- Department of Head and Neck Surgery, Neurosurgery Unit, Garibaldi Hospital, Catania, Italy
- Experimental Biomedicine and Clinical Neurosciences, School of Medicine, Postgraduate, Residency Program in Neurological Surgery, Neurosurgical Clinic, University Hospital “Paolo Giaccone”, Palermo, Italy
- Breast Surgery Unit, Garibaldi Hospital “Nesima”, Catania, Italy
- Anesthesiology and Intensive Care Unit, Garibaldi Hospital“Nesima”, Catania, Italy
- Department of Neurosurgery, Cannizzaro Hospital, Trauma and Gamma Knife Center, Catania, Italy.
Correspondence Address:
Gianluca Scalia, Department of Head and Neck Surgery, Neurosurgery Unit, Garibaldi Hospital, Catania, Italy.
DOI:10.25259/SNI_219_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gianluca Scalia1, Manikon Poullay Silven2, Roberta Costanzo2, Giancarlo Ponzo1, Agatino Florio1, Sara Pettinato3, Lucia Terranova4, Domenico Gerardo Iacopino2, Giuseppe Emmanuele Umana5, Giovanni Federico Nicoletti1. Motorboat propeller-related head injuries: A systematic literature review with a case illustration. 19-May-2023;14:175
How to cite this URL: Gianluca Scalia1, Manikon Poullay Silven2, Roberta Costanzo2, Giancarlo Ponzo1, Agatino Florio1, Sara Pettinato3, Lucia Terranova4, Domenico Gerardo Iacopino2, Giuseppe Emmanuele Umana5, Giovanni Federico Nicoletti1. Motorboat propeller-related head injuries: A systematic literature review with a case illustration. 19-May-2023;14:175. Available from: https://surgicalneurologyint.com/surgicalint-articles/12330/
Abstract
Background: Propeller-related injuries from motorboats are a major cause of injury in recreational water activities including severe and multiple lacerations that can promote scarring, blood loss, traumatic, or surgical amputations. The real incidence of these accidents is still unclear. The authors here present a systematic review of the literature, focusing on head injury, and related recommendations for its evaluation and management, also reporting a case of a female patient injured by a motorboat propeller.
Methods: A systematic literature review was conducted according to the preferred reporting items for systematic reviews and meta-analyses statement, with no limits in terms of publication date. The following Mesh and free text terms were identified: “motorboat and propeller and injuries” (107 results).
Results: A total of 12 papers were included in this systematic review. Only few case reports describing traumatic brain injury (TBI) have been documented. Out of a total of 90 cases analyzed, only five cases with TBI were reported. The authors also reported a case of a 12-year-old female, that during a boat trip, reported a severe polytrauma with concussive head trauma from a penetrating left fronto-temporo-parietal lesion, left mammary gland trauma and fracture of the left hand from falling into the water and impact with a motorboat propeller. She underwent an urgent left fronto-temporo-parietal decompressive craniectomy and then surgery with a multidisciplinary team. At the end of the surgical procedure, the patient was transferred to the pediatric intensive care unit. She was discharged on postoperative day 15. The patient was able to walk without assistance, with mild right hemiparesis and persistence of aphasia nominum.
Conclusion: Motorboat propeller injuries can result in extensive damage to soft tissue and bones with severe functional disability, amputations, and high mortality. There are still no recommendations and protocols for the management of motorboat propeller related injuries. Although there are several potential solutions that aim to prevent or ease motorboat-propeller injuries, there are still lack of consistent regulations.
Keywords: Hemicraniectomy, Infections, Motorboat, Propeller, Traumatic brain injury
INTRODUCTION
Propeller-related injuries associated to falls, drowning and burns, can occur during boating recreational activities. Propeller injuries from motorboats are a major cause of injury in recreational water activities including deep, multiple, and parallel lacerations that can promote scarring, blood loss, and traumatic or surgical amputations.[
The real incidence of these accidents is still unclear. During a period from 2009 to 2013, there were 915 reported cases of propeller injuries, with 129 deaths (14.1%) in the USA and 2.6% related to propeller strikes, with overall fatality rate of 15–23%, and a similar rate of major amputations.[
Head trauma has been reported as the most common cause of death with up to 40% of deaths with a fatality rate from 1976 to 1990 of 0.3–1.3%.[
Furthermore, serious late-onset complications such as wound infection, near drowning injuries, and hypothermia can occur, often with unusual bacteria that may not be detected by routine blood culture sampling.[
Herein, the authors present a case of a female patient injured by a motorboat propeller with a review of the literature, focusing on head injury, and related recommendations for its evaluation and management.
