- Department of Neuroscience, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
Correspondence Address:
Nancy E. Epstein
Department of Neuroscience, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
DOI:10.4103/sni.sni_49_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. More risks and complications for elective spine surgery in morbidly obese patients. 26-Apr-2017;8:66
How to cite this URL: Nancy E. Epstein. More risks and complications for elective spine surgery in morbidly obese patients. 26-Apr-2017;8:66. Available from: http://surgicalneurologyint.com/surgicalint-articles/more-risks-and-complications-for-elective-spine-surgery-in-morbidly-obese-patients/
Abstract
Background:The vast majority of studies emphasize the greater morbidity/mortality for elective spine surgery in morbidly obese patients.
Methods:This review focuses on the increased morbidity/mortality of performing elective spinal operations in morbidly obese patients. There are two definitions of morbid obesity; a body mass index (BMI) of equal to or greater than 35 plus two major comorbid factors (e.g., hypertension, diabetes, etc.) or a BMI (morbidly obese III) of =≥40 kg/m2.
Results:For patients undergoing spinal surgery, morbid obesity increases perioperative morbidity/mortality for various reasons. The quality of preoperative and intraoperative imaging is often compromised potentially leading to mistaken preoperative diagnoses, and wrong level surgery. Resultant major technical surgical limitations include poor/inadequate operative exposure, and the risk of suboptimal placement of instrumentation There is also increased exposure to major perioperative complications such as deep venous thrombosis, pulmonary embolism, infection, pneumonia, cardiac complications, blindness in the prone position, brachial and lumbar plexus injuries, increased anesthetic risks (e.g., even using awake intubation/awake positioning), and postoperative wound seromas/hematomas.
Conclusions:Most of the spinal literature documents the marked increased perioperative morbidity/mortality for morbidly obese patients undergoing elective spine surgery. If elective surgery is warranted in these patients, the risks and timing of surgical intervention should include consideration of major preoperative weight loss strategies including bariatric procedures to optimize outcomes.
Keywords: Elective spine surgery, morbid obesity, morbidity, mortality, rates
INTRODUCTION
