- Department of Neurousrgery, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
Correspondence Address:
Nancy E. Epstein
Department of Neurousrgery, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
DOI:10.4103/2152-7806.174895
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Epstein NE. More nerve root injuries occur with minimally invasive lumbar surgery, especially extreme lateral interbody fusion: A review. Surg Neurol Int 25-Jan-2016;7:
How to cite this URL: Epstein NE. More nerve root injuries occur with minimally invasive lumbar surgery, especially extreme lateral interbody fusion: A review. Surg Neurol Int 25-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/more-nerve-root-injuries-occur-with-minimally-invasive-lumbar-surgery-especially-extreme-lateral-interbody-fusion-a-review/
Abstract
Background:In the lumbar spine, do more nerve root injuries occur utilizing minimally invasive surgery (MIS) techniques versus open lumbar procedures? To answer this question, we compared the frequency of nerve root injuries for multiple open versus MIS operations including diskectomy, laminectomy with/without fusion addressing degenerative disc disease, stenosis, and/or degenerative spondylolisthesis.
Methods:Several of Desai et al. large Spine Patient Outcomes Research Trial studies showed the frequency for nerve root injury following an open diskectomy ranged from 0.13% to 0.25%, for open laminectomy/stenosis with/without fusion it was 0%, and for open laminectomy/stenosis/degenerative spondylolisthesis with/without fusion it was 2%.
Results:Alternatively, one study compared the incidence of root injuries utilizing MIS transforaminal lumbar interbody fusion (TLIF) versus posterior lumbar interbody fusion (PLIF) techniques; 7.8% of PLIF versus 2% of TLIF patients sustained root injuries. Furthermore, even higher frequencies of radiculitis and nerve root injuries occurred during anterior lumbar interbody fusions (ALIFs) versus extreme lateral interbody fusions (XLIFs). These high frequencies were far from acceptable; 15.8% following ALIF experienced postoperative radiculitis, while 23.8% undergoing XLIF sustained root/plexus deficits.
Conclusions:This review indicates that MIS (TLIF/PLIF/ALIF/XLIF) lumbar surgery resulted in a higher incidence of root injuries, radiculitis, or plexopathy versus open lumbar surgical techniques. Furthermore, even a cursory look at the XLIF data demonstrated the greater danger posed to neural tissue by this newest addition to the MIS lumbar surgical armamentariu. The latter should prompt us as spine surgeons to question why the XLIF procedure is still being offered to our patients?
Keywords: Extreme lateral interbody fusions (XLIF), minimally invasive surgery (MIS), nerve root injuries: lumbar surgery, percutaneous procedures, posterior lumbar interbody fusion (PLIF), posterolateral fusions (PLF), transforaminal lumbar interbody fusion (TLIF)
INTRODUCTION
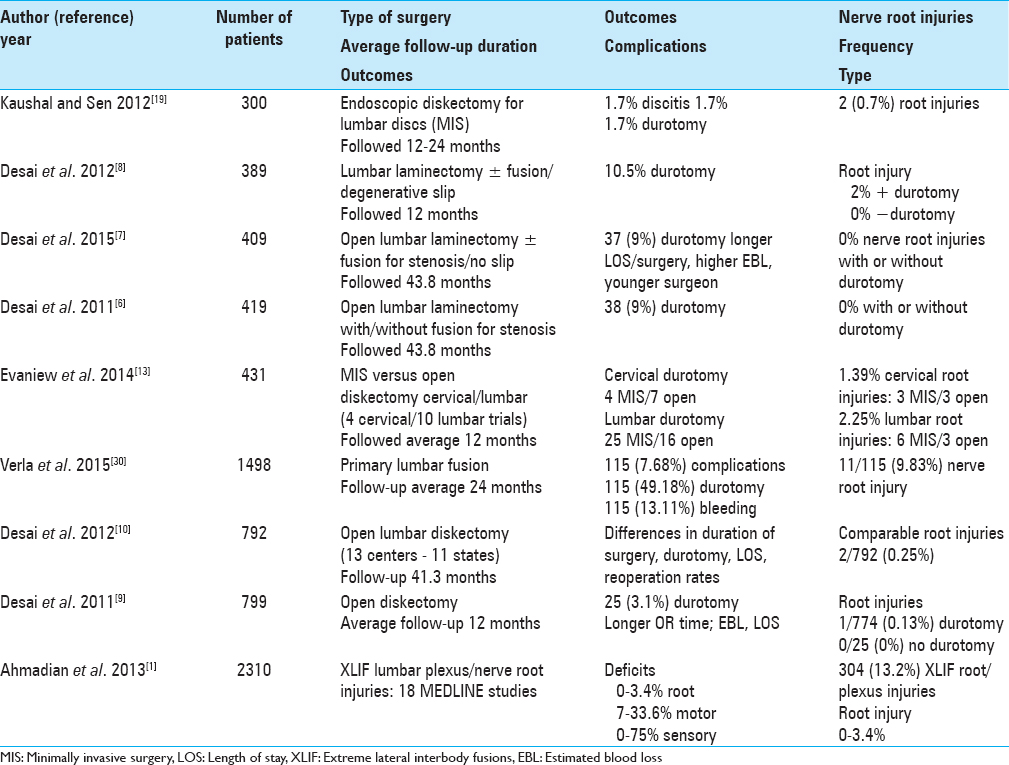
In the lumbar spine, do more nerve root injuries occur utilizing minimally invasive surgery (MIS) techniques versus open lumbar procedures? To answer this question, we compared the frequency of nerve root injuries for multiple open versus MIS operations including diskectomy, laminectomy with/without fusion addressing degenerative disc disease, stenosis, and/or degenerative spondylolisthesis [Tables
Desai et al. large Spine Patient Outcomes Research Trial (SPORT) studies showed the frequency for nerve root injury following an open diskectomy ranged from 0.13% to 0.25%, for open laminectomy/stenosis with/without fusion it was 0%, and for open laminectomy/stenosis/degenerative spondylolisthesis with/without fusion it was 2% [
