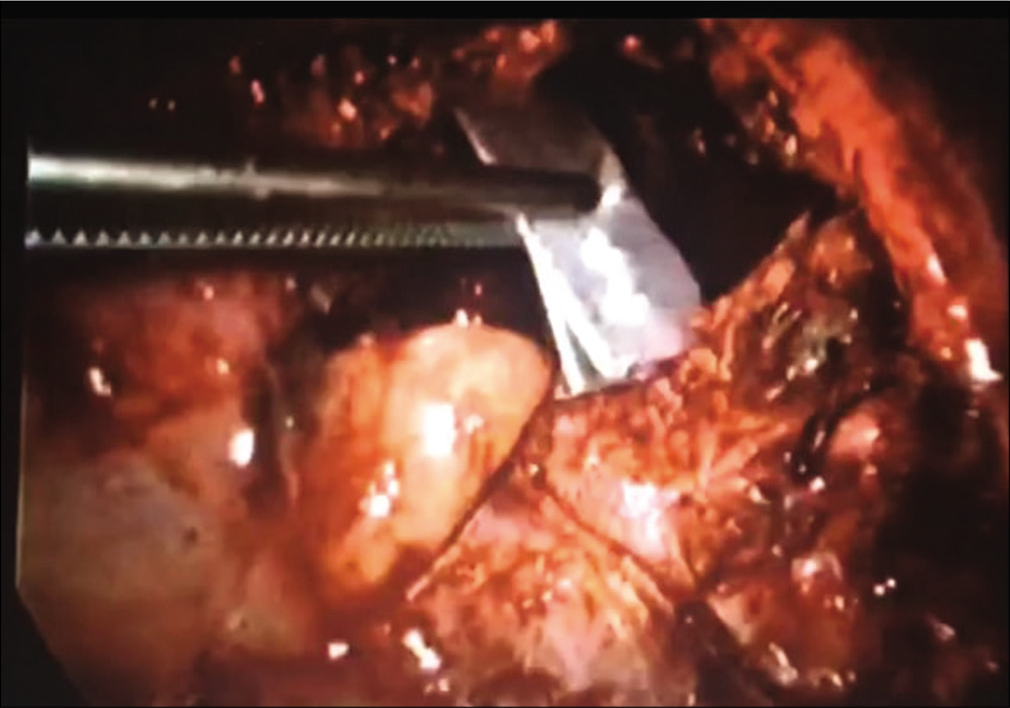
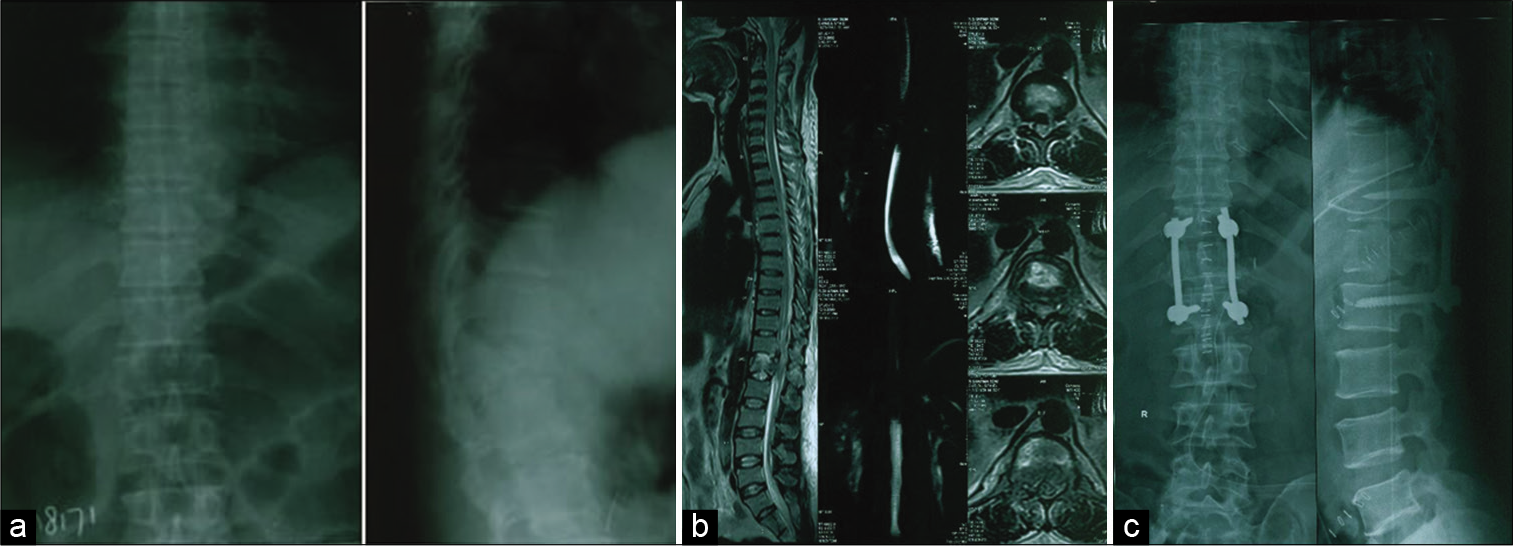
Figure 6:
(a) Preoperative anteroposterior and lateral radiograph showing burst fracture of T12 vertebra. (b) Sagittal and axial magnetic resonance imaging showing fracture of T12 vertebra with surrounding edema. (c) Postoperative anteroposterior and lateral radiographs showing T11-L1 posterior pedicle screw instrumentation with anterior iliac crest strut graft in position.
RESULTS
Twenty-two patients were included in study. They averaged 35.5 years of age and were followed up for 8 years 3 months on an average [
About 95.45% of cases showed fusion at the latest follow-up. One patient showed radiological evidence of pseudoarthrosis. The average preoperative kyphotic angle was corrected from 34.2 ± 3.5° to 20.5 ± 1.0° postoperatively with an average correction of 41.1%. Radiographs at final follow-up showed an average loss of kyphotic correction of 2.4% and there was no evidence of implant loosening or migration.
The most common complication was intercostal neuralgia seen in 12 patients; 10 required membrane stabilizing agents (pregabalin) and two patients required intercostal nerve block. There was one case with traumatic cerebrospinal fluid leakage; this was successfully managed with a muscle graft and postoperative lumbar drainage. The patient with pseudoarthrosis was clinically asymptomatic. On close follow-up, there was no evidence of implant failure or increase in kyphosis. Hence, no active intervention was done.
