- Department of Neurosurgery, Rhode Island Hospital, Providence, Rhode Island, United States
- Department of Neurosurgery, New York Presbyterian Hospital, New York, New York State, United States.
Correspondence Address:
Hael Abdulrazeq, Department of Neurosurgery, Rhode Island Hospital, Providence, Rhode Island, United States.
DOI:10.25259/SNI_604_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Radmehr Torabi1, Joseph Anthony Carnevale2, Hael Abdulrazeq1, Matthew Anderson1, Mahesh Jayaraman1, Adetokunbo Oyelese1, Ziya Gokaslan1, Krisztina Moldovan1. Minimizing blood loss with direct percutaneous polymethylmethacrylate embolization before corpectomy for vascular spinal tumors. 04-Aug-2023;14:280
How to cite this URL: Radmehr Torabi1, Joseph Anthony Carnevale2, Hael Abdulrazeq1, Matthew Anderson1, Mahesh Jayaraman1, Adetokunbo Oyelese1, Ziya Gokaslan1, Krisztina Moldovan1. Minimizing blood loss with direct percutaneous polymethylmethacrylate embolization before corpectomy for vascular spinal tumors. 04-Aug-2023;14:280. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12480
Abstract
Background: Standard surgical treatment for vascular spinal tumors, including renal cell carcinomas and hemangiomas, may result in significant blood loss despite preoperative arterial tumor embolization.
Methods: This is a retrospective review of 12 patients who underwent direct percutaneous polymethylmethacrylate embolization (DPPE) with or without feeding artery embolization before partial or complete corpectomy for the resection of vascular spinal tumors (2013–2018). Estimated blood loss (EBL) was compared to the blood loss reported in the literature and to patients receiving standard arterial embolization before surgery.
Results: The mean EBL for 12 patients was 1030 mL; three of 12 patients required blood transfusions. For the single level corpectomies, the EBL ranged from 100 mL to 3900 mL (mean 640 mL). This mean blood loss was not increased in patients receiving only DPPE preoperatively versus those patients receiving preoperative arterial embolization in addition to DPPE (1005 vs. 1416 mL); in fact, the EBL was significantly reduced for those undergoing DPPE alone.