This review of open versus MIS lumbar surgical studies variously addressing degenerative lumbar disc disease, stenosis, stenosis/spondylolisthesis, indicates a higher overall incidence of root injuries, radiculitis, or plexopathy utilizing MIS approaches. Furthermore, the addition of BMP-2 to lumbar fusions (off-label) correlated with nearly a 50% frequency of new postoperative root-related complaints. After performing this analysis we then question, where is the value added for many of these MIS techniques? Certainly, even a cursory look at the XLIF demonstrates its significant threat to neural tissue. Should not we, therefore, reconsider whether it should remain part of the MIS lumbar surgical armamentarium? After all, we as spine surgeons must use our cumulative knowledge to question and change the procedures being offered to our patients.
NERVE ROOT COMPLICATIONS OF OPEN LUMBAR SURGERY
Nerve root complications of open lumbar stenosis surgery
Spine Patient Outcomes Research Trial: Does incidental durotomy affect long-term outcomes of spinal stenosis?
Desai in 2011 looked at the SPORT data regarding the incidence of durotomy and its impact on outcomes for 419 patients with spinal stenosis with/without spondylolisthesis undergoing initial open laminectomies with/without fusion [
Comments: In Desai et al. study in 2011, the SPORT data analysis revealed that for 419 patients undergoing open initial decompressive laminectomies with/without fusions, 9% developed dural tears, but there were no root injuries in either the durotomy or nondurotomy groups.[
COMPLICATIONS OF OPEN LUMBAR SURGERY: DISKECTOMY
Spine Patient Outcomes Research Trial: Do outcomes vary across centers for surgery for lumbar disc herniation?
Desai et al. in 2012 noted that lumbar diskectomy is the most common spine operation; over 250,000 elective procedures are performed per year.[
Comments: This is an excellent study in which 792 patients from 13 academic centers in 11 states entered data regarding the frequency of risks and complications following initial open diskectomy.[
COMPLICATIONS OF OPEN LUMBAR SURGERY: FUSION
Impact of complications on patient outcomes following spinal fusion surgery
Verla et al. in 2015 noted that 2–16% of patients undergoing spinal surgery developed complications; they questioned their impact on long-term results [
Comments: This series of 1498 patients underwent primary lumbar fusions for back pain or radiculopathy[
LUMBAR NERVE ROOT INJURIES WITH MINIMALLY INVASIVE SURGERY
Minimally invasive surgery for disc degeneration and nerve root injuries
Clinical and radiological outcomes of anterior-posterior fusion (APF) versus transforaminal lumbar interbody fusion (TLIF) for disc degeneration
Faundez et al. in 2009 compared the operative results, including frequency of nerve root injuries, for 133 patients with lumbar disc degeneration undergoing one or two level anterior/posterior spine fusions (anterior-posterior fusion [APF]: 68 patients versus TLIF: 65 patients).[
Comments: This study addressed degenerative lumbar disease variously treated with APF versus TLIF. Notably, patients did not clearly exhibit focal preoperative neurological deficits or neurodiagnostic evidence of neural compromise to warrant these operations in the first place. Nevertheless, of the total 133 procedures performed, APF resulted in major life-threatening venous lacerations, while TLIF were responsible for many new root deficits.[
Preventing postoperative dysesthesia in minimally invasive transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar discs
