- Department of Neurosurgery, Gunma University, Maebashi, Japan.
- Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Fujieda, Japan.
Correspondence Address:
Hiroya Shimauchi-Ohtaki, Department of Neurosurgery, Gunma University, Maebashi, Japan.
DOI:10.25259/SNI_669_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hiroya Shimauchi-Ohtaki1, Toshiyuki Takahashi2, Manabu Minami2, Ryo Kanematsu2, Fumiaki Honda1, Junya Hanakita2. Morphological changes in nerve rootlets in patients with cervical radiculopathy assessed using computed tomography myelogram. 26-Aug-2022;13:391
How to cite this URL: Hiroya Shimauchi-Ohtaki1, Toshiyuki Takahashi2, Manabu Minami2, Ryo Kanematsu2, Fumiaki Honda1, Junya Hanakita2. Morphological changes in nerve rootlets in patients with cervical radiculopathy assessed using computed tomography myelogram. 26-Aug-2022;13:391. Available from: https://surgicalneurologyint.com/surgicalint-articles/11821/
Abstract
Background: There are only a few reports that utilize computed tomography myelogram (CTM) to define cervical nerve rootlet compromise in patients with radiculopathy. Here, we assessed the characteristic morphological changes in nerve rootlets in 32 cases with cervical radiculopathy by analyzing CTMs warranting anterior foraminotomy.
Methods: CTMs were analyzed to elucidate morphological changes in nerve rootlets in 31 patients/32 cases with cervical radiculopathy. Notably, three of the four neurosurgeons evaluating these CTM had to agree on the presence of “significant” changes consisting of contrast-enhanced defects near the entrance of the intervertebral foramen on axial sections.
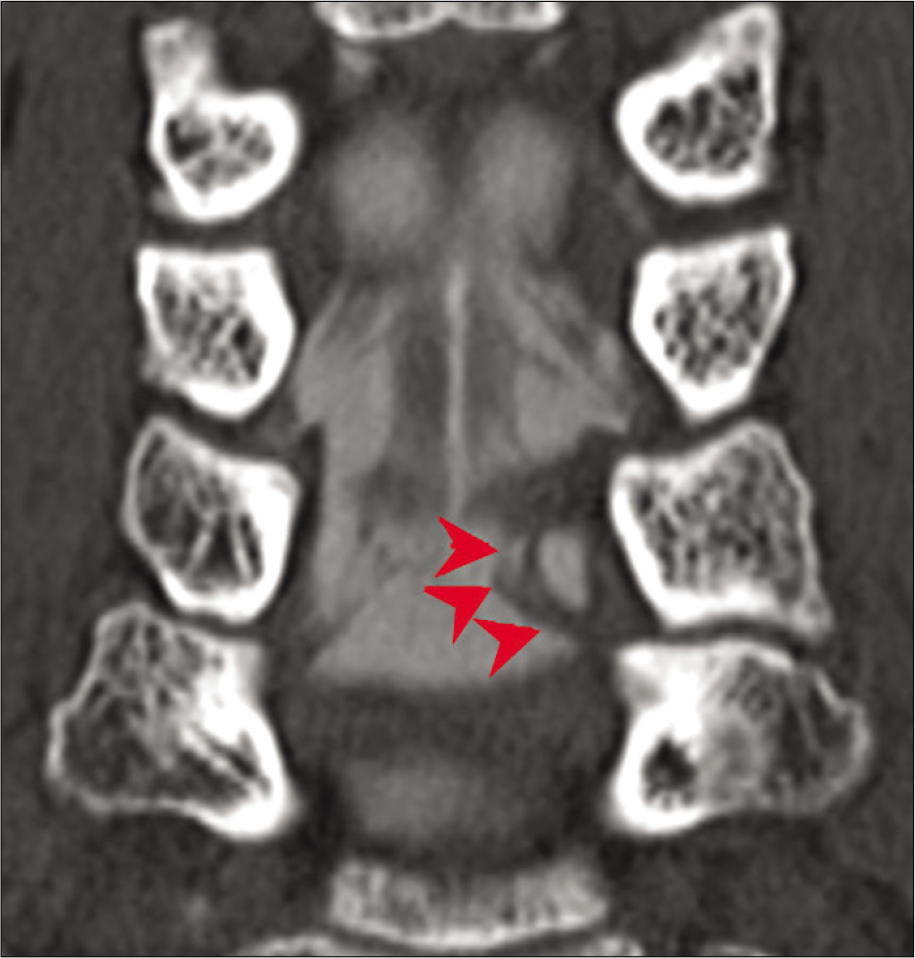
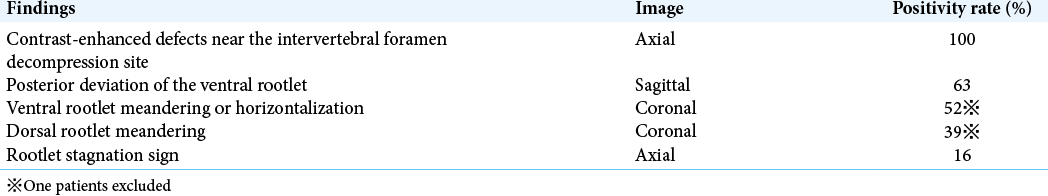
Results: Our findings included; posterior deviation of the ventral rootlet on the sagittal section (63%), ventral rootlet meandering or horizontalization (52%), and dorsal rootlet meandering (39%) on the coronal section. Furthermore, 16% of cervical nerve rootlets may exhibit an abnormal course proximal to the compression site (i.e., the definition of the “rootlet stagnation sign”).
