- Department of Neurosurgery, King Saud University Medical City, College of Medicine, King Saud University, Riyadh, Saudi Arabia
- Medical Intern, College of Medicine, King Saud University, Riyadh, Saudi Arabia
- Department of Neurosurgery, King Saud University Medical City, Riyadh, Saudi Arabia
- Medical student, College of Medicine, King Saud University, Riyadh, Saudi Arabia
- Medical student, College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
- Department of Radiology, King Saud University Medical City, Riyadh, Saudi Arabia.
- Department of Pathology, King Saud University Medical City, Riyadh, Saudi Arabia.
Correspondence Address:
Ali A. Basalamah, Department of Neurosurgery, King Saud University Medical City, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_536_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fawaz S. Almotairi1, Alwaleed Abdulrahman Alsaleh2, Ali A. Basalamah3, Mohannad M. Mallat4, Emad M. Babateen5, Ali Abdu6, Saeed O. Bahabri7. Mixed pyogenic and tuberculous spinal epidural abscesses perforating the dura and extending into the subdural space: A case report and review of the literature. 08-Sep-2023;14:315
How to cite this URL: Fawaz S. Almotairi1, Alwaleed Abdulrahman Alsaleh2, Ali A. Basalamah3, Mohannad M. Mallat4, Emad M. Babateen5, Ali Abdu6, Saeed O. Bahabri7. Mixed pyogenic and tuberculous spinal epidural abscesses perforating the dura and extending into the subdural space: A case report and review of the literature. 08-Sep-2023;14:315. Available from: https://surgicalneurologyint.com/surgicalint-articles/12542/
Abstract
Background: Spinal infections are associated with a wide variety of clinical conditions, including osteomyelitis, spondylitis, diskitis, septic facet joints, and abscesses. Based on its anatomical relationship with the dura mater, the abscess can be epidural (extradural) or subdural (intrathecal). Subdural intramedullary abscesses of the lumbar spinal canal are more common than subdural extramedullary abscesses. Here, we present a rare case of a patient with a mixed pyogenic and tuberculous epidural abscess in the lumbar spine, which perforated the dura and extended to the subdural space.
Case Description: A 29-year-old male presented with progressively worsening back pain and lower-limb weakness over a period of 3 months, with an associated inability to walk, intermittent radicular pain primarily on the left side, intermittent incontinence, and a history of low-grade fever and night sweats. The patient had a history of intravenous (IV) drug abuse and reported practicing unprotected sexual intercourse. Furthermore, the patient had recently came into contact with a person diagnosed with tuberculosis (TB). The patient was administered empirical broad-spectrum antibiotics and underwent emergent L4–L5 laminectomy and spinal abscess decompression. IV antibiotics were selected based on culture results, and anti-TB medications were started. Postoperatively, the patient demonstrated a remarkable lower-limb power improvement and radicular pain alleviation.
Conclusion: Spinal epidural abscess perforation of the dura and extension into the subdural space is extremely rare. Distinguishing between epidural and subdural abscesses radiologically is challenging. Multiple risk factors, such as unprotected sexual contact and IV drug misuse, may be associated with the development of polymicrobial abscesses in the lumbar spine. Careful anticipation, identification, and isolation of the causative micro-organisms can ensure effective antibacterial treatment. Early diagnosis, expeditious surgical decompression, and antibiotic treatment are associated with promising outcomes.
Keywords: Epidural abscess, Pyogenic spinal infection, Spinal infection, Spinal tuberculosis, Subdural abscess
INTRODUCTION
Spinal infections are rare and are associated with several clinical manifestations, including, but not limited to, osteomyelitis, spondylitis, diskitis, septic facet joints, and abscesses. These may be caused by hematogenous seeding, dissemination from infected contagious tissue, or direct inoculation during surgery or trauma.[
Spinal canal abscess is a well-described sequela of spondylitis and spondylodiscitis[
Staphylococcus aureus is the most frequent cause of spinal infections, accounting for more than 50% of cases. In contrast, Mycobacterium tuberculosis accounted for <25% of the cases. Almost half of skeletal tuberculosis (TB) cases occur in the spine. The thoracolumbar junction is the most affected area in the spine, followed by the lumbar and cervical spine.[
Here, we present the rare case of a 29-year-old male with a mixed pyogenic and tuberculous lumbar epidural abscess that perforated the dura into the subdural space.