MATERIALS AND METHODS
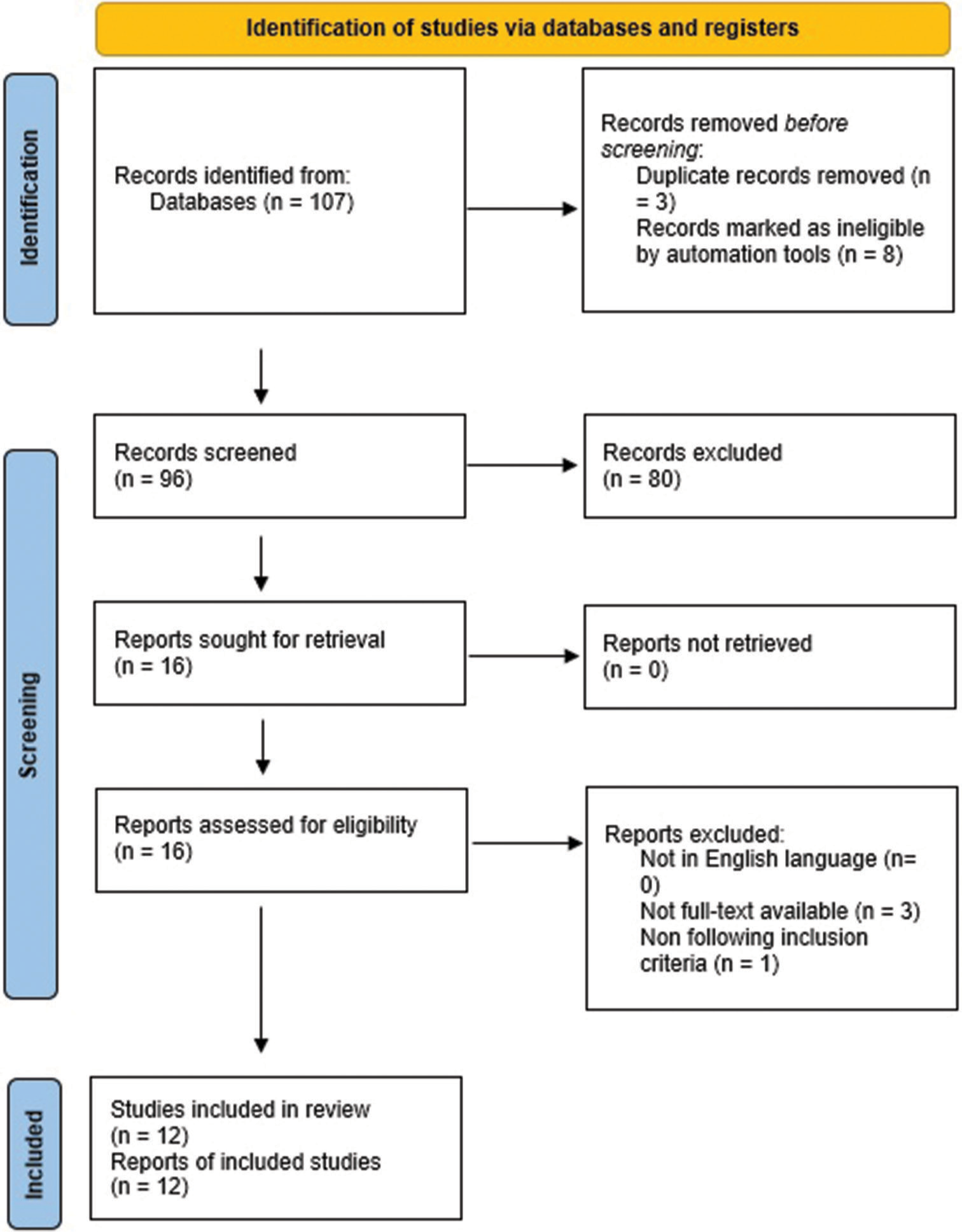
A systematic literature review was conducted according to the preferred reporting items for systematic reviews and meta-analyses statement, with no limits in terms of publication date [
Elegibility criteria
The articles were selected according to the following inclusion criteria:
Full article in English Human subjects Clinical studies (case reports, case series, and retrospective studies) Studies focusing on head trauma Studies focusing on severe speedboat-related injuries.
Exclusion criteria
The following criteria were excluded from the study:
Articles not in English Meta-analysis.
Data extraction
The available data included authors, year, study design, number of patients, sex, age, injuries, injury type, eventual surgical amputation, and death.
