- Department of Neurosurgery, Banha University, Banha, Egypt,
- Department of Neurosurgery, der Barmherzigen Brüder Hospital, Trier, Germany.
Correspondence Address:
Mohammed Ahmed Mourad, Department of Neurosurgery, Banha University, Banha, Egypt.
DOI:10.25259/SNI_707_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammed Ahmed Mourad1, Andy Ottenbacher2, Ahmed R. Rizk2. Modified anterior transarticular C1/2 fixation for odontoid fractures: An approach with high complication rate in geriatric population. 07-Oct-2022;13:457
How to cite this URL: Mohammed Ahmed Mourad1, Andy Ottenbacher2, Ahmed R. Rizk2. Modified anterior transarticular C1/2 fixation for odontoid fractures: An approach with high complication rate in geriatric population. 07-Oct-2022;13:457. Available from: https://surgicalneurologyint.com/surgicalint-articles/11921/
Abstract
Background: In patients over 75 years of age, we applied a modified anterior transarticular C1/2 fixation with reduced pharyngeal mobilization versus the standard anterior triple/quadruple osteosynthesis procedures.
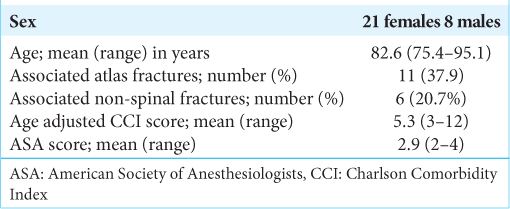
Methods: From 2010 to 2018, 29 patients underwent a modified anterior transarticular C1/2 fixation utilizing single odontoid screw fixation through a right-sided Smith-Robinson – (i.e., short and steep screw trajectory for the right and long trajectory for the left side) approach. All the patients were 75 years of age or older (mean age 82.6) and had sustained odontoid Type II fractures. In addition, a subset exhibited further ligamentous injuries and/or atlas fractures. Their Mean Age-adjusted Charlson Comorbidity Index was 5.3 points (range 3–12), while mean American Society of Anesthesiologists scores averaged 2.9 (range 2–4).
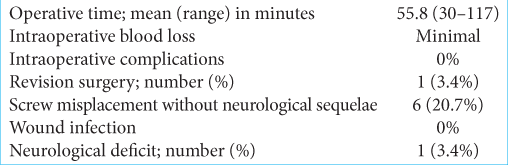
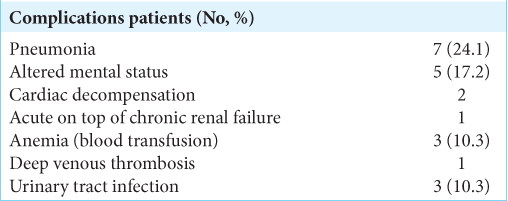
Results: The mean operating time was 55.8 min, there were no intraoperative complications, and there was minimal blood loss in all cases. The most common medical complications included aspiration pneumonia (24.1%, n = 7), altered mental status (17.2%, n = 5), and cardiac decompensation (6.9%, n = 2). One patient with delayed dysphagia and an infected implant resulting in loosening/dislocation required implant removal and long-term antibiotic therapy. The 30-day mortality rate was 13.8% (four patients) and the 1-year mortality rate was 27.6% (eight patients).
Conclusion: Anterior transarticular C1/2/odontoid fixation with reduced pharyngeal mobilization and shorter operative times was associated with high morbidity/mortality rates. Dysphagia/aspiration was the major postoperative complications leading to some deaths especially in patients with dementia/Parkinsonism.