CASE DESCRIPTION
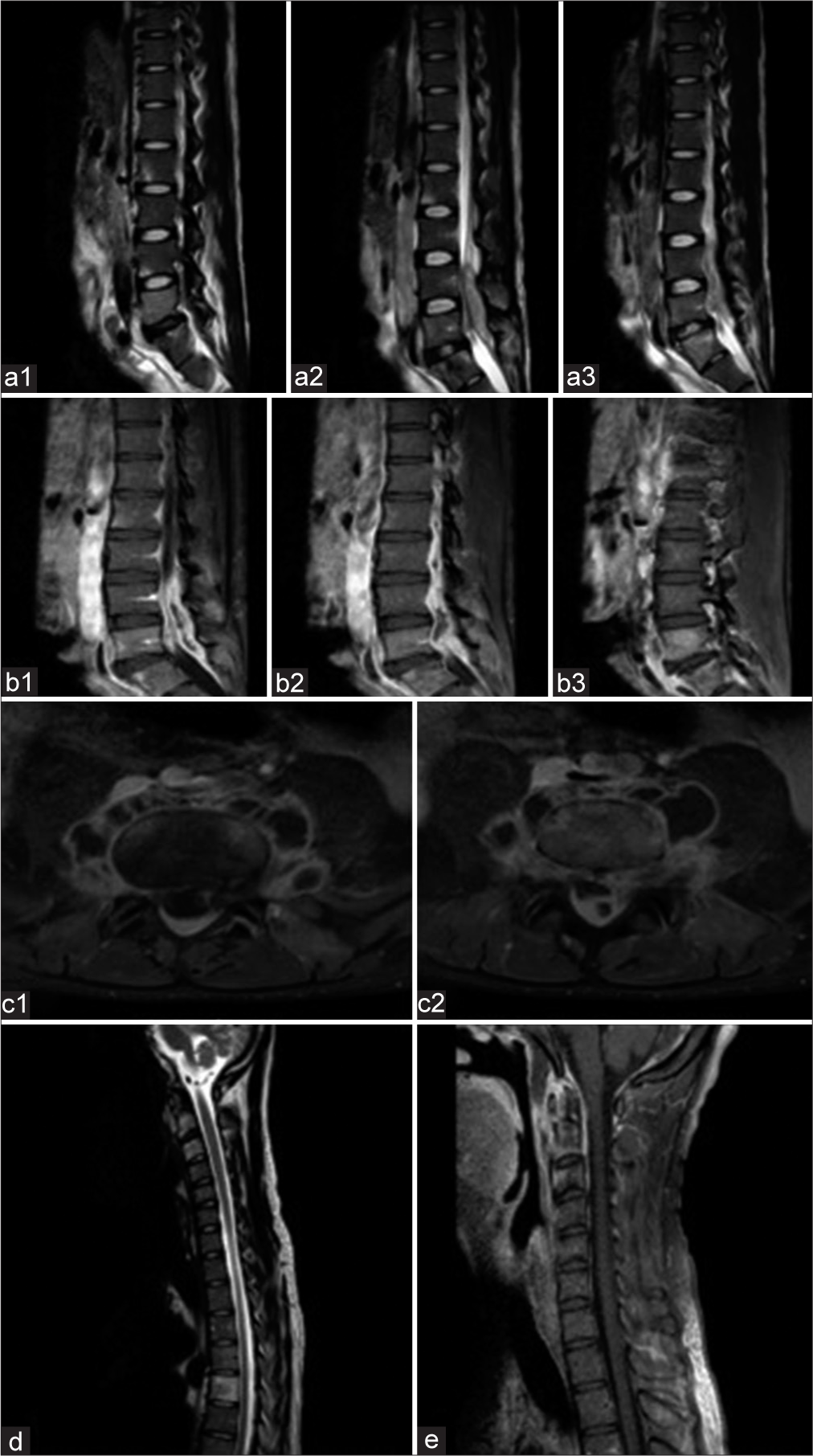
A 29-year-old male presented with progressive lower back pain, left lower-limb radicular pain, lower-limb weakness, and inability to walk associated with intermittent incontinence over a period of 3 months. The patient reported a history of low-grade fever and nighttime sweats. There was a history of IV drug abuse and recent unprotected sexual intercourse. Furthermore, the patient had a recent contact with a person diagnosed with TB. Clinical examination was remarkable for moderate to severe back pain associated with lower-limb weakness (2–3/5 power): right > left, pinprick sensation was decreased on the left side from L2 to S1, joint position sensation was intact, reflexes were decreased (+1), and rectal tone was normal. White blood cell count was normal but inflammatory marker levels were elevated (erythrocyte sedimentation rate [ESR], 120). Blood culture results were negative. Preoperative computed tomography (CT) and MRI revealed sternoclavicular joint arthritis, left fourth anterior rib infection with a pathological fracture, and multilevel early disc dehydration. Moreover, at the L4/L5 level, there was a 4.5 × 1.2 × 0.8 cm intradural, extramedullary bright T2 and bright Tl signal intensity lesion with low internal T2 signals, which was compressing the filum terminale anteriorly. There was associated underlying bone scalloping. At the same level, there was a partially imaged tubular branching, abnormal bright T2/fluid signal with an epicenter at the neural foramina encircling the L4 and L5 vertebral bodies anteriorly [
Figure 1:
Radiology: Spondylodiscitis with epidural and paraspinal abscess. (a1-a3) Sagittal T2WI of the lumbar spine shows multiple abnormal marrow signals involving the vertebral body and endplates of L2, L4, L5, and S1 with disc degeneration at L5/S1. There is an associated abnormal large ventral and dorsal epidural and paraspinal components compressing the thecal sac and cauda equina nerve roots. Sagittal (b1-b3) and axial (c1 