Cho et al. in 2011 recorded perioperative complications attributed to MIS transforaminal percutaneous endoscopic lumbar discectomy (PELD) [
Comments: This study by Cho et al. in 2011 notes that of 154 patients undergoing MIS PELD utilizing a modified “floating method,” the frequency of POD (e.g., nerve root injuries) resulting from retraction of the DRG was reduced to 0%, although there was still 1 dural injury, 1 instance of discitis, and 3 cases (1.9%) of disc recurrence.[
Full-endoscopic interlaminar approach for lumbar discs, and when conversion to an open procedure becomes warranted
Wang et al. in 2012 utilized a full-endoscopic (FE) technique, including a unilateral portal interlaminar approach, for treating 50 patients with lumbar disc herniations (LDH) [
Comments: Wang et al. in 2012 observed a 10% conversion rate (5 of 50 patients) for patients initially undergoing FE unilateral portal interlaminar lumbar diskectomies.[
Posterior minimally invasive endoscopic discectomy: Results in 300 patients
Kaushal and Sen in 2012 evaluated the results of 300 posterior lumbar MIS endoscopic discectomies performed for managing disc disease [
Comments: Kaushal and Sen in 2012 performed 300 posterior lumbar MIS endoscopic diskectomies and concluded the procedure was both “safe and effective.”[
Exiting root injury in transforaminal endoscopic discectomy
Choi et al. in 2013 evaluated the clinical/radiological features signaling the risks of root injuries for proposed transforaminal endoscopic discectomy.[
Comments: This MR-based study nicely documents that MIS procedures should be individually tailored to each patient's anatomy. Here, directly measuring on the preoperative MR a shorter distance between the exiting root to the lower facet (6.4 ± 1.5 mm vs. 4.4 ± 0.8 mm) would enable the surgeon to choose other safer approaches (e.g., microdiscectomy or conventional open discectomy) to avoid root injuries that occurred in 20 (4.3%) of 233 MIS transforaminal endoscopic diskectomies.[
Meta-analysis of minimally invasive surgery versus open surgery for cervical and lumbar discectomy
In 2014, Evaniew et al. compared the safety/efficacy of MIS diskectomy versus open procedures addressing cervical or lumbar disc herniations (LDH) [
Comments: This study described the higher root injury and durotomy rates for different types of MIS versus open cervical and lumbar diskectomy procedures. Root injuries occurred in 1.39% of cervical and 2.25% of lumbar cases. Consistently, higher rates of neural injury were reported utilizing MIS techniques in both the cervical and lumbar regions.[
Full-endoscopic interlaminar L5/S1 discectomy
Li et al. in 2015 evaluated the efficacy of fully endoscopic (no conversions to open procedures) interlaminar L5/S1 diskectomy in 72 patients with axillary, ventral, or shoulder types/locations of disc herniations [
Comments: In this evaluation of 72 patients undergoing endoscopic diskectomy at the L5–S1 level, the authors noted no root injuries, no infections, and only one disc recurrence.[
MINIMALLY INVASIVE FUSION AND NERVE ROOT INJURIES; TRANSFORAMINAL LUMBAR INTERBODY FUSION (TLIF) ALONE (VS. OTHER MINIMALLY INVASIVE SURGICAL FUSIONS)
Transforaminal lumbar interbody fusion (TLIF) versus posterior lumbar interbody fusion (PLIF) morbidity including frequency of root injuries
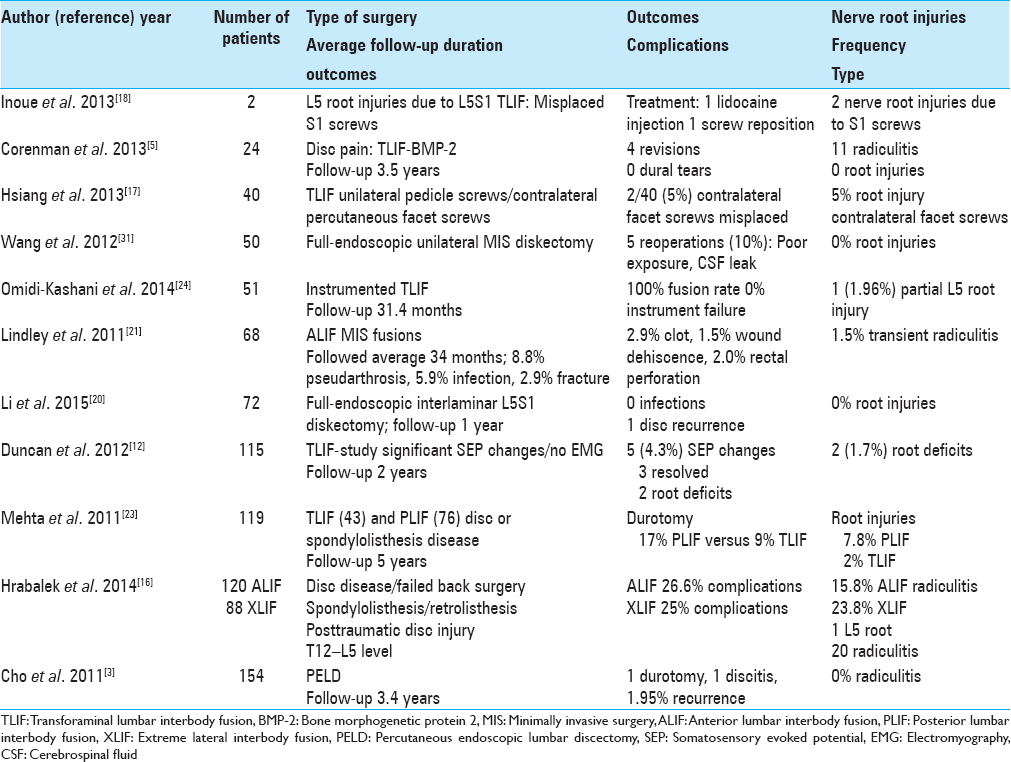
Over an average 5-year period, Mehta et al. in 2011 retrospectively compared the intraoperative and postoperative morbidity of 119 TLIF (43 patients) versus PLIF (76 patients) in patients undergoing spinal fusion for spondylolisthesis and degenerative disc disease [