Conclusion: CTM better defines the anatomy, pathology, and radiology impacting the anterior or posterior cervical roots in patients presenting with cervical radiculopathy.
Keywords: Anterior foraminotomy, Cervical nerve root, Cervical radiculopathy, Computed tomography myelogram
INTRODUCTION
Here, we studied how computed tomography myelogram (CTM) better defined the pathology of cervical nerve rootlets for 31 patients/32 cases presenting with cervical radiculopathy about to undergo anterior cervical foraminotomies.[
MATERIALS AND METHODS
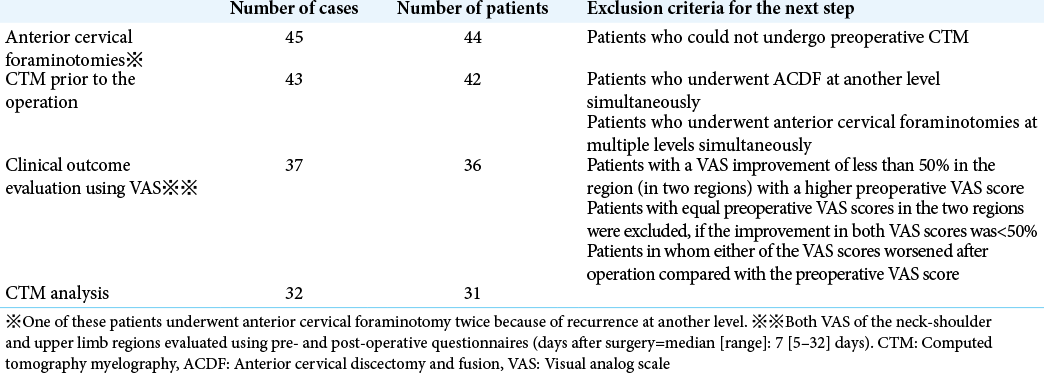
We assessed 32 cases of cervical radiculopathy in 31 patients, with an average age of 57.4 years (36–81 years), undergoing anterior cervical foraminotomies at the C4/5 (one case: 3%), C5/6 (three cases: 9%), C6/7 (22 cases: 69%), and C7/T1 (six cases: 19%) levels. In addition, clinical outcomes were assessed utilizing the visual analog scale (VAS) [
Evaluation of CTMs
CTMs were performed and then reviewed by four neurosurgeons who independently evaluated all 31 patients/32 cases who underwent anterior cervical foraminotomy for cervical radiculopathy. Studies were considered “positive” when three of four neurosurgeons agreed on the findings.
RESULTS
Outcomes
Postoperatively, the VAS improved in all patients; median values for the preoperative neck-shoulder and upper limb VAS were 7 (1–10) cm and 7 (0–10) cm, respectively. Median values of the postoperative neck-shoulder and upper limb VAS were 1 (0–8) cm and 0.5 (0–3) cm, respectively.