and c2) WI show abnormal post contrast enhancement of the vertebral bodies and end-plated and marginal enhancement of the large epidural and paraspinal abscesses with extension against the neural foramen. (d) Sagittal T2WI of the cervical spine shows abnormal signal intensity of the upper cervical spine C2/3 and T5 suggesting noncontiguous infection. (e) A sagittal post contrast study shows abnormal vertebral with associated mild prevertebral and ventral epidural enhancement suggesting an infective process.
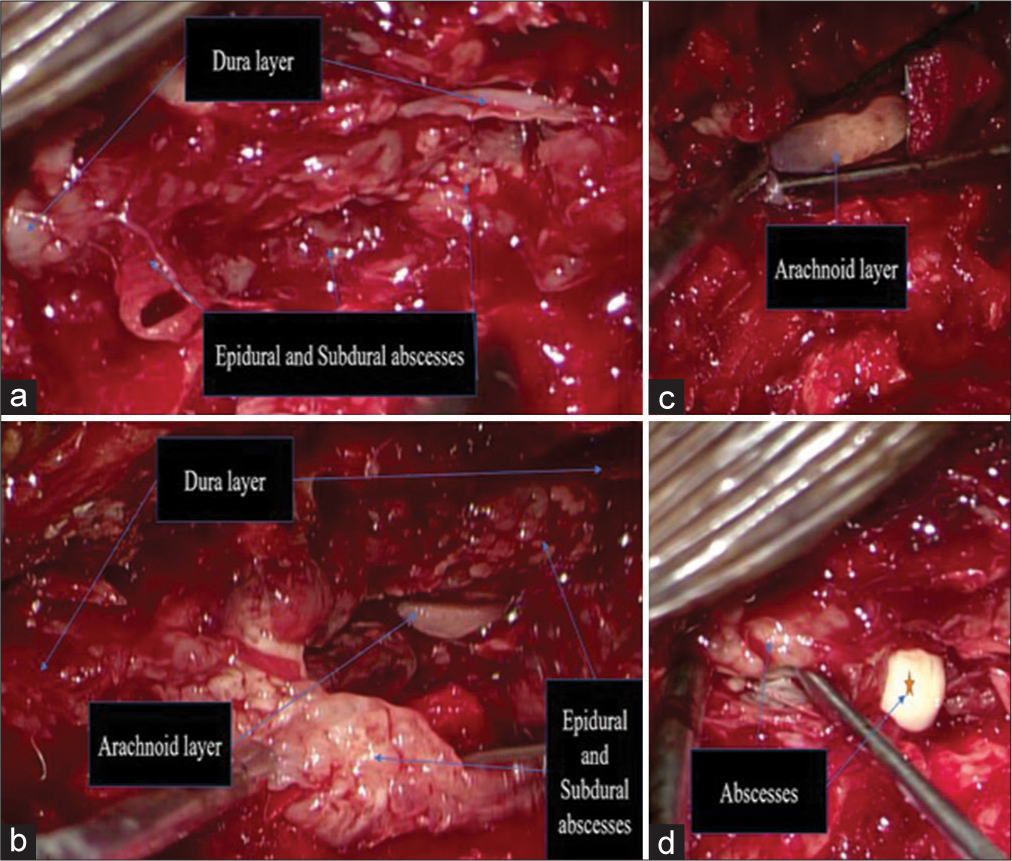
Empirical broad-spectrum antibiotics were initiated, and the patient underwent emergency L4–L5 decompression. The infiltrated bone was weak and brittle, with some sclerotic areas. The ligamentum flavum was thickened and infected. The epidural collection was multilayered and lobulated. Nonpurulent phlegmon was noted. In other areas, there was a white-yellow purulent fluid discharge within a thin encapsulated membrane. Phlegmon/abscess in the epidural space was observed. The abscess perforated the dura and was dissecting intradurally (within the subdural space). The dura was thick and inflamed. In addition, a paraspinal muscle abscess extension noted [
Figure 2:
(a and b) Epidural and subdural multi-layered inflamed nonpurulent soft-tissue/phlegmon perforating the dura and extending into the subdural space. (b and c) A thick, inflamed, and intact arachnoid layer. (d) White-yellow liquor puris purulent fluid pus discharge contained within a thin encapsulated membrane.
The abscess was grossly removed. Notably, the arachnoid layer was thick, inflamed, and intact. Hemostasis was achieved after adequate decompression and sampling. The dura was sealed using gel foam, along with TachoSil and TISSEL. A drain was inserted. The fascia was closed water-tight using 2.0 Vicryl. The subcutaneous layer was closed using 2.0 Vicryl while the skin was sealed with staples. The patient was shifted to the recovery unit and had no complications.
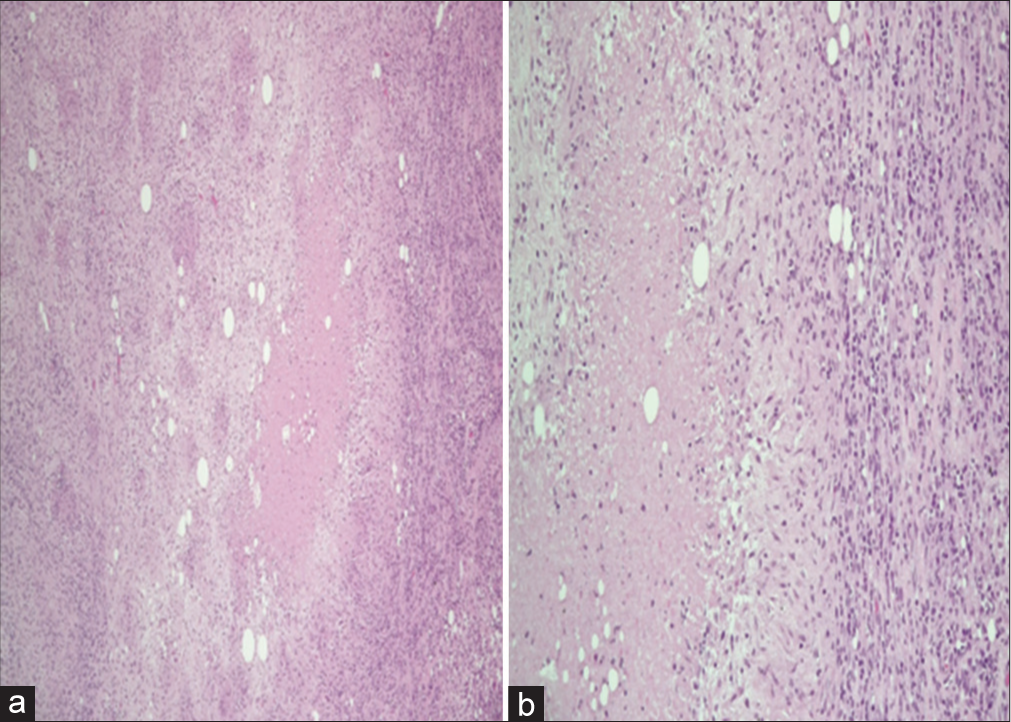