Comments: The authors ultimately concluded that any interbody device, whether placed utilizing the TLIF or PLIF approaches, resulted in a higher incidence of not only nerve root injuries, but also durotomy.[
Minimally invasive one-level lumbar transforaminal lumbar interbody fusion (TLIF) utilizing both pedicle screw fixation and transpedicular facet screws
Hsiang et al. in 2013 presented a new minimally invasive (MI) technique for one-level TLIF utilizing ipsilateral pedicle screws alone with percutaneously placed contralateral tranpedicular fact screws [
Comments: This study presents a modification of the typical MI TLIF; they utilized ipsilateral pedicle screws, but contralateral percutaneously placed transpedicular facet screws to minimize soft tissue manipulation, and yet “preserve” biomechanical stabilization.[
Nerve root anomalies: Implications for transforaminal lumbar interbody fusion (TLIF)
Burke et al. in 2013 noted 2 cases in which conjoined/confluent nerve roots were either anticipated based on preoperative MR studies or simply encountered during mini-open TLIF surgery at the L4–L5 level [
Comments: Recognition either preoperatively or intraoperatively of conjoined/confluent nerve root anomalies is critical particularly with more restricted operative exposures provided in MI/MIS, or mini-open TLIF. Indeed, these minimal exposures potentially subject these nerve roots to inadvertent injury.[
L5 spinal nerve injury caused by misplacement of outwardly inserted S1 pedicle screws
Inoue et al. in 2013 evaluated 2 cases in which L5 nerve root injuries (e.g., severe pain resulting) were caused during L5S1 pedicle screw instrumented TLIF procedures [
Comments: This is an interesting analysis of what is often seen; anterior sacral perforation by S1 pedicle screws.[
Instrumented transforaminal lumbar interbody fusion (TLIF) for recurrent discs
Omidi-Kashani et al. in 2014 noted that after surgery for LDH the frequency of recurrent discs ranged from 5% to 15% [
Comments: There are several major questions raised here. First, why for LDH, is a TLIF required? Why not a focal decompression with diskectomy. Second, it is very difficult to believe the 100% TLIF fusion rate, particularly when many other series cite higher frequencies of pseudarthrosis. For example, Gologorsky et al. in 2014 cited a 17.5% pseudarthrosis rate for TLIF using unilateral pedicle instrumentation, and 2.5% for bilateral TLIF instrumented procedures.[
Increased pseudarthrosis rate after unilateral instrumented transforaminal lumbar interbody fusion (TLIF) for lumbar spondylosis
Gologorsky et al. in 2014 evaluated the utility of TLIF in 80 prospective patients utilizing bilateral (40 patients) or unilateral (40 patients) pedicle screw instrumentation over an average of 52 postoperative months.[
Comments: This article highlights the results of unilateral versus bilateral pedicle screw placement in TLIF constructs in a prospective patient population.[
MINIMALLY INVASIVE FUSION AND NERVE ROOT INJURIES; EXTREME LATERAL INTERBODY FUSION (XLIF)
Review: Safe zone for retractor placement to the lumbar spine via the transpsoas approach or extreme lateral interbody fusion (XLIF)
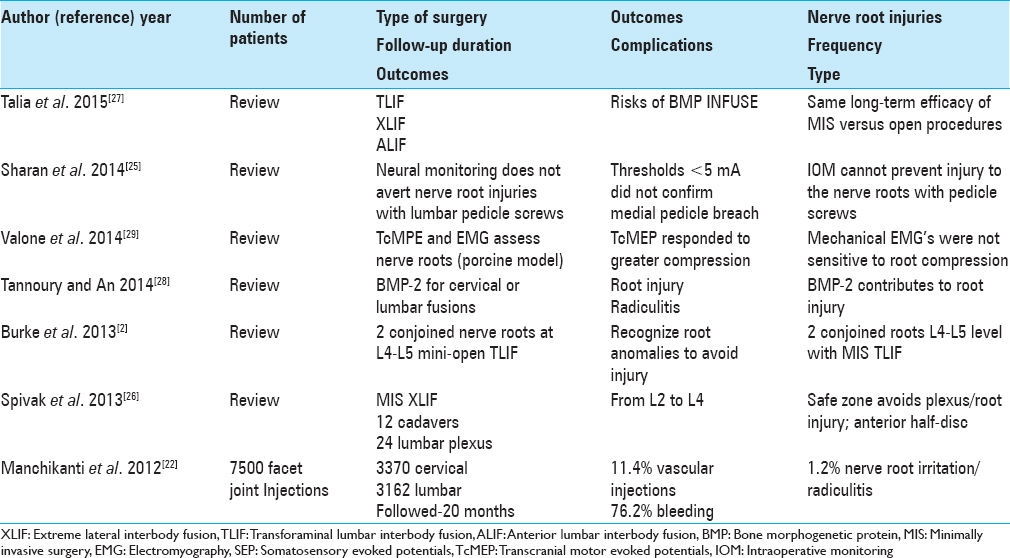
Spivak et al. in 2013 discussed the variable anatomy of the lumbar plexus with respect to the psoas muscle at the L23, L34, and L45 disc levels so that retractors for XLIF/transpsoas procedures could be safely placed [
Comments: As XLIF are typically performed for patients with pain alone without focal neurological or neuroradiological deficits, they should be considered unnecessary. Furthermore, this cadaveric study documents that the lumbar plexus and nerve roots from the L23 through the L45 levels are at great risk during these procedures.[