RESULTS
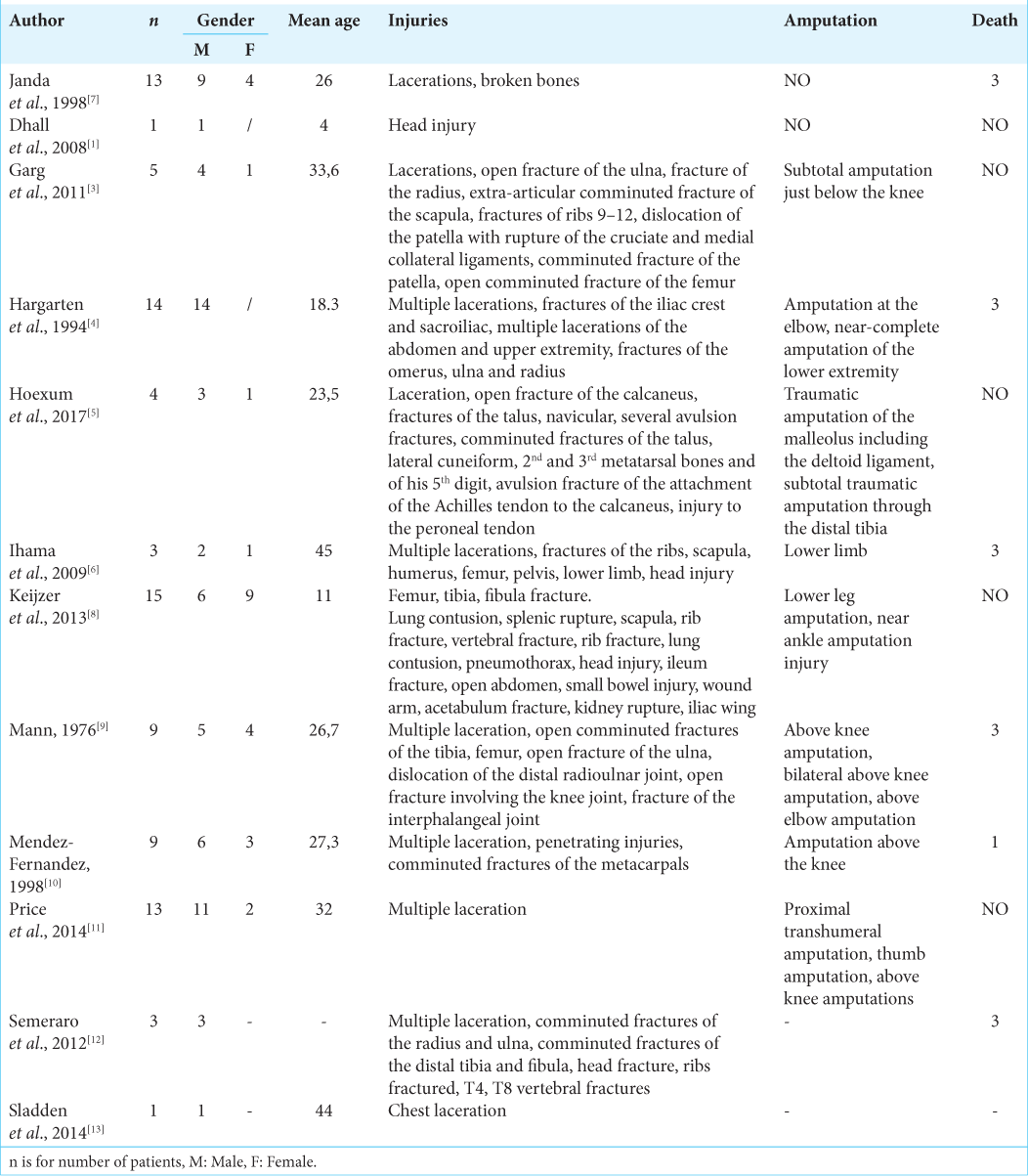
A total of 107 published studies were identified through PubMed and Google Scholar databases and additional reference list searches. After removing duplicates, the papers screened were n = 96. Based on the titles and abstracts, the authors then excluded n = 80 articles. The titles and abstracts of the articles identified during the literature search were reviewed to check if they fulfilled the following inclusion criteria: full article in English, human subjects, clinical studies (case reports, case series, and retrospective studies), and studies focusing on head trauma and severe speedboat-related injuries. The articles that remained were assessed in full against exclusion criteria: articles not in English and meta-analysis. Three articles were not retrieved due to the unavailability of the full text, no article was excluded because not in English language. Then, another one paper was excluded due to incompatibility with our eligibility criteria. Finally, a total of 12 papers were included in this systematic review [