DISCUSSION
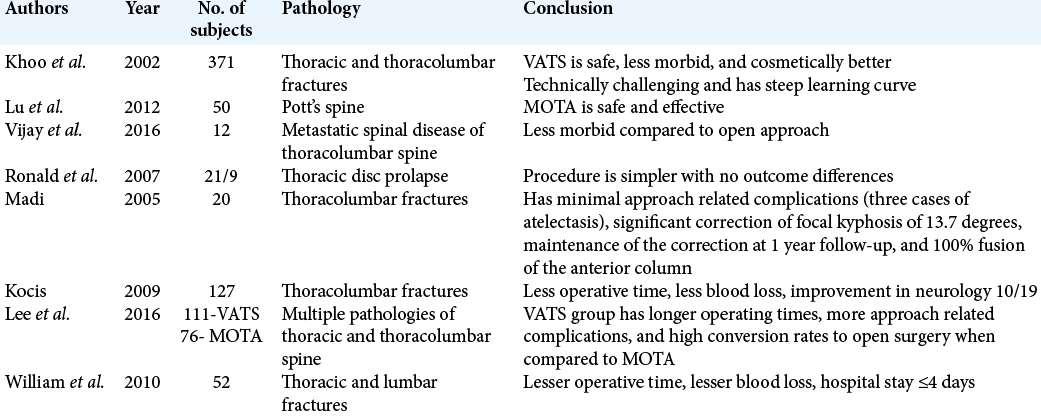
The mini-open thoracoscopic surgery (MOTA) was introduced for anterior thoracic and thoracolumbar spinal cord decompression with anterior column reconstruction. It provides direct three-dimensional visualizations of focal neurovascular structures, while also providing easy access to manage complications.[
This technique has been used successfully in various indications such as Pott’s spine, metastatic spine tumors, and thoracic disc prolapse. Lu et al.[
The present study shows the results of MOTA technique to perform corpectomy for unstable TBF. The average operating time was 120–180 min, significantly less than the open thoracotomy approach (average: 210–617 min). The average estimated blood loss (EBL) was 300–500 mL which is comparable with previously published MOTA approach literature; this is also significantly less than the average 1362 ml[
About 95.45% of cases in the current series showed fusion at their latest follow-up, with overall good stabilization of kyphosis. One patient with pseudoarthrosis was managed conservatively as he was clinically asymptomatic with no evidence of progression of kyphosis or implant failure.