Keywords: Geriatric population, Odontoid fractures, Transarticular C1/2 fixation
INTRODUCTION
Odontoid fractures, representing only 9–15% of all cervical spine fractures, are more common in the elderly population (i.e., largely Type II fractures in patients over 75 years of age). [
MATERIALS AND METHODS
We performed modified anterior transarticular C1/C2 fixations for Type II odontoid fractures in 29 patients who averaged 82.6 years of age (i.e., all over 75 years old, between 2010 and 2018). We used a right-sided Smith-Robinson-approach and a short/right steep screw trajectory with a long left-sided screw trajectory. Factors studied included medical comorbidities (Age-adjusted Charlson Comorbidity Index [CCI: mean 5.3 points]; American Society of Anesthesiologists [ASA: mean 2.9 points: 20 severe and nine mild systemic disease]), neurologic deficits, and 30-day/1-year survival rates [
Etiology of Type II fractures in 29 patients
Fractures were attributed to fall in all 29 patients; fall from a standing position (27 patients) one patient fell from a ladder, and another fell during mountain climbing. Eleven patients (37.9%) had associated atlas fractures; 6 (20.7%) of the 11 had attendant Jeffereson fractures. Six other patients had nonspinal fractures [
RESULTS
Surgery-related complications
All 29 patients sustained no intraoperative complications. Further, the intraoperative blood loss was minimal [
Mortality
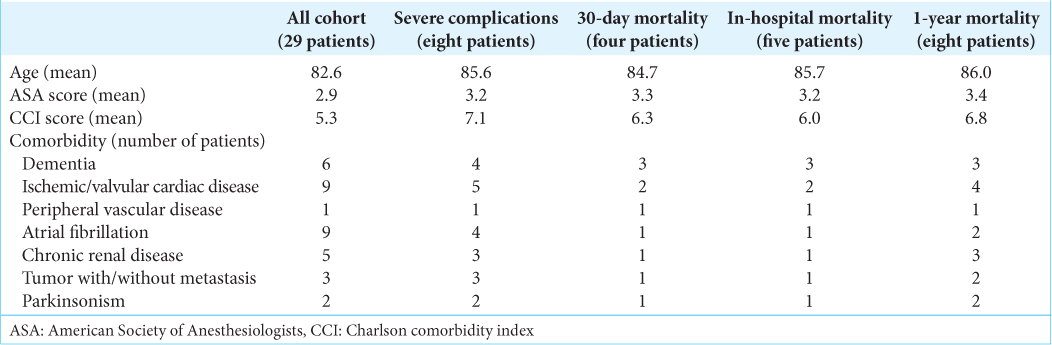
The 30-day mortality rate was 13.8% (n = 4), due to pneumonia [three patients] and heart failure [one patient]. However, one more patient died as a result of pneumonia occurring on the 32nd postoperative day [i.e., total in-hospital mortality rate was 17.2% [n = 5]). The 1-year mortality rate was 27.6% (n = 8). The mean ASA and CCI scores in these cases were higher versus the remaining cohort. Further the probability of severe complications was higher in patients with dementia, cardiac diseases, peripheral vascular disease, Parkinsonism, and chronic renal disease. In addition, early mortality was highest among those with peripheral vascular disease (100%), dementia (50%), Parkinsonism (50%), and tumors (33%) [
DISCUSSION
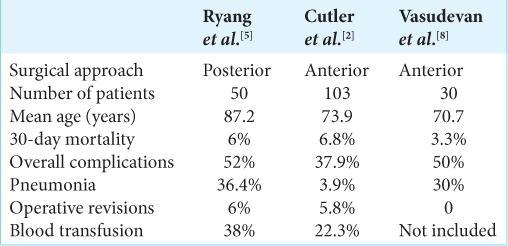
Our 29 patients with Type II odontoid fractures over the age of 75 warranted surgical C1/C2 odontoid fixation. Dysphagia is one of the leading causes of perioperative morbidity in odontoid fractures in the elderly especially following anterior approach due to manipulation of the pharynx/esophagus during placement of the screws.[
CONCLUSION
Despite utilizing a modified anterior transarticular C1/2/ odontoid fixation technique in 29 patients over 75 years of age, involving less pharyngeal mobilization/shorter operative times, there were still high 30-day and 1-year postoperative morbidity/mortality rates.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Amling M, Posl M, Wening VJ, Ritzel H, Hahn M, Delling G. Structural heterogeneity within the axis: The main cause in the etiology of dens fractures. A histomorphometric analysis of 37 normal and osteoporotic autopsy cases. J Neurosurg. 1995. 83: 330-5
2. Cutler HS, Guzman JZ, Lee NJ, Kothari P, Kim JS, Shin JI. Short-term complications of anterior fixation of odontoid fractures. Glob Spine J. 2018. 8: 47-56
3. Herren C, Pishnamaz M, Lichte P, Hildebrand F, Sellei RM, Pape HC. The anterior “Triple-/Quadruple” technique for C1/C2 Trauma in the elderly: First experience with 16 patients. Z Orthop Unfall. 2015. 153: 533-9
4. Hsu WK, Anderson PA. Odontoid fractures: Update on management. J Am Acad Orthop Surg. 2010. 18: 383-94
5. Ryang YM, Török E, Janssen I, Reinke A, Buchmann N, Gempt J. Early morbidity and mortality in 50 very elderly patients after posterior atlantoaxial fusion for traumatic odontoid fractures. World Neurosurg. 2016. 87: 381-91
6. Schroeder GD, Kepler CK, Kurd MF, Paul JT, Rubenstein RN, Harrop JS. A systematic review of the treatment of geriatric Type II odontoid fractures. Neurosurgery. 2015. 77: S6-14
7. Tian NF, Hu XQ, Wu LJ, Wu XL, Wu YS, Zhang XL. Pooled analysis of non-union, re-operation, infection, and approach related complications after anterior odontoid screw fixation. PLoS One. 2014. 9: e103065
8. Vasudevan K, Grossberg JA, Spader HS, Torabi R, Oyelese AA. Age increases the risk of immediate postoperative dysphagia and pneumonia after odontoid screw fixation. Clin Neurol Neurosurg. 2014. 126: 185-9
9. Watanabe M, Sakai D, Yamamoto Y, Nagai T, Sato M, Mochida J. Analysis of predisposing factors in elderly people with Type II odontoid fracture. Spine J. 2014. 14: 861-6