This review focuses on the increased morbidity/mortality for performing elective spine surgery in morbidly obese patients, but does not address emergency surgery. Here, we define morbid obesity as a BMI of >35 with two major comorbidities, or a BMI of >/=40 kg/m2 or greater. Our evaluation included the assessment of multiple perioperative factors and the attendant adverse events (AE)/complications that accompanied morbid obesity. Increased perioperative risks correlated with more prolonged anesthetic and operative times, greater estimated blood loss (EBL), poorer quality of preoperative, intraoperative (more difficulty correctly localizing the surgical levels), and postoperative diagnostic studies, more medical complications, and poorer surgical outcomes.
REVIEW DOES NOT INCLUDE ANALYSIS OF TRAUMATIC INJURIES IN MORBIDLY OBESE PATIENTS
This review did not focus on the greater morbidity/mortality associated with treating morbidly obese patients following traumatic spine injuries.[
LIMITATIONS OF LARGE DATABASE ANALYSIS FOR MORBIDLY OBESE PATIENTS UNDERGOING SPINE SURGERY
Large database analyses for morbidly obese patients undergoing spine surgery often have major shortcomings. When Golinvaux et al. (2014) used the International Classification of Diseases Ninth Revision (ICD-9) codes to study morbidly obese patients undergoing spine surgery, 174 of 2075 patients were “morbidly obese” (BMI >40), but only 84 were correctly coded (278.01) [
MORE MEDICAL RISK FACTORS WITH MORBID OBESITY
As spinal surgeons, we need to carefully assess whether our patients are “adequate medical” candidates for surgery [
Higher risks of deep venous thrombosis/pulmonary embolism in morbidly obese patients undergoing spine surgery
Morbid obesity increases the risks of perioperative/postoperative phlebitis, and pulmonary embolism [
Role for prophylactic inferior vena cava filters for spine surgery in morbidly obese patients
The spinal surgical literature supports the prophylactic placement of inferior vena cava (IVC) filters for morbid obesity (BMI >40), a history of DVT/PE, cancer, fusions, hypercoagulation syndromes, pulmonary/circulatory disorders, preoperative/postoperative immobility, staged procedures (five spinal levels), combined anterior-posterior surgery, iliocaval manipulation, age >80 years, and prolonged surgery (e.g., >261 min vs. >8 h). In 2015, two morbidly obese patients, ages 68 and 69 years of age, prophylactically had IVC filters placed by the author prior to multilevel L1-S1 lumbar laminectomies (note negative preoperative “surveillance” Doppler’s).[
ANESTHETIC RISKS WITH MORBID OBESITY
Administering anesthesia is more complex in morbidly obese patients undergoing spine surgery. These patients may undergo awake nasotracheal/endotracheal fiberoptic intubation and awake positioning. Additionally using the 3-pin head holder maintains the neck in a neutral posture and avoids kinking the nasotracheal/endotracheal tube, avoids direct pressure on the face, limits neck rotation avoiding carotid and/or jugular compression, and avoids pressure on the eyes limiting the risk of blindness in the prone position (e.g., ischemic optic neuropathy (ION) (anterior (AION)/posterior (PION) by avoiding direct eye compression and increased venous/arterial pressure). Increased intraoperative risks for morbidly obese patients undergoing spinal procedures also include greater blood loss (attributed to increased intrathoracic pressure and greater back-bleeding from Batson's venous plexus), positioning-related brachial or lumbar plexus injury [e.g., even with intraoperative electromyography (EMG) monitoring], and sores/skin sloughing particularly for longer cases. In an analysis of 1861 patients undergoing elective posterior lumbar fusions, obtained from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP), factors correlating with greater complications/AE with spine surgery included longer length of stay (LOS), older age, morbid obesity (body mass index ≥40 kg/m), higher American Society of Anesthesiologists (ASA) classification, longer and multilevel operations, and greater transfusion requirements [
NO INCREASED MORBIDITY FOR CERVICAL SPINE SURGERY IN MORBIDLY OBESE PATIENTS
Two studies documented no significant increase in morbidity/mortality for morbidly obese patients undergoing cervical spine surgery [
INCREASED MORBIDITY FOR LUMBAR SURGERY IN MORBIDLY OBESE PATIENTS
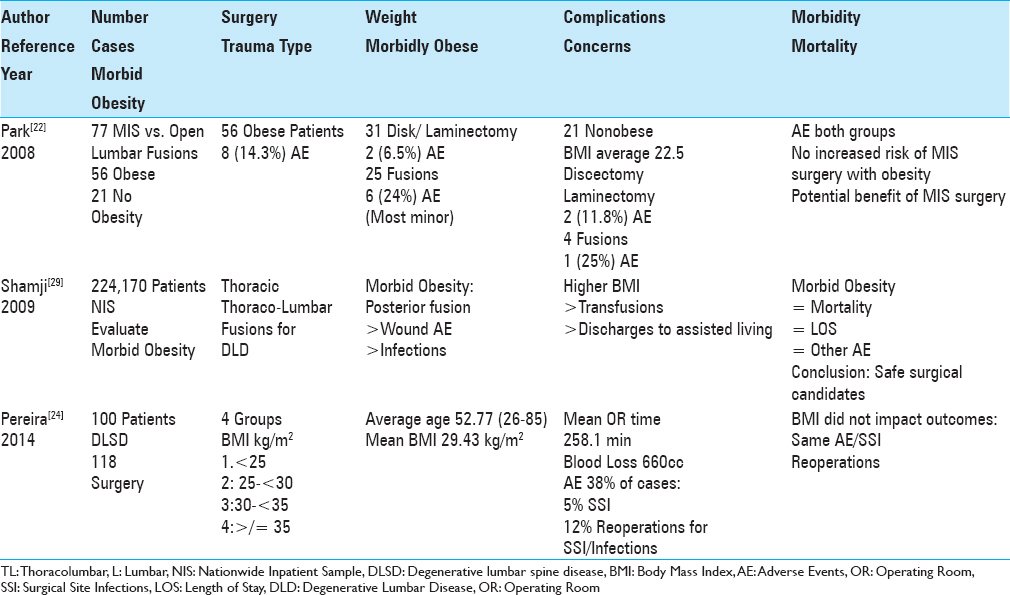
Three research studies specifically documented marked increases in perioperative morbidity for elective spine operations performed in morbidly obese patients [
A third study (2014) retrospectively examined the outcomes of lumbar fusions [anterior, posterior, transforaminal lumbar interbody fusions (TLIF)], for nonobese vs. obese (2 groups) vs. morbidly obese patients using the ACS-NSQIP database (2005 to 2010) [
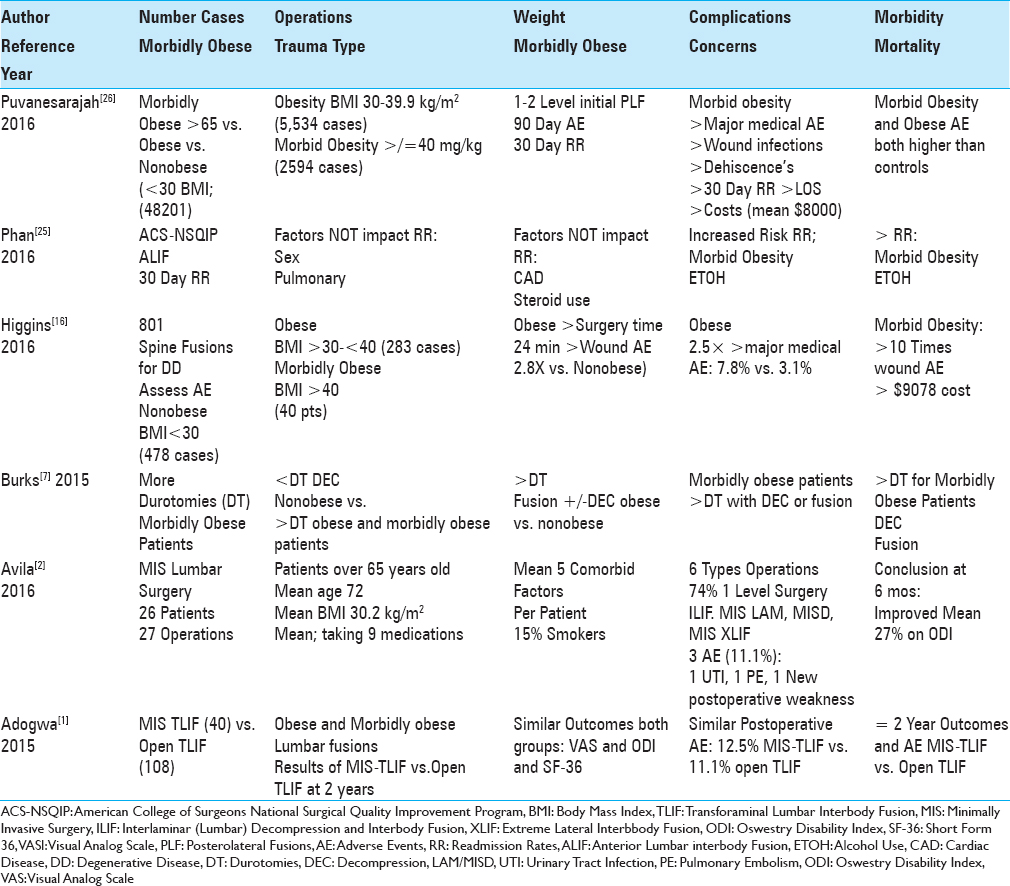
Lumbar fusions in morbidly obese patients increase complication/AE, readmission/reoperation rates, and resource utilization
Morbidly obese patients undergoing lumbar fusions experienced increased complications/AE, readmission, reoperation, and resource utilization rates [
Instrumented thoracolumbar/lumbar fusions in morbidly obese patients associated with more complications/AE
Several studies documented increased complication rates for morbidly obese patients undergoing thoracic/thoracolumbar/lumbar instrumented fusions [
Morbid obesity increases infection rate for lumbar surgery
Olsen et al. (2003) determined that morbid obesity was a major risk factor contributing to surgical site infections (SSIs) following laminectomy and/or spinal fusion procedures [
More durotomies in morbidly obese patients undergoing lumbar surgery
Burks et al. (2015) observed that durotomies (dural tears (DT)) typically occurred in from 0.5% to 2.6% (large database population) of patients undergoing spinal procedures, but were more frequent in obese or morbidly obese patients having decompression and/or fusions [
