- Loma Linda University School of Medicine, Loma Linda University Medical Center, California, USA.
- University of Nevada, Reno School of Medicine, Reno, Nevada, USA.
- Department of Otolaryngology–Head and Neck Surgery, Loma Linda University Medical Center, California, USA.
- Department of Pathology, Loma Linda University Medical Center, Loma Linda, California, USA.
Correspondence Address:
Wilson P. Lao
Department of Otolaryngology–Head and Neck Surgery, Loma Linda University Medical Center, California, USA.
DOI:10.25259/SNI_473_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Wilson P. Lao, Jordan M. Thompson, Lauran Evans, Yohanan Kim, Laura Denham, Steve C. Lee. Mixed olfactory neuroblastoma and neuroendocrine carcinoma: An unusual case report and literature review. 09-May-2020;11:97
How to cite this URL: Wilson P. Lao, Jordan M. Thompson, Lauran Evans, Yohanan Kim, Laura Denham, Steve C. Lee. Mixed olfactory neuroblastoma and neuroendocrine carcinoma: An unusual case report and literature review. 09-May-2020;11:97. Available from: https://surgicalneurologyint.com/surgicalint-articles/10013/
Abstract
Background: The aim of the study was to present a case of mixed olfactory neuroblastoma (ONB) and carcinoma, an extremely rare tumor with only a few cases in the published literature.
Case Description: An otherwise healthy 27-year-old male presented with sinus complaints, headache, and unilateral eye discharge. Imaging and endoscopy revealed a mass presumed to represent a juvenile nasopharyngeal angiofibroma. Unexpectedly, the final pathology report revealed high grade mixed ONB and carcinoma. This tumor is the sixth and youngest documented patient with mixed ONB and carcinoma.
Conclusion: Physicians should remain vigilant for the possibility of malignancy in their approach to nasal cavity masses, even in young otherwise healthy patients. Careful review of the immunohistopathology should also be taken, as mixed olfactory tumors such as these are aggressive, rare entities that require multidisciplinary oncologic care.
Keywords: Diagnostic delay, Mixed tumor, Neuroendocrine neoplasm, Olfactory mixed neuroblastoma, Olfactory neuroblastoma
INTRODUCTION
Neuroendocrine neoplasms comprise a rare heterogeneous subset of tumors arising within the head and neck. Sinonasal tumors with neuroendocrine differentiation are of particular interest as its phenomenon is an infrequent occurrence. Classification of sinonasal tumors with neuroendocrine differentiation has been subdivided into neuroectodermal and epithelial origin, of which olfactory neuroblastomas (ONBs) (also known as esthesioneuroblastoma) and neuroendocrine carcinomas manifest, respectively. However, classification and nomenclature remain in constant debate. Although neuroendocrine carcinoma classification is well-established, the current nomenclature and classification of ONBs remains a challenge as its exact origin and histology are unknown partly attributed to a low incidence.[
Age of the diagnosis of ONB is typically between 40 and 70 years old.[
This case report exhibits a young, apparently healthy patient with a diagnosis of mixed ONB and carcinoma. To the best of our knowledge, only 12 cases of combined histopathology have been reported and only five with mixed pathology of this type.[
CASE DESCRIPTION
A 27-year-old male presented to the emergency department (ED) with a right-sided nasal mass and associated progressively worsening lower right eyelid swelling over the course of several months. Medical history was insignificant. His social history was significant for a two pack-year smoking history with additional cocaine and marijuana use. Before his initial presentation, the patient had visited the ED multiple times for symptoms of intermittent epistaxis, sinus congestion, midface pressure, throbbing headaches, and ocular discharge. He had been treated with antibiotics and steroids without improvement. Due to periorbital inflammation, concern for increased intraocular pressure and decreased visual acuity at this ED encounter, the patient underwent a lateral canthotomy and cantholysis by ophthalmology, after which the patients’ eye symptoms improved quickly.