Review: Analysis of lumbar plexopathies and nerve injury after extreme lateral interbody fusion (XLIF) (lateral retroperitoneal transpsoas approach)
Ahmadian et al. in 2013 noted that the most typical complication of XLIF (lateral retroperitoneal transpsoas approach) included lumbar plexus/nerve root injuries [
Comments: In Ahmadian et al. study in 2013, they evaluated 18 studies involving 2310 patients, 304 (13.2%) of whom sustained root/plexus injuries.[
A comparison of complication rates for anterior versus lateral approaches to the lumbar spine; minimally invasive anterior lumbar interbody fusion (ALIF) versus minimally invasive extreme lateral interbody fusion (XLIF)
Hrabalek et al. in 2015 compared the complication rates of traditional MIS ALIF (120 patients) versus newer MIS XLIF (88 patients) procedures to approach disc herniations at the T12–L5 levels [
Comments: Again and again, we see studies in which the data clearly point out a vast number of major and/or minor complications attributed to minimally invasive operations, yet the authors/surgeons conclude the procedures are safe and effective. Nevertheless, the high frequency of nerve root/plexus-related complications noted in this XLIF study alone would seriously call into question whether these procedures should be performed at all.[
Comparison of lumbar interbody fusion techniques: Transforaminal lumbar interbody fusion (TLIF), anterior lumbar interbody fusion (ALIF), and extreme lateral interbody fusion (XLIF): A review
Talia et al. in 2015 reviewed the different surgical techniques offered for interbody lumbar fusion; anterior, lateral, transforaminal, and posterior approaches [
Comments: This review advisedly questions the safety/efficacy of TLIF, ALIF, and XLIF versus open procedures, while also raising the controversy regarding the use of BMP/INFUSE versus the gold standard; iliac crest autograft.[
COMPLICATIONS OF MINIMALLY INVASIVE ANTERIOR LUMBAR INTERBODY FUSIONS (ALIF) INCLUDING ROOT INJURIES
In 2011, Lindley et al. reviewed the complications of 68 MIS ALIF performed at the L1-L5, and L5-S1 levels over an average postoperative period of 34 months [
Comments: In this 2011 study, Lindley et al. found a 26.5% complication rate for 68 MIS ALIF performed at the L4–L5 and L5–S1 levels. Notably, there was a 1.5% incidence of transient nerve root irritation among a myriad of other significant complications.[
DUROTOMY AND LUMBAR NERVE ROOT INJURIES
Outcomes after incidental durotomy during 1st time open posterior lumbar diskectomy
Desai et al. in 2011 utilized the SPORT data to evaluate the frequency of durotomy and its accompanying complications following 799 1st time open diskectomy utilizing a “standard” open posterior lumbar diskectomy (use of the microscope was at the surgeon's discretion and was not recorded) [
Comments: The morbidity of open lumbar diskectomy as confirmed in this SPORT trial was extremely low. Out of 799 patients undergoing initial open surgery, the incidental durotomy rate was only 3.1%, and the frequency of neural injury was 1/774 (0.13%) without durotomy and 0/25 (0%) with durotomy.[
Surgery for lumbar degenerative spondylolisthesis in Spine Patient Outcomes Research Trial: Does incidental durotomy affect the outcome?
Desai et al. in 2012 retrospectively reviewed a multi-institutional (e.g., SPORT) database looking at the impact of durotomy on outcome in 389 patients undergoing initial decompressive lumbar laminectomy for degenerative spondylolisthesis with/without fusion [
Comments: In this SPORT trial by Desai et al. in 2012, for the 389 patients undergoing decompressive lumbar laminectomy for degenerative spondylolisthesis with/without fusion (not a MIS study), the overall incidence or durotomy was 10.5%.[
Incidental durotomy impact on long-term outcomes for spinal stenosis
Desai et al. in 2015, as part of another SPORT study evaluated patients with spinal stenosis without spondylolisthesis who underwent 1st time laminectomies with/without fusions [
Comments: The frequency of durotomy in this series appeared to be extraordinarily high at 9%; indeed there were 13 centers in 11 states involved in the study. Likely, many of these centers were major teaching hospitals, and the higher incidence of dural tears with less experienced surgeons likely reflected the number of residents involved.[
ELECTROPHYSIOLOGICAL MONITORING OF LUMBAR SURGERY AND NERVE ROOT INJURIES
Intraoperative decrease in amplitude of somatosensory evoked potentials of the lower extremities with interbody fusion cage placement during lumbar fusions
Duncan et al. in 2012 retrospectively analyzed over a 2 year period how often decreases in somatosensory evoked potential (SEP) amplitudes occurred without electromyographic (EMG) or MEP changes during 115 TLIF procedures [
Comments: This study underscores the need to better monitor not only TLIF but also any lumbar decompression with/without fusion with SEPs and EMGs (often MEP are not used as there is no cord involvement).[
Electrophysiological monitoring of lumbar fusion
Sharan et al. in 2014 observed that IOM is often utilized during lumbar fusion surgery to avert nerve root injuries attributed to pedicle screw placement [
Comments: This article states that IOM of pedicle screw placement during lumbar spinal instrumentation does not avoid nerve root injuries, and that low thresholds encountered following screw placement (e.g., M5 mA) did not clearly reflect medial pedicle breaches.[
Efficacy of transcranial motor evoked potentials and electromyography to assess nerve root function during compression in a porcine model
Valone et al. in 2014 observed that lumbar nerve root injury/weakness, variously attributed to operative manipulation/decompression, occurs in up to 30% of spinal deformity cases [
Comments: Valone et al. in 2014 observed that lumbar nerve root injury/weakness, variously attributed to operative manipulation/decompression, occurs in up to 30% of spinal deformity cases [
NERVE ROOT INJURIES DUE TO BONE MORPHOGENETIC PROTEIN IN LUMBAR FUSIONS
Bone morphogenetic protein-2 and spinal arthrodesis: Protein interaction with the nervous system
Dmitriev et al. in 2011 noted the high frequency of off-label use of BMP-2 (rhBMP-2) in spinal fusions. In theory, rhBMP-2, a potent growth factor, when placed near neural structures, can cause direct cord and root injury (e.g., DRG).[
Comments: There is a significant negative impact for applying rhBMP-2 near neural structures as documented by Dmitriev et al. in this 2011 article.[
Bone morphogenetic protein-2 (INFUSE) transforaminal lumbar interbody fusion for discogenic pain
Corenman et al. in their 2013 retrospective study, evaluated the outcomes, complications, and reoperation rates for TLIF performed in patients with discogenic pain syndrome (DPS) over a 2-year period utilizing BMP-2 [
Commentary: Corenman et al. 2013 retrospectively evaluated the results of TLIF with BMP-2 performed for patients with DPSs.[
Complications with the use of bone morphogenetic protein 2 in spine surgery (review)
Tannoury and An in 2014 reviewed literature regarding the morbidity/adverse events whey utilizing rhBMP-2 to perform cervical and lumbar spine fusions [