Conclusion: In this initial study, nine patients treated with DPPE embolization alone before spinal tumor resection demonstrated reduction of intraoperative blood loss compared to three patients having arterial embolization with DDPE.
Keywords: Corpectomy, Direct percutaneous embolization, Intraoperative blood loss, Polymethyl methacrylate, Vascular spinal tumors
INTRODUCTION
The surgical resection of hypervascular spinal tumors poses significant challenges due to the risk of substantial intraoperative blood loss. Typically, these lesions are treated preoperatively with super-selective angiography and embolization that includes the selective blocking of specific blood vessels feeding the tumor and reducing the risk of intraoperative hemorrhage.
Nevertheless, these cases still usually involve an average 2.1 L, blood loss.[
MATERIALS AND METHODS
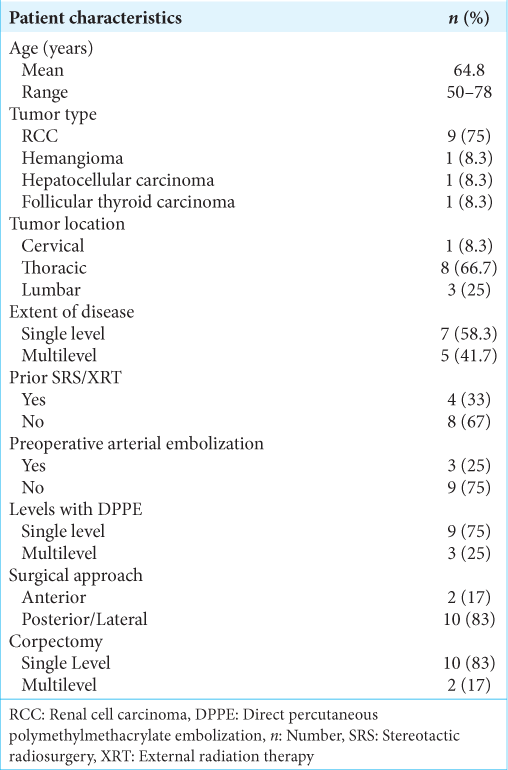
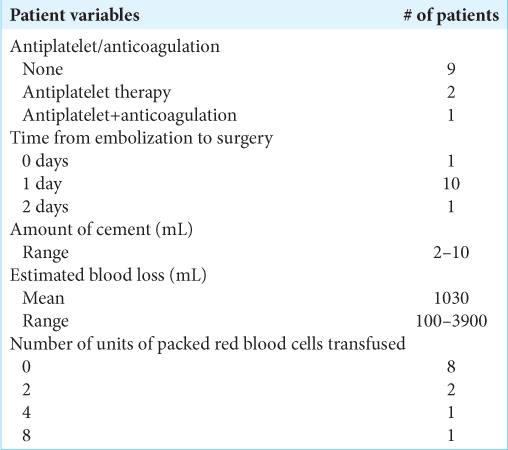
In this Institutional Review Board approved study, we retrospectively reviewed the outcomes for 12 patients (2013–2018) undergoing DPPE performed by neurosurgeons with or without additional arterial embolization (i.e., Using Polyvinyl Alcohol –and/or coils). Of note, one additional patient was removed from the study due to an intraoperative vascular injury to the iliac vein. We treated 12 patients averaging 64.8 years of age, all of whom underwent preoperative DPPE before corpectomies for spinal tumors (i.e., nine renal cell carcinoma metastases to the spine, one spinal hemangioma, one metastatic spinal hepatocellular carcinoma, and one metastasis from follicular thyroid cancer). There were eight eight thoracic lesions, three lumbar lesions, and one cervical lesion. There were seven patients with single level vertebral involvement, one with two levels, three with three levels, and one with more than three levels involved [
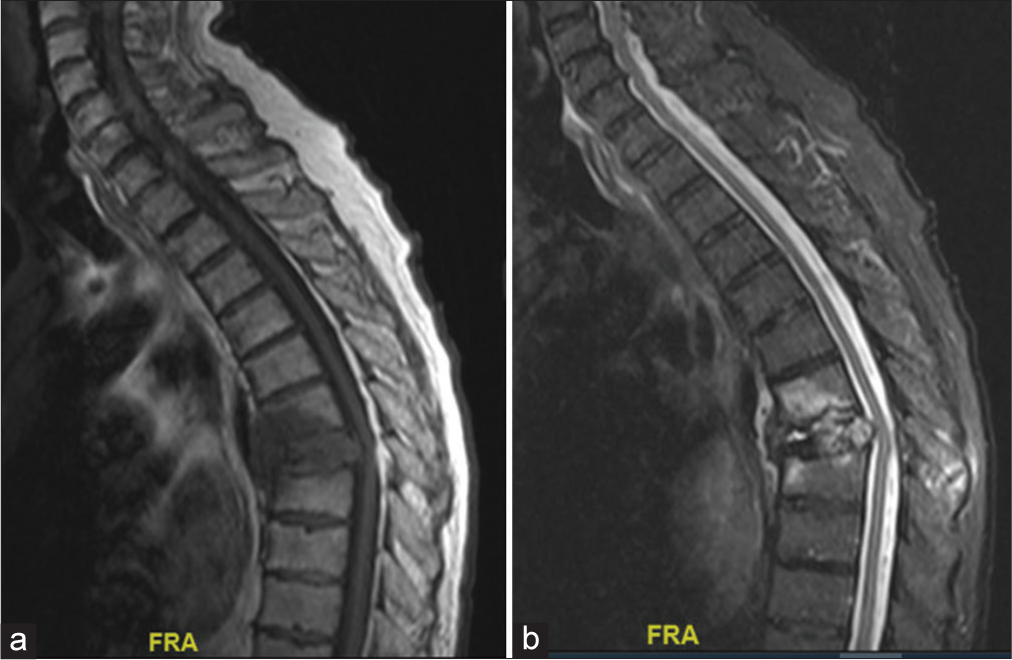
Figure 1:
(a) Sagittal magnetic resonance imaging (MRI) thoracic spine with contrast showing metastatic lesion at T7 without enhancement. (b) Sagittal MRI thoracic spine with short tau inversion recovery sequence showing hyperintensity at the affected level, suggesting edema and acute fracture. FRA: Front.