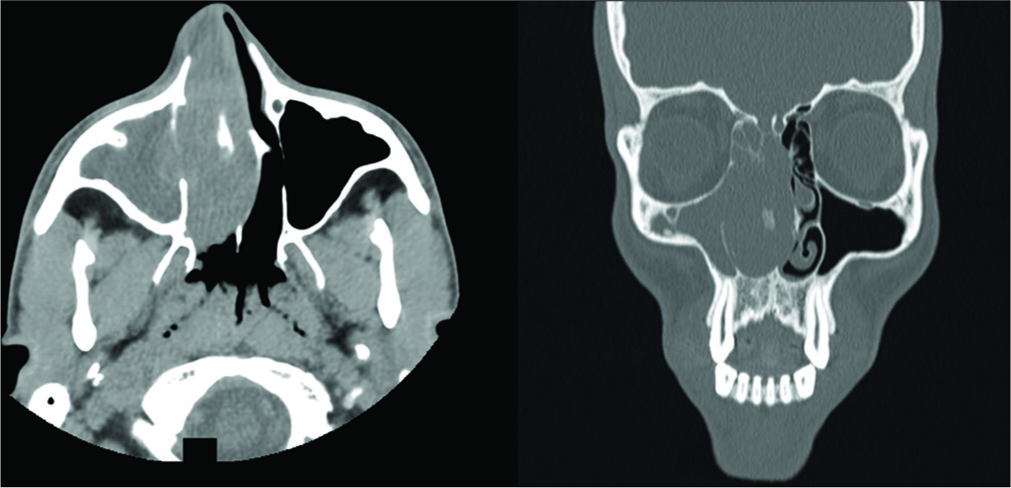
Contrast-enhanced computed tomography (CT) at that time showed a 4.0 × 2.2 cm mass in the right nasal cavity, deviation of the nasal septum to the left, erosion of most of the ethmoidal air cells, and possible extension through the cribriform plate. There was near total opacification of the right frontal sinus, maxillary sinus, and ethmoid air cells with right preseptal soft-tissue edema [
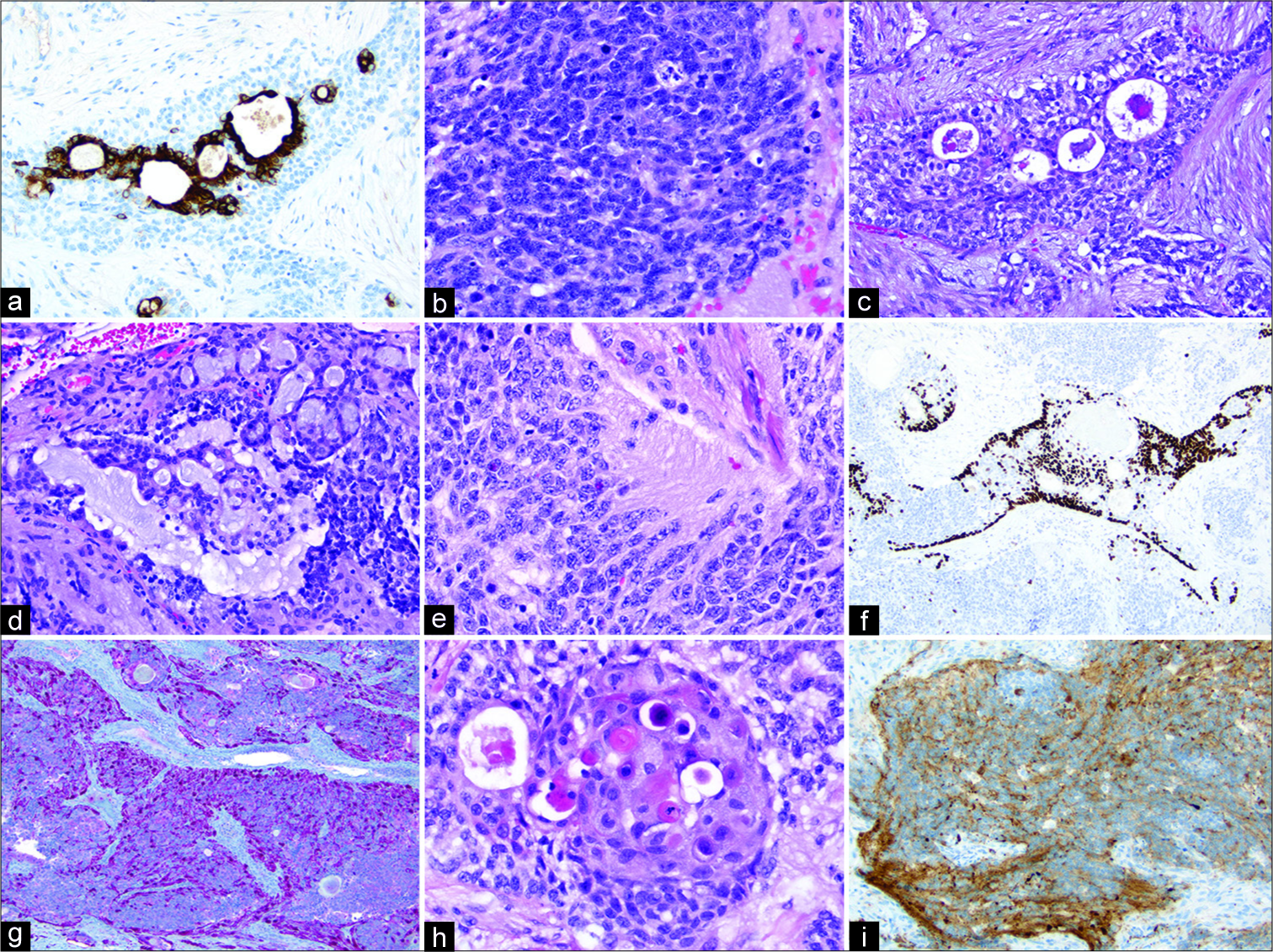
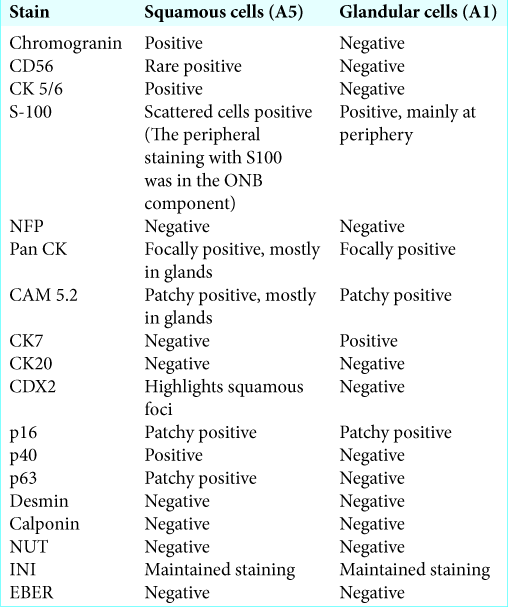
For the treatment of the presumed JNA, otolaryngology performed a right medial maxillectomy, right nasal endoscopy with debridement, total ethmoidectomy, and removal of the intranasal mass. The patient recovered appropriately and was discharged on postoperative day 2. Unexpectedly, the pathology from the right maxilla revealed a high grade malignant neoplasm, most consistent immunophenotypically and histologically with high grade “mixed” ONB and carcinoma [
Figure 2:
(a) CK7 highlights the glandular component ×200, (b) Cytologically the majority of cells have high nuclear to cytoplasmic ratios coarse chromatin and display frequent mitoses and apoptotic bodies H&E ×400, (c) Glandular component corresponding to CK7 image H&E ×200, (d) Glandular component merging into poorly differentiated carcinoma H&E ×200, (e) Neuroblastoma component with neuropil formation H&E ×400, (f) p40 is positive in a subset of cells and is negative in glandular and neuroblastoma components ×200, (g) S100 is positive mainly at the periphery of nests ×100, (h) Squamous component with single cell keratinization H&E ×400, (i) Synaptophysin is positive in majority of cells ×200.
During postoperative follow-up, the patient reported improved right periorbital swelling and erythema, decreased serosanguinous drainage from right nares. No purulent nasal drainage was noted and he remained afebrile. Based on the results of pending magnetic resonance imaging (MRI) and positron emission tomography scans, the patient is expected to undergo further resection of residual tumor versus chemotherapy and radiation.