The tissue cultures were positive for Enterobacter cloacae, Citrobacter koseri, and Staphylococcus epidermidis. The result of the QuantiFERON-TB test was positive. The final surgical pathology revealed a well-formed necrotizing (caseating) granuloma with central necrosis surrounded by epithelioid histiocytes and lymphocytes. Acid-fast bacilli (AFB) were negative for Mycobacterium [
Figure 3:
Pathology: low power ×4 (a) and high power ×20 (b), shows a well-formed necrotizing (caseating) granuloma with central necrosis, surrounded by epithelioid histiocyte and lymphocyte. Special stains (not shown here) for Mycobacterium [Ziehl-Neelsen stain (ZN)] and fungal infection [Grocott methenamine silver (GMS) stain] are negative (these studies are for screening purposes. Negativity for these stains does not rule out the possibility of such infection).
IV antibiotics were selected based on the culture report, and anti-TB medications were initiated. Postoperatively, the patient demonstrated a remarkable lower-limb power improvement and back/radicular pain alleviation.
DISCUSSION
Intradural extension of a SEA is a rare phenomenon with unknown incidence.[
Vertebral infections are frequently hematogenous. In pyogenic spinal infections, the vertebral endplate is first infected and subsequently, associated with early disc involvement and destruction. However, TB infection results from venous spread through Batson’s paravertebral venous plexus. In spinal TB, the initial destruction involves the anterior inferior aspect of the vertebra. Subsequently, subligamentous spread to the adjacent vertebra by skipping the disc at the early stages of infection.[
Classically, spinal TB is a granulomatous inflammation resulting from the aggregation of lymphocytes in the affected tissue leading to the formation of a caseating granuloma, also known as a cold abscess. Granulomas are formed by aggregates of histiocytes or macrophages mixed with variable numbers of inflammatory cells, with or without giant cells. It can have infectious or noninfectious etiologies, the identification of which is key to treatment and prognosis. Underlying etiologies include infections, sarcoidosis, hematologic and nonhematologic malignancies, drug reactions, autoimmune diseases, and other disorders. Two common histological findings are caseating or noncaseating granulomas. Histopathological features are not reliable for differentiating between causes, and it is necessary to combine morphology with microbiological, serological, molecular, and clinical findings for accurate interpretation. Histopathologically, a caseating/necrotizing granuloma containing a central area of necrosis (caseation) surrounded by epithelioid histiocytes and lymphocytes is observed, and immunohistochemistry results are positive for cluster of differentiation (CD)68 and CD163, thereby highlighting the cluster of histiocytes. AFB is positive for mycobacterial infections while Grocott’s methenamine silver is positive for fungal infections.[
This case illustrates a rare finding of an aggressive, mixed pyogenic, and tuberculous epidural abscess in the lumbar spine that perforated the dura into the subdural space. To the best of our knowledge, this phenomenon has been described in only a few cases in the literature.[
Conservative management, including bed brace, analgesics, appropriate antibiotic coverage, and spinal immobilizing brace, resulted in 90% of infection eradication and pain control.[
CONCLUSION
Spinal epidural perforation of the dura and extension into the subdural space is an extremely rare phenomena. Distinguishing between epidural and subdural abscesses radiologically is challenging. Multiple risk factors, such as unprotected sexual contact and IV drug misuse, may be associated with the development of polymicrobial abscesses in the lumbar spine. Careful anticipation, identification, and isolation of the causative micro-organisms can ensure effective antibacterial treatment. Early diagnosis, expeditious surgical decompression, and antibiotic treatment are associated with promising outcomes.
Ethics
In conducting and reporting this case study, we have adhered to ethical standards, ensuring that the welfare of the patient and their privacy has been prioritized throughout the process. All efforts have been made to ensure the anonymity and confidentiality of the patient involved in this case report and any potentially identifying information has been removed.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology to assist in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akalan N, Ozgen T. Infection as a cause of spinal cord compression: A review of 36 spinal epidural abscess cases. Acta Neurochir (Wien). 2000. 142: 17-23
2. Ameer MA, Knorr TL, Munakomi S, Mesfin FB, editors. Spinal epidural abscess. StatPearls. Treasure Island, FL: StatPearls; 2023. p.
3. Bond A, Manian FA. Spinal epidural abscess: A review with special emphasis on earlier diagnosis. Biomed Res Int. 2016. 2016: 1614328
4. Danner RL, Hartman BJ. Update on spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 1987. 9: 265-74
5. Du JY, Schell AJ, Kim CY, Trivedi NN, Ahn UM, Ahn NU. 30-day mortality following surgery for spinal epidural abscess: Incidence, risk factors, predictive algorithm, and associated complications. Spine (Phila Pa 1976). 2019. 44: E500-9
6. Fotaki A, Anatoliotaki M, Tritou I, Tzagaraki A, Kampitaki M, Vlachaki G. Review and case report demonstrate that spontaneous spinal epidural abscesses are rare but dangerous in childhood. Acta Paediatr. 2019. 108: 28-36
7. Garg RK, Somvanshi DS. Spinal tuberculosis: A review. J Spinal Cord Med. 2013. 34: 440-54
8. Issa K, Pourtaheri S, Stewart T, Faloon M, Sahai N, Mease S. Clinical differences between monomicrobial and polymicrobial vertebral osteomyelitis. Orthopedics. 2017. 40: e370-3
9. Lee KY. Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian Spine J. 2014. 8: 216-23
10. Levy ML, Wieder BH, Schneider J, Zee CS, Weiss MH. Subdural empyema of the cervical spine: Clinicopathological correlates and magnetic resonance imaging. Report of three cases. J Neurosurg. 1993. 79: 929-35
11. Nussbaum ES, Rigamonti D, Standiford H, Numaguchi Y, Wolf AL, Robinson WL. Spinal epidural abscess: A report of 40 cases and review. Surg Neurol. 1992. 38: 225-31
12. Rosinsky PJ, Zimhony O, Ciobotaro P, Sagiv S, Ben-Galim P. Intradural extension of a pyogenic epidural abscess: A case report. JBJS Case Connect. 2015. 5: e76
13. Smith C, Crawford CH, Dimar J. Spinal epidural abscess: A review of diagnosis and treatment. Curr Orthop Pract. 2014. 25: 29-33
14. Tanriverdi T, Kizilkiliç O, Hanci M, Kaynar MY, Unalan H, Oz B. Atypical intradural spinal tuberculosis: Report of three cases. Spinal Cord. 2003. 41: 403-9
15. Tsantes AG, Papadopoulos DV, Vrioni G, Sioutis S, Sapkas G, Benzakour A. Spinal infections: An update. Microorganisms. 2020. 8: 476
16. Vural M, Arslantaş A, Adapinar B, Kiremitçi A, Usluer G, Cuong B. Spinal subdural Staphylococcus aureus abscess: Case report and review of the literature. Acta Neurol Scand. 2005. 112: 343-6