Evaluation of CTM
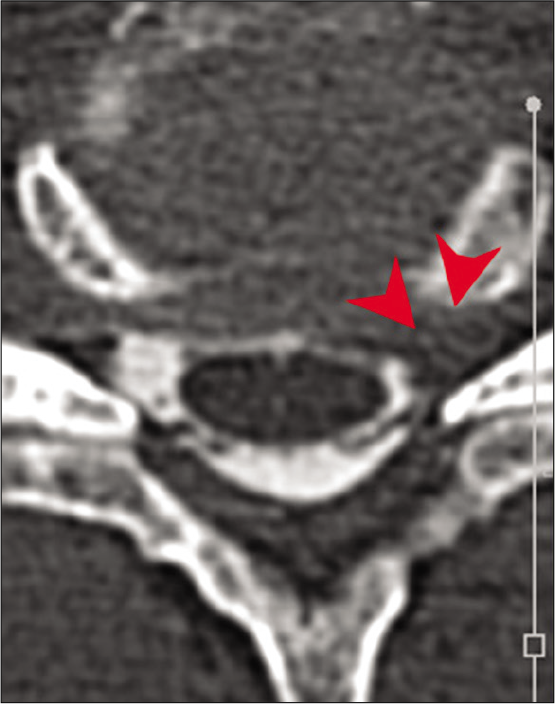
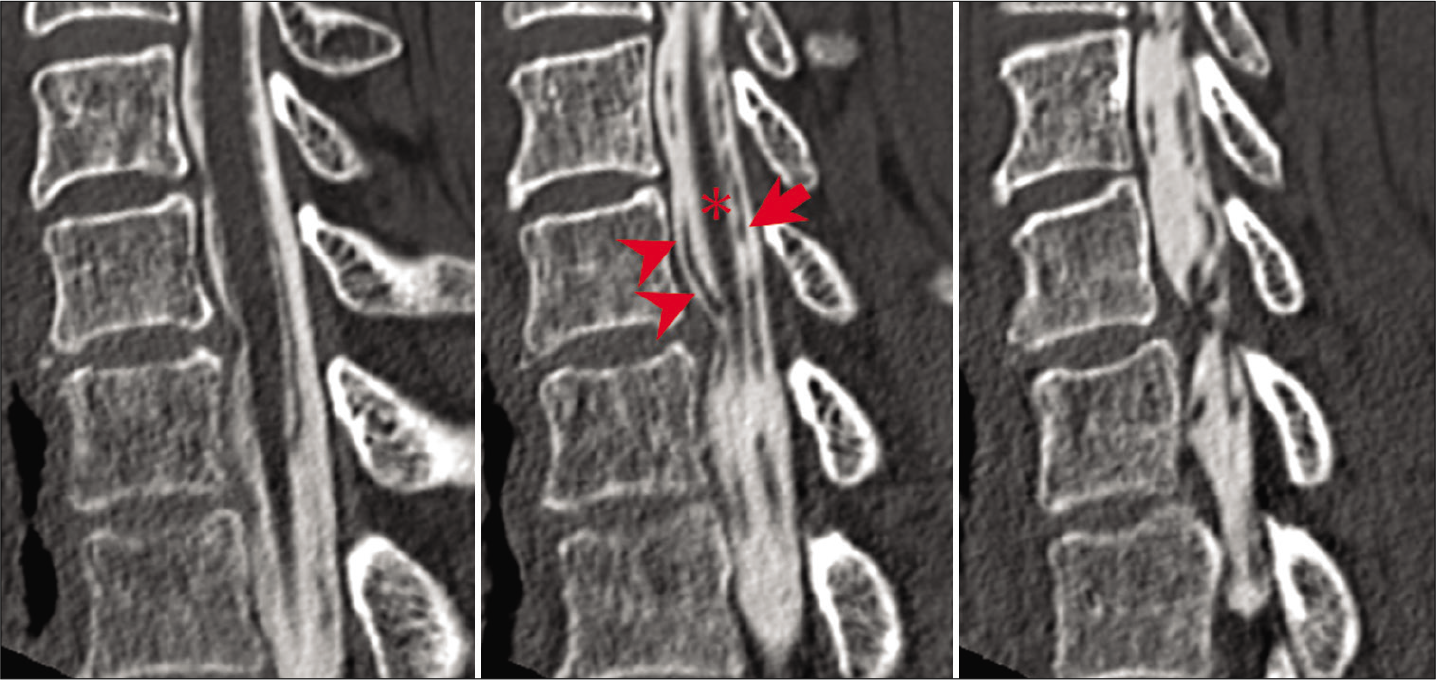
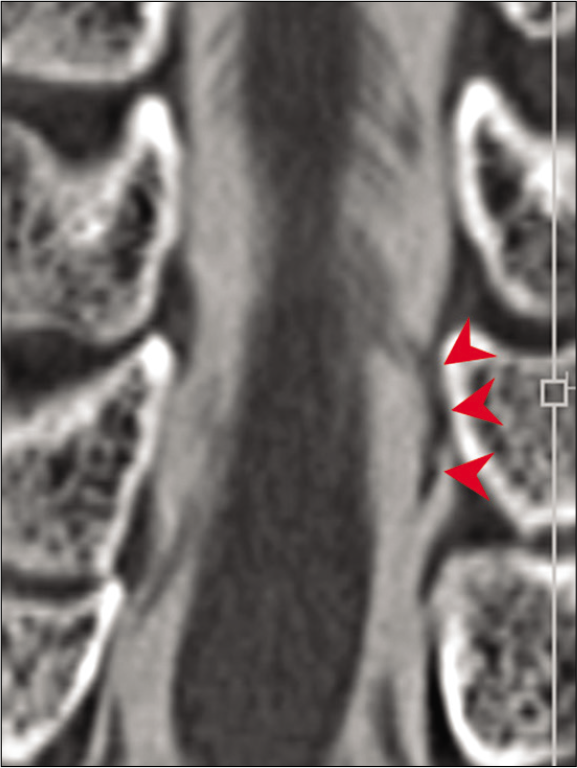
Contrast-enhanced defects near the entrance of the intervertebral foramen were seen in all 32 cases on axial CTMs, while posterior deviation of the ventral rootlets was seen in 63% of patients on serial sagittal studies [
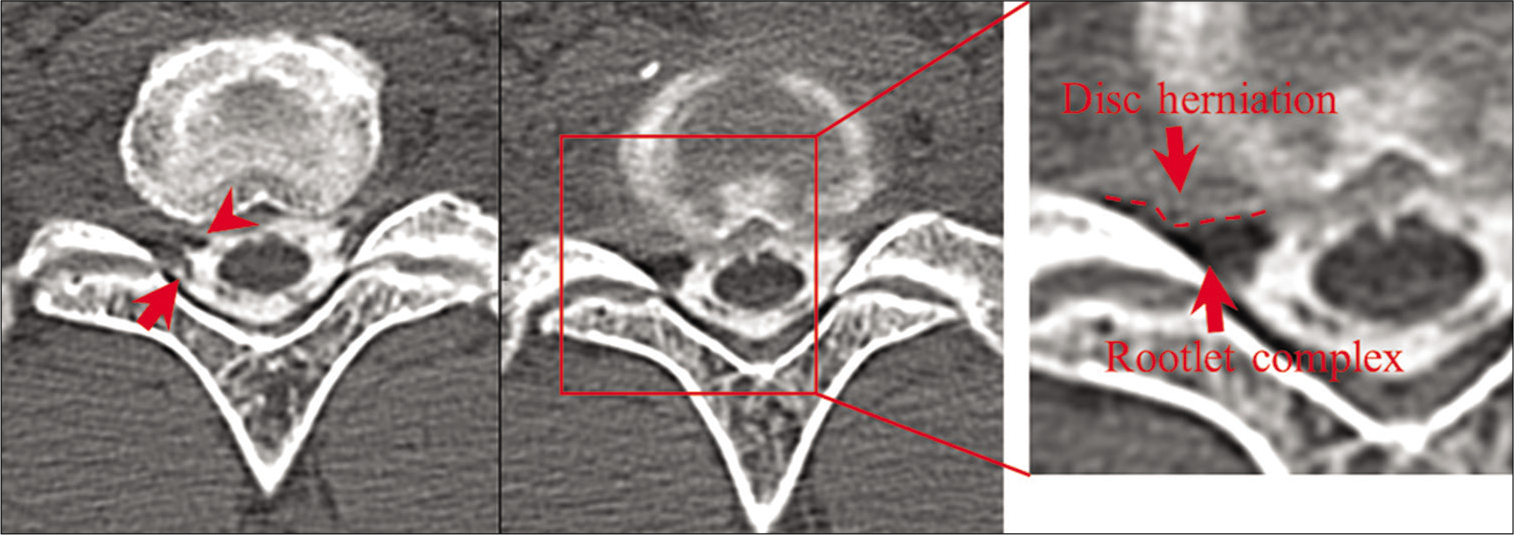
Figure 5:
Horizontal section of computed tomography myelogram showing contrast-enhanced defects contributed by rootlet stagnation (arrowhead: ventral rootlet and arrow: dorsal rootlet). In this representative case, the disk contrast and rootlets complex could be clearly differentiated based on the density of CT images.
DISCUSSION
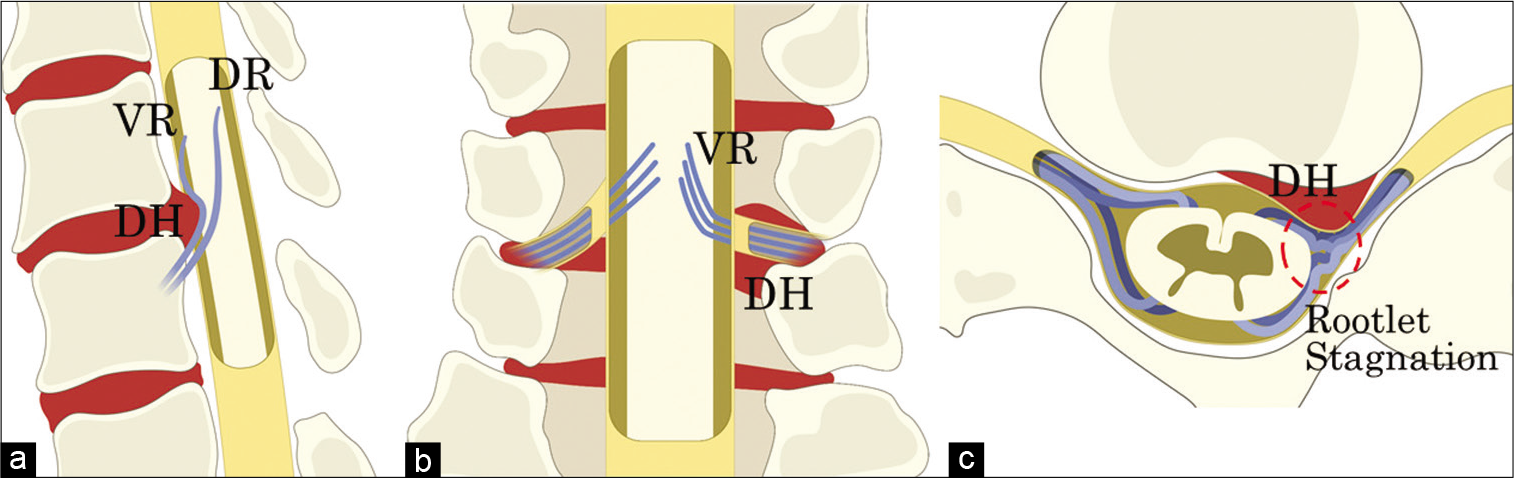
This study examined the efficacy of CTMs in displaying the morphological changes of the nerve rootlets in patients with cervical radiculopathy. Abnormal contrast-enhanced CTMs documented proximal compression of the cervical nerve roots (i.e., “rootlet stagnation sign”) on axial, sagittal, and coronal CTMs proximal to the compromised neural foramina [
Figure 6:
Illustrated images of the morphological changes in cervical nerve rootlets in cervical radiculopathy. (a) The sagittal image shows posterior deviation of the ventral rootlet due to anterior compression. (b) The coronal image shows the ventral rootlet coursing laterally, near the entrance of the intervertebral foramen. (c) The axial image shows the ventral and dorsal rootlets coming close together due to anterior compression at the proximal margin of the compression in the dural canal, and the rootlets appear to be stagnating near the entrance of the intervertebral foramen (“rootlet stagnation sign”). VR: Ventral root, DR: Dorsal root, and DH: Disk herniation.
CONCLUSION
For patients with cervical radiculopathy, preoperative CTMs document multiple abnormalities on the axial, sagittal, and coronal sections that provide further documentation as to whether anterior foraminotomies are warranted.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Sato S, Miyoshi S. A study of MRI findings and CT myelograms of the cervical foraminotomy cases. Nihon Sekitsuisekizuibyougakkai Zasshi. 2005. 16: 117
2. Song KJ, Choi BW, Kim GH, Kim JR. Clinical usefulness of CTmyelogram comparing with the MRI in degenerative cervical spinal disorders: Is CTM still useful for primary diagnostic tool?. J Spinal Disord Tech. 2009. 22: 353-7