DISCUSSION
ONB is itself a rare entity. Therefore, the presence of a histologically mixed tumor is noteworthy. Cases of mixed neuroendocrine with nonneuroendocrine tumors have been previously reported 12 times,[
This patient was diagnosed with JNA based on his presenting symptoms, imaging, exam, and age. However, a few features of this case are unusual for JNA in retrospect. First, the patient’s age is somewhat advanced for JNA, although reports of JNA in older patients and even in an elderly female have been reported.[
Of reported cases, ONBs make up <5% of malignant tumors found in the nasal fossa and paranasal sinuses.[
Common presenting symptoms in ONBs throughout the literature include epistaxis, nasal obstruction, anosmia, headache, rhinorrhea, lacrimation, visual disturbances, and SIADH.[
The diagnostic protocol of ONB begins with a histologically confirmed positive biopsy usually, followed by classification. However, the classification of these tumors continues to remain in debate. At present, the Kadish clinical system appears to be the most commonly used classification system for ONBs, apart from traditional tumor-node-metastasis, Dulguerov, and Hyams classification systems.[
In the previous series, intended curative surgical resection with an endoscopic approach was performed on patients with ONBs regardless of staging. Although surgery is still considered first-line treatment, multidisciplinary management of such tumors is crucial. Grandhoke et al.’s patient did not undergo adjuvant radiation or chemotherapy and had a fast-growing recurrence only 2 months after total resection.[
CONCLUSION
Providers should be aware of this rare sinonasal mixed neuroendocrine malignancy and the management of such a histologically diverse tumor. In addition, diagnostic caution should be practiced when considering a sinonasal mass in a young adult, as more aggressive malignancies may mimic benign conditions such as JNA. Finally, further studies are necessary to develop a more standard classification system and treatment modality.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bartel R, Gonzalez-Compta X, Cisa E, Cruellas F, Torres A, Rovira A. Importance of neoadjuvant chemotherapy in olfactory neuroblastoma treatment: Series report and literature review. Acta Otorrinolaringol Esp. 2018. 69: 208-13
2. Bell D. Sinonasal neuroendocrine neoplasms: Current challenges and advances in diagnosis and treatment, with a focus on olfactory neuroblastoma. Head Neck Pathol. 2018. 12: 22-30
3. Caldwell NJ, Sato TS. Ectopic primary olfactory neuroblastoma of the nasopharynx: A case report and review of the literature. Radiol Case Rep. 2019. 14: 997-1002
4. Gandhoke CS, Dewan A, Gupta D, Syal SK, Jagetia A, Saran RK. A rare case report of mixed olfactory neuroblastoma: Carcinoma with review of literature. Surg Neurol Int. 2017. 8: 83-
5. Hyams VJ, Batsakis JG, Michaels L.editors. Tumors of the Upper Respiratory Tract and Ear, Atlas of Tumor Pathology. Washington DC: Armed Forces Institute Press; 1988. Vol. 25: 240-8
6. Joshi RR, Husain Q, Roman BR, Cracchiolo J, Yu Y, Tsai J. Comparing Kadish, TNM, and the modified dulguerov staging systems for esthesioneuroblastoma. J Surg Oncol. 2019. 119: 130-42
7. Kadish S, Goodman M, Wang CC. Olfactory neuroblastoma. A clinical analysis of 17 cases. Cancer. 1976. 37: 1571-6
8. Meyer C, Hamersley ER, Manosalva RE, Torske K, McIntyre N, Mitchell A. Olfactory neuroblastoma with divergent differentiation: An unusual histologic finding in a rare tumor. Head Neck Pathol. 2017. 11: 531-6
9. Miller DC, Goodman ML, Pilch BZ, Shi SR, Dickersin GR, Halpern H. Mixed olfactory neuroblastoma and carcinoma. A report of two cases. Cancer. 1984. 54: 2019-28
10. Ralli M, Fusconi M, Visconti IC. Nasopharyngeal angiofibroma in an elderly female patient: A rare case report. Mol Clin Oncol. 2018. 9: 702-4
11. Shah K, Perez-Ordóñez B. Neuroendocrine neoplasms of the sinonasal tract: Neuroendocrine carcinomas and olfactory neuroblastoma. Head Neck Pathol. 2016. 10: 85-94
12. Hermsen MA, Riobello C, Garcia-Marin R, Cabal VN, Suarez-Fernandez L, Lopez F. Translational genomics of sinonasal cancers. Semin Cancer Biol. 2020. 61: 101-9