Major limitations of this study include the very small sample size, retrospective nature of analysis, data from a single center, and lack of control group. Our study is just a preliminary report on the safety and efficacy of MOTA approach for the management of TBF. A multi-centric analysis with a larger sample size is needed to further validate our findings. However, we believe that the MOTA approach may serve as a useful middle ground between open and endoscopic procedures mitigating the disadvantages of each.
CONCLUSION
The MOTA approach to unstable thoracic single-/double- level fractures is yet to be confirmed, as this study is only a preliminary report as to its safety/efficacy.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Karmakar MK, Ho AM. Postthoracotomy pain syndrome. Thorac Surg Clin. 2004. 14: 345-52
2. Khoo LT, Beisse R, Potulski M. Thoracoscopic-assisted treatment of thoracic and lumbar fractures: A series of 371 consecutive cases. Neurosurgery. 2002. 51: S104-17
3. Kocis J, Wendsche P, Muzík V, Bilik A, Veselý R, Cernohousová I. Minimally invasive thoracoscopic transdiaphragmatic approach to thoracolumbar junction fractures. Acta Chir Orthop Traumatol Cech. 2009. 76: 232-8
4. Lee CY, Wu MH, Li YY, Cheng CC, Lee CY, Huang TJ. Video-assisted thoracoscopic surgery and minimal access spinal surgery compared in anterior thoracic or thoracolumbar junctional spinal reconstruction: A case-control study and review of the literature. Biomed Res Int. 2016. 2016: 6808507
5. Lu G, Wang B, Li J, Liu W, Cheng I. Anterior debridement and reconstruction via thoracoscopy-assisted mini-open approach for the treatment of thoracic spinal tuberculosis: Minimum 5-year follow-up. Eur Spine J. 2012. 21: 463-9
6. Madi K, Dehoux E, Aunoble S, Le Huec JC. Video-assisted mini-thoracotomy for surgical treatment of thoracolumbar junction fractures. Rev Chir Orthop Reparatrice Appar Mot. 2005. 91: 702-8
7. Ravindra VM, Brock A, Awad AW, Kalra R, Schmidt HM. The role of the mini-open thoracoscopic-assisted approach in the management of metastatic spine disease at the thoracolumbar junction. Neurosurg Focus. 2016. 41: E16
8. Smith WD, Dakwar E, Le TV, Christian G, Serrano S, Uribe JS. Minimally invasive surgery for traumatic spinal pathologies: A mini-open, lateral approach in the thoracic and lumbar spine. Spine (Phila Pa 1976). 2010. 35: S338-46
9. Vaccaro AR, Lehman RA, Hurlbert RJ, Anderson PA, Harris M, Hedlund R. A new classification of thoracolumbar injuries: The importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005. 30: 2325-33
10. Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: A systematic review of the literature on techniques, complications, and outcome. Spine. 2004. 29: 803-14