MORBID OBESITY DOES NOT INCREASE MORBIDITY FOR OPEN VS. MIS SPINE SURGERY
Morbid obesity had no negative impact on complications/AE or outcomes of MIS vs. open lumbar spine surgery [
Avila et al. (2016) retrospectively evaluated the outcomes/complications for one surgeon performing 27 MIS lumbar procedures in 26 patients over the age of 65 with multiple comorbidities, and an average BMI of 30.2 kg/m2 [
ANTERIOR LUMBAR INTERBODY FUSIONS IN MORBIDLY OBESE PATIENTS INCREASES COMPLICATION/AE RATES
Phan et al. (2016), utilizing National Surgical Quality Improvement Program (ACS NSQIP), evaluated the 30-day readmissions after anterior lumbar interbody fusions (ALIF) [
PROS AND CONS OF BARIATRIC SURGERY IN MORBIDLY OBESE PATIENTS
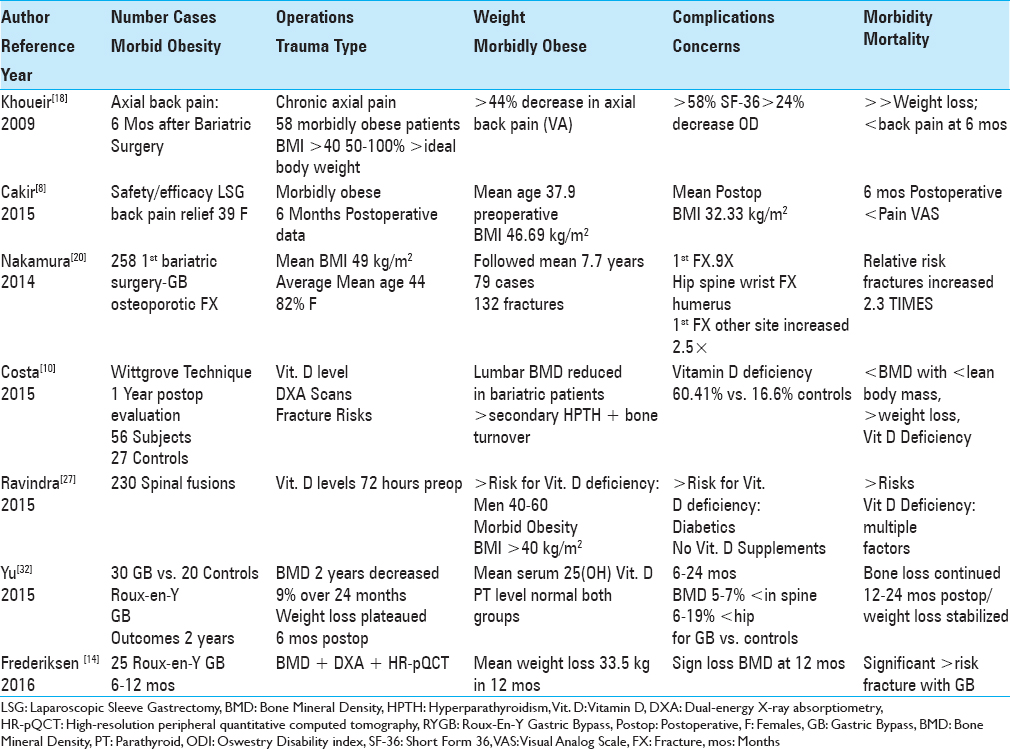
Bariatric surgery and weight loss reduces back pain in morbidly obese patients
Several authors documented substantial weight reduction, reduced chronic back pain, and a reduced need for spine surgery 6 months following bariatric procedures in morbidly obese patients.[
Bariatric surgery in morbidly obese patients results in osteoporosis, reduced bone mineral density (BMD), vitamin D deficiency, and increases fracture risk
Three studies demonstrated that bariatric surgery results in a greater risk of osteoporosis, reduced bone mineral density (BMD), Vitamin D deficiency, and an increased risk of spinal fractures [
Two-year changes in BMD after Roux-en-Y gastric bypass surgery
Two studies showed decreases in BMD following Roux-en-Y gastric bypasses.[
CONCLUSION
The majority of studies involving morbidly obese patients undergoing lumbar spinal surgery demonstrated increased perioperative morbidity. The greater complication/AE Rates included more prolonged operative times, longer anesthesia time, greater intraoperative blood loss, more postoperative wound complications, higher infection rate, longer LOS, poorer outcomes, more durotomies, and more medical complications (e.g., DVT/PE, UTI, respiratory complications) among others. Interestingly, morbid obesity did not negatively impact the outcomes of cervical spine surgery, particularly if performed anteriorly. Although bariatric procedures prior to spine surgery typically results in marked weight loss and potential reduction of perioperative morbidity, the procedures themselves increase the perioperative risks attributed to more severe osteoporosis, reduced BMD, greater Vitamin D Deficiency, and greater susceptibility to fracture.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adogwa O, Carr K, Thompson P, Hoang K, Darlington T, Perez E. A prospective, multi-institutional comparative effectiveness study of lumbar spine surgery in morbidly obese patients: Does minimally invasive transforaminal lumbar interbody fusion result in superior outcomes?. World Neurosurg. 2015. 83: 860-6