RESULTS
Treatment with DDPE with/without arterial embolization and number of vertebral levels involved
Surgery included 10 posterior or combined posterior and lateral approaches for corpectomy and two anterior approach surgeries. Three out of 12 patients received preoperative arterial embolization, plus DPPE, while nine had DDPE alone Treatment included one vertebral level in nine patients and two levels in three [
Timing of DDPE
The timing of DPPE injections varied from the day of surgery to 2 days preoperatively (i.e., average of 1 day). The average intraoperative blood loss was 1030 mL (range 100–3900 mL). Blood transfusions, averaging 4 units (packed red blood cells), were necessitated in three patients. The average blood loss in single-level cases was 640 cc, significantly lower than the 3450 mL noted in multilevel corpectomies. Notably, patients receiving preoperative arterial embolization plus DPPE exhibited an average blood loss of 1416 cc, significantly greater than the 1005 cc seen in patients only receiving DPPE preoperatively [
DISCUSSION
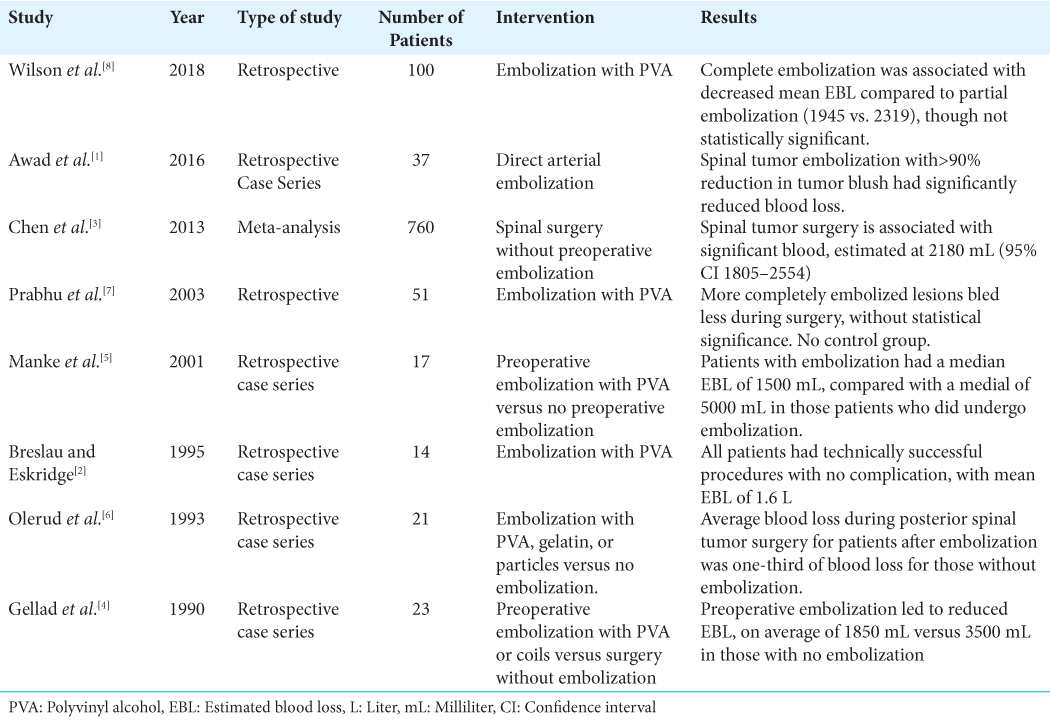
To combat extensive bleeding risk in cases of hypervascular spinal tumor resection, preoperative transarterial embolization using various embolic materials has been utilized (i.e., including detachable coils and injectable embolic agents) [
CONCLUSION
In this preliminary case series, nine patients with DDPE alone had significantly reduced intraoperative blood loss compared with those receiving both arterial embolization and DDPE.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Awad AW, Almefty KK, Ducruet AF, Turner JD, Theodore N, McDougall CG. The efficacy and risks of preoperative embolization of spinal tumors. J Neurointerv Surg. 2016. 8: 859-64
2. Breslau J, Eskridge JM. Preoperative embolization of spinal tumors. J Vasc Interv Radiol. 1995. 6: 871-5
3. Chen Y, Tai BC, Nayak D, Kumar N, Chua KH, Lim JW. Blood loss in spinal tumour surgery and surgery for metastatic spinal disease: A meta-analysis. Bone Joint J. 2013. 95B: 683-8
4. Gellad FE, Sadato N, Numaguchi Y, Levine AM. Vascular metastatic lesions of the spine: Preoperative embolization. Radiology. 1990. 176: 683-6
5. Manke C, Bretschneider T, Lenhart M, Strotzer M, Neumann C, Gmeinwieser J. Spinal metastases from renal cell carcinoma: Effect of preoperative particle embolization on intraoperative blood loss. AJNR Am J Neuroradiol. 2001. 22: 997-1003
6. Olerud C, Jónsson HJ, Löfberg AM, Lörelius LE, Sjöström L. Embolization of spinal metastases reduces peroperative blood loss. 21 patients operated on for renal cell carcinoma. Acta Orthop Scand. 1993. 64: 9-12
7. Prabhu VC, Bilsky MH, Jambhekar K, Panageas KS, Boland PJ, Lis E. Results of preoperative embolization for metastatic spinal neoplasms. J Neurosurg. 2003. 98: 156-64
8. Wilson MA, Cooke DL, Ghodke B, Mirza SK. Retrospective analysis of preoperative embolization of spinal tumors. AJNR Am J Neuroradiol. 2010. 31: 656-60