Comments: This review article by Tannoury and An in 2014 underscores the now commonly held belief that the use of rhBMP-2 resulted in adverse events including nerve root injury/radiculitis when utilized to perform cervical or lumbar fusions.[
ROOT INJURIES ATTRIBUTED TO FACET JOINT NERVE BLOCKS
Complications of fluoroscopically directed facet joint nerve blocks: A prospective evaluation of 7500 episodes with 43,000 nerve blocks
Manchikanti et al. in 2012 studied the adverse effects and complications of ambulatory fluoroscopically guided facet joint injection (FJI) performed over 20 months in the cervical spine (3370 patients), in the lumbar spine (3162 patients), and thoracic spine (950 patients) [
Comments: Considering there is no long-term documented efficacy for epidural steroid injections (ESIs) or facet joint injections (FJs), the frequency of minor complications appeared quite significant.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahmadian A, Deukmedjian AR, Abel N, Dakwar E, Uribe JS. Analysis of lumbar plexopathies and nerve injury after lateral retroperitoneal transpsoas approach: Diagnostic standardization. J Neurosurg Spine. 2013. 18: 289-97
2. Burke SM, Safain MG, Kryzanski J, Riesenburger RI. Nerve root anomalies: Implications for transforaminal lumbar interbody fusion surgery and a review of the Neidre and Macnab classification system. Neurosurg Focus. 2013. 35: E9-
3. Cho JY, Lee SH, Lee HY. Prevention of development of postoperative dysesthesia in transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar disc herniation: Floating retraction technique. Minim Invasive Neurosurg. 2011. 54: 214-8
4. Choi I, Ahn JO, So WS, Lee SJ, Choi IJ, Kim H. Exiting root injury in transforaminal endoscopic discectomy: Preoperative image considerations for safety. Eur Spine J. 2013. 22: 2481-7
5. Corenman DS, Gillard DM, Dornan GJ, Strauch EL. Recombinant human bone morphogenetic protein-2-augmented transforaminal lumbar interbody fusion for the treatment of chronic low back pain secondary to the homogeneous diagnosis of discogenic pain syndrome: Two-year outcomes. Spine (Phila Pa 1976). 2013. 38: E1269-77
6. Desai A, Ball PA, Bekelis K, Lurie J, Mirza SK, Tosteson TD. SPORT: Does incidental durotomy affect long-term outcomes in cases of spinal stenosis?. Neurosurgery. 2011. 69: 38-44
7. Desai A, Ball PA, Bekelis K, Lurie J, Mirza SK, Tosteson TD. SPORT: Does incidental durotomy affect longterm outcomes in cases of spinal stenosis?. Neurosurgery. 2015. 76: S57-63
8. Desai A, Ball PA, Bekelis K, Lurie J, Mirza SK, Tosteson TD. Surgery for lumbar degenerative spondylolisthesis in spine patient outcomes research trial: Does incidental durotomy affect outcome?. Spine (Phila Pa 1976). 2012. 37: 406-13
9. Desai A, Ball PA, Bekelis K, Lurie JD, Mirza SK, Tosteson TD. Outcomes after incidental durotomy during first-time lumbar discectomy. J Neurosurg Spine. 2011. 14: 647-53
10. Desai A, Bekelis K, Ball PA, Lurie J, Mirza SK, Tosteson TD. Spine patient outcomes research trial: Do outcomes vary across centers for surgery for lumbar disc herniation?. Neurosurgery. 2012. 71: 833-42
11. Dmitriev AE, Lehman JT, Symes AJ. Bone morphogenetic protein-2 and spinal arthrodesis: The basic science perspective on protein interaction with the nervous system. Spine J. 2011. 11: 500-5
12. Duncan JW, Bailey RA, Baena R. Intraoperative decrease in amplitude of somatosensory-evoked potentials of the lower extremities with interbody fusion cage placement during lumbar fusion surgery. Spine (Phila Pa 1976). 2012. 37: E1290-5
13. Evaniew N, Khan M, Drew B, Kwok D, Bhandari M, Ghert M. Minimally invasive versus open surgery for cervical and lumbar discectomy: A systematic review and meta-analysis. CMAJ Open. 2014. 2: E295-305
14. Faundez AA, Schwender JD, Safriel Y, Gilbert TJ, Mehbod AA, Denis F. Clinical and radiological outcome of anterior-posterior fusion versus transforaminal lumbar interbody fusion for symptomatic disc degeneration: A retrospective comparative study of 133 patients. Eur Spine J. 2009. 18: 203-11
15. Gologorsky Y, Skovrlj B, Steinberger J, Moore M, Arginteanu M, Moore F. Increased incidence of pseudarthrosis after unilateral instrumented transforaminal lumbar interbody fusion in patients with lumbar spondylosis: Clinical article. J Neurosurg Spine. 2014. 21: 601-7
16. Hrabalek L, Adamus M, Gryga A, Wanek T, Tucek P. A comparison of complication rate between anterior and lateral approaches to the lumbar spine. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014. 158: 127-32
17. Hsiang J, Yu K, He Y. Minimally invasive one-level lumbar decompression and fusion surgery with posterior instrumentation using a combination of pedicle screw fixation and transpedicular facet screw construct. Surg Neurol Int. 2013. 4: 125-
18. Inoue M, Inoue G, Ozawa T, Miyagi M, Kamoda H, Ishikawa T. L5 spinal nerve injury caused by misplacement of outwardly-inserted S1 pedicle screws. Eur Spine J. 2013. 22: S461-5
19. Kaushal M, Sen R. Posterior endoscopic discectomy: Results in 300 patients. Indian J Orthop. 2012. 46: 81-5
20. Li ZZ, Hou SX, Shang WL, Song KR, Zhao HL. The strategy and early clinical outcome of full-endoscopic L5/S1 discectomy through interlaminar approach. Clin Neurol Neurosurg. 2015. 133: 40-5
21. Lindley EM, McCullough MA, Burger EL, Brown CW, Patel VV. Complications of axial lumbar interbody fusion. J Neurosurg Spine. 2011. 15: 273-9
22. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. Complications of fluoroscopically directed facet joint nerve blocks: A prospective evaluation of 7,500 episodes with 43,000 nerve blocks. Pain Physician. 2012. 15: E143-50
23. Mehta VA, McGirt MJ, Garcés Ambrossi GL, Parker SL, Sciubba DM, Bydon A. Trans-foraminal versus posterior lumbar interbody fusion: Comparison of surgical morbidity. Neurol Res. 2011. 33: 38-42
24. Omidi-Kashani F, Ghayem Hasankhani E, Noroozi HR. Instrumented transforaminal lumbar interbody fusion in surgical treatment of recurrent disc herniation. Med J Islam Repub Iran. 2014. 28: 124-
25. Sharan A, Groff MW, Dailey AT, Ghogawala Z, Resnick DK, Watters WC. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 15: Electrophysiological monitoring and lumbar fusion. J Neurosurg Spine. 2014. 21: 102-5
26. Spivak JM, Paulino CB, Patel A, Shanti N, Pathare N. Safe zone for retractor placement to the lumbar spine via the transpsoas approach. J Orthop Surg (Hong Kong). 2013. 21: 77-81
27. Talia AJ, Wong ML, Lau HC, Kaye AH. Comparison of the different surgical approaches for lumbar interbody fusion. J Clin Neurosci. 2015. 22: 243-51
28. Tannoury CA, An HS. Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J. 2014. 14: 552-9
29. Valone F, Lyon R, Lieberman J, Burch S. Efficacy of transcranial motor evoked potentials, mechanically elicited electromyography, and evoked electromyography to assess nerve root function during sustained compression in a porcine model. Spine (Phila Pa 1976). 2014. 39: E989-93
30. Verla T, Adogwa O, Fatemi P, Martin JR, Gottfried ON, Cheng J. Clinical implication of complications on patient perceived health status following spinal fusion surgery. J Clin Neurosci. 2015. 22: 342-5
31. Wang B, Lü G, Liu W, Cheng I, Patel AA. Full-endoscopic interlaminar approach for the surgical treatment of lumbar disc herniation: The causes and prophylaxis of conversion to open. Arch Orthop Trauma Surg. 2012. 132: 1531-8