2. Avila MJ, Walter CM, Baaj AA. Outcomes and Complications of Minimally Invasive Surgery of the Lumbar Spine in the Elderly. Cureus. 2016. 8: e519-
3. Basques BA, Fu MC, Buerba RA, Bohl DD, Golinvaux NS, Grauer JN. Using the ACS-NSQIP to identify factors affecting hospital length of stay after elective posterior lumbar fusion. Spine. 2014. 39: 497-502
4. Baxi V, Budhakar S. Anesthesia management of a morbidly obese patient in prone position for lumbar spine surgery. Craniovertebr Junction Spine. 2010. 1: 55-7
5. Buerba RA, Fu MC, Grauer JN. Anterior and posterior cervical fusion in patients with high body mass index are not associated with greater complications. Spine J. 2014. 14: 1643-53
6. Buerba RA, Fu MC, Gruskay JA, Long WD, Grauer JN. Obese Class III patients at significantly greater risk of multiple complications after lumbar surgery: An analysis of 10,387 patients in the ACS NSQIP database. Spine J. 2014. 14: 2008-18
7. Burks CA, Werner BC, Yang S, Shimer AL. Obesity is associated with an increased rate of incidental durotomy in lumbar spine surgery. Spine. 2015. 40: 500-4
8. Çakır T, Oruç MT, Aslaner A, Duygun F, Yardımcı EC, Mayir B. The effects of laparoscopic sleeve gastrectomy on head, neck, shoulder, low back and knee pain of female patients. Int J Clin Exp Med. 2015. 8: 2668-73
9. Chotai S, Sielatycki JA, Parker SL, Sivaganesan A, Kay HL, Stonko DP1. Effect of obesity on cost per quality-adjusted life years gained following anterior cervical discectomy and fusion in elective degenerative pathology. Spine J. 2016. 9430: 30281-9
10. Costa TL, Paganotto M, Radominski RB, Kulak CM, Borba V. Calcium metabolism, vitamin D and bone mineral density after bariatric surgery. Osteoporos Int. 2015. 26: 757-64
11. Douglass J, Fraser J, Andrzejowski J. Awake intubation and awake prone positioning of a morbidly obese patient for lumbar spine surgery. Anaesthesia. 2014. 69: 166-9
12. Epstein NE. How much medicine do spine surgeons need to know to better select and care for patients?. Surg Neurol Int. 2012. 3: S329-49
13. Epstein NE. Prophylactic inferior vena cava filter placement prior to lumbar surgery in morbidly obese patients: Two-case study and literature review. Surg Neurol Int. 2015. 6: S469-74
14. Frederiksen KD, Hanson S, Hansen S, Brixen K, Gram J, Jørgensen NR. Bone Structural Changes and Estimated Strength After Gastric Bypass Surgery Evaluated by HR-pQCT. Calcif Tissue Int. 2016. 98: 253-62
15. Golinvaux NS, Bohl DD, Basques BA, Fu MC, Gardner EC, Grauer JN. Limitations of administrative databases in spine research: A study in obesity. Spine J. 2014. 14: 2923-8
16. Higgins DM, Mallory GW, Planchard RF, Puffer RC, Ali M, Gates MJ. Understanding the Impact of Obesity on Short-term Outcomes and In-hospital Costs After Instrumented Spinal Fusion. Neurosurgery. 2016. 78: 127-32
17. Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine. 2012. 37: 982-8
18. Khoueir P, Black MH, Crookes PF, Kaufman HS, Katkhouda N, Wang MY. Prospective assessment of axial back pain symptoms before and after bariatric weight reduction surgery. Spine J. 2009. 9: 454-63
19. Marquez-Lara A, Nandyala SV, Sankaranarayanan S, Noureldin M, Singh K. Body mass index as a predictor of complications and mortality after lumbar spine surgery. Spine. 2014. 39: 798-804
20. Nakamura KM, Haglind EG, Clowes JA, Achenbach SJ, Atkinson EJ, Melton LJ. Fracture risk following bariatric surgery: A population-based study. Osteoporos Int. 2014. 25: 151-8
21. Olsen MA, Mayfield J, Lauryssen C, Polish LB, Jones M, Vest J. Risk factors for surgical site infection in spinal surgery. J Neurosurg. 2003. 98: 149-55
22. Park P, Upadhyaya C, Garton HJ, Foley KT. The impact of minimally invasive spine surgery on perioperative complications in overweight or obese patients. Neurosurgery. 2008. 62: 693-9
23. Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR. Obesity and spine surgery: Relation to perioperative complications. J Neurosurg Spine. 2007. 6: 291-7
24. Pereira BJ, de Holanda CV, Ribeiro CA, de Moura SM, Galvão PE, Quidute BS. Impact of body mass index in spinal surgery for degenerative lumbar spine disease. Clin Neurol Neurosurg. 2014. 127: 112-5
25. Phan K, Lee NJ, Kothari P, Kim JS, Cho SK. Risk Factors for Readmissions Following Anterior Lumbar Interbody Fusion. Spine. 2016. p.
26. Puvanesarajah V, Cancienne JM, Pehlivan H, Jain A, Shimer AL, Singla A. Morbid Obesity and Lumbar Fusion in Patients over 65 Years of Age: Complications, Readmissions, Costs, and Length of Stay. Spine. 2017. 42: 122-7
27. Ravindra VM, Godzik J, Guan J, Dailey AT, Schmidt MH, Bisson EF. Prevalence of Vitamin D Deficiency in Patients Undergoing Elective Spine Surgery: A Cross-Sectional Analysis. World Neurosurg. 2015. 83: 1114-9
28. Rosenfeld HE, Limb R, Chan P, Fitzgerald M, Bradley WP, Rosenfeld JV. Challenges in the surgical management of spine trauma in the morbidly obese patient: A case series. Neurosurg Spine. 2013. 19: 101-9
29. Shamji MF, Parker S, Cook C, Pietrobon R, Brown C, Isaacs RE. Impact of body habitus on perioperative morbidity associated with fusion of the thoracolumbar and lumbar spine. Neurosurgery. 2009. 65: 490-8
30. Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine. 2009. 34: 495-500
31. Yagi M, Patel R, Boachie-Adjei O. Complications and Unfavorable Clinical Outcomes in Obese and Overweight Patients Treated for Adult Lumbar or Thoracolumbar Scoliosis With Combined Anterior/Posterior Surgery. J Spinal Disord Tech. 2015. 28: E368-76
32. Yu EW, Bouxsein ML, Putman MS, Monis EL, Roy AE, Pratt JS. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015. 100: 1452-9