Case description
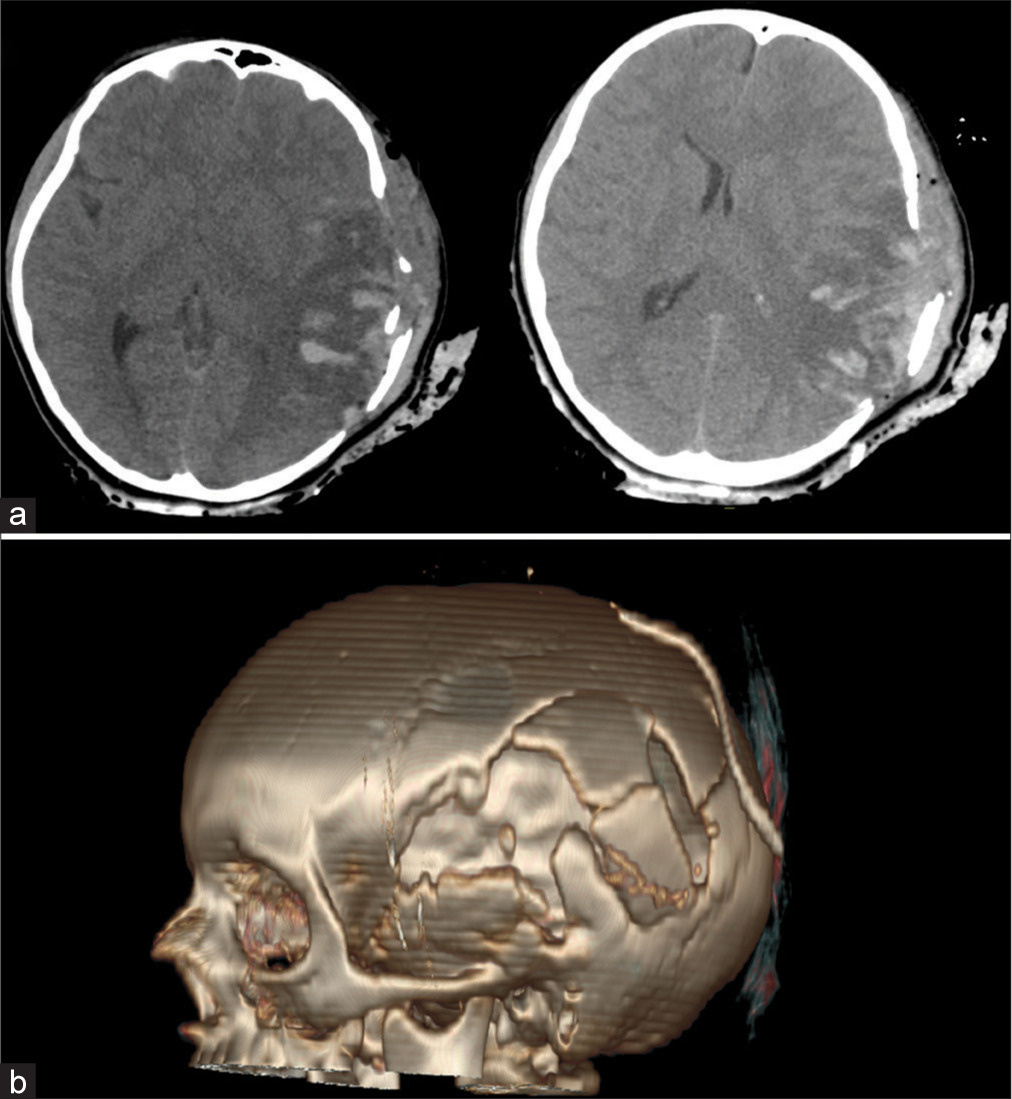
A 12-year-old female, during a boat trip, reported a severe polytrauma characterized by concussive head trauma from a penetrating left fronto-temporo-parietal lesion, lacerated-contusive trauma of the chest wall, left mammary gland trauma (multiple contused lacerated wounds with loss of substance and necrotic areas), and fracture of the left hand from falling into the water and impact with a motorboat propeller [
Figure 2:
Preoperative images after basic life support procedures showing concussive head trauma from a penetrating left frontotemporo-parietal lesion (a) lacerated-contusive trauma of the chest wall, left mammary gland trauma (multiple contused lacerated wounds with loss of substance and necrotic areas) and fracture of the left hand from falling into the water and impact with a motorboat propeller (b).
The patient sedated and intubated, