- Department of Ortho-Spine Surgery, Sir Ganga Ram Hospital, New Delhi, India.
DOI:10.25259/SNI_268_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shankar Acharya, Deepak Kaucha, Arashpreet Singh Sandhu, Nitin Adsul, R. S. Chahal, K. L. Kalra. Misdiagnosis of “White Cord Syndrome” following posterior cervical surgery for ossification of the posterior longitudinal ligament: A case report. 31-May-2021;12:244
How to cite this URL: Shankar Acharya, Deepak Kaucha, Arashpreet Singh Sandhu, Nitin Adsul, R. S. Chahal, K. L. Kalra. Misdiagnosis of “White Cord Syndrome” following posterior cervical surgery for ossification of the posterior longitudinal ligament: A case report. 31-May-2021;12:244. Available from: https://surgicalneurologyint.com/surgicalint-articles/10839/
Abstract
Background: Following decompressive cervical surgery for significant spinal cord compression/myelopathy, patients may rarely develop the “White Cord Syndrome (WCS).” This acute postoperative reperfusion injury is characterized on T2W MRI images by an increased intramedullary cord signal. However, it is a diagnosis of exclusion, and WCS can only be invoked once all other etiologies for cord injury have been ruled out.
Case Description: A 49-year-old male, 3 days following a C3-C7 cervical laminectomy and C2-T1 fusion for extensive cord compression due to ossification of the posterior longitudinal ligament (OPLL), developed acute quadriparesis. This new deficit should have been attributed to an intraoperative iatrogenic cord injury, not the WCS.
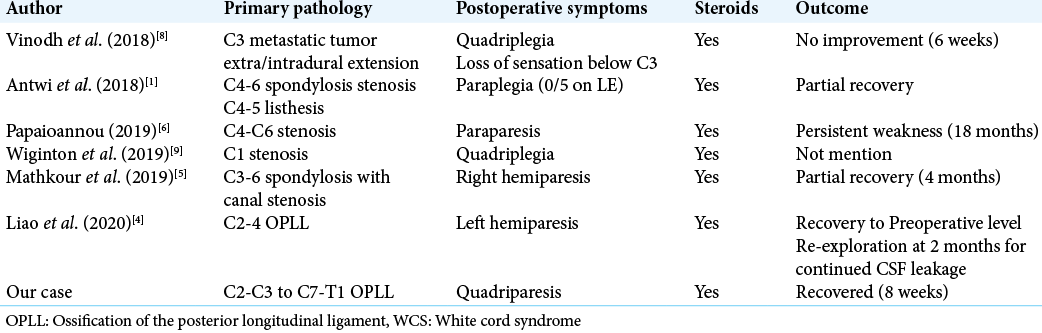
Conclusion: Very rarely patients sustain postoperative significant/severe new neurological deficits attributable to the WCS. Notably, the WCS is a diagnosis of exclusion, and all other etiologies (i.e. intraoperative iatrogenic surgeon-based mechanical cord injury, graft/instrumentation extrusion, failure to adequately remove/resect OPLL thus stretching cord over residual disease, other reasons for continued cord compression, including the need for secondary surgery, etc.) of cord injury must first be ruled out.
Keywords: Cervical decompressive surgery, Cervical myelopathy, Ossification of the posterior longitudinal ligament, White cord syndrome
INTRODUCTION
The cervical “White Cord Syndrome (WCS)” is attributed to an acute intraoperative “reperfusion injury.” This is characterized on the postoperative T2W MRI by an increased intramedullary cord signal.[
CASE REPORT
A 49-year-old male presented with 8 years of progressive myelopathy; he had acutely deteriorated over the prior month. On examination, he exhibited a significant left hemiparesis accompanied by marked hyperreflexia (i.e. left-sided Hoffman’s and Babinski response). The cervical CT and MR scan both documented OPLL extending from C2-C3 to C7-T1 resulting in significant cervical canal stenosis/ cord compression [
Figure 1:
(a) Preoperative T2W sagittal MRI: Marked cervical canal stenosis and cord compression from C2-C3 disc to C7-T1 disc level, predominantly contributed by OPLL with the background of cervical spondylosis. (b) Postoperative T2W sagittal MRI: In addition to an adequately decompressed cervical canal, there is increased signal intensity in the cord with edema opposite at the C3, C6, and C7 levels.
Postoperative course
On postoperative day 1, his strength was 4/5 in the upper, and 5/5 in the lower extremities, and his spasticity had decreased. However, on postoperative day 3, he became acutely quadriparetic (i.e. 2/5 in the left and 3/5 in the right upper extremity, with 4/5 motor function in both lower extremities without an accompanying sensory deficit).
Postoperative imaging
The postoperative MRI documented adequate cord decompression, but new intramedullary cord edema on the T2-weighted image opposite the C3, C6, and C7 levels [
Postoperative management
Once the deficit appeared, the patient was started on high-dose intravenous steroids (Methylprednisolone). NO further surgery was performed (i.e. no surgical lesion was identified on the postoperative MR). The patient regained his preoperative neurological baseline within 7 postoperative days.
DISCUSSION
The WCS is rare following cervical spine surgery. It is characterized by an increased intramedullary cord signal on postoperative T2W MRI scan.[
WCS diagnosis of exclusion
The diagnosis of WCS is one of exclusion; all other potential aetiologies of injury must first be ruled out.[
CONCLUSION
The WCS is a diagnosis of exclusion that only rarely follows cervical spine surgery. However, it is a diagnosis of exclusion, and all other causes of intraoperative and postoperative cord injury must first be ruled out.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Antwi P, Grant R, Kuzmik G, Abbed K. White cord syndrome of acute hemiparesis after posterior cervical decompression and fusion for chronic cervical stenosis. World Neurosurg. 2018. 113: 33-6
2. Chin KR, Seale J, Cumming V. White cord syndrome of acute tetraplegia after anterior cervical decompression and fusion for chronic spinal cord compression: A case report. Case Rep Orthop. 2013. 2013: 697918
3. Epstein NE. Reperfusion injury (RPI)/white cord syndrome (WCS) due to cervical spine surgery: A diagnosis of exclusion. Surg Neurol Int. 2020. 11: 320
4. Liao YX, He SS, He ZM. White cord syndrome, a rare but disastrous complication of transient paralysis after posterior cervical decompression for severe cervical spondylotic myelopathy and spinal stenosis: A case report. Exp Ther Med. 2020. 20: 90
5. Mathkour M, Werner C, Riffle J, Scullen T, Dallapiazza RF, Dumont A. Reperfusion white cord syndrome in cervical spondylotic myelopathy: Does mean arterial pressure goal make a difference? Additional case and literature review. World Neurosurg. 2020. 137: 194-9
6. Papaioannou I, Repantis T, Baikousis A, Korovessis P. Late-onset white cord syndrome in an elderly patient after posterior cervical decompression and fusion: A case report. Spinal Cord Ser Cases. 2019. 5: 28
7. Seichi A, Takeshita K, Kawaguchi H, Nakajima S, Akune T, Nakamura K. Postoperative expansion of intramedullary high-intensity areas on T2-weighted magnetic resonance imaging after cervical laminoplasty. Spine (Phila Pa 1976). 2004. 29: 1478-82
8. Vinodh VP, Rajapathy SK, Sellamuthu P, Kandasamy R. White cord syndrome: A devastating complication of spinal decompression surgery. Surg Neurol Int. 2018. 9: 136
9. Wiginton JG, Brazdzionis J, Mohrdar C, Sweiss RB, Lawandy S. Spinal cord reperfusion injury: Case report, review of the literature, and future treatment strategies. Cureus. 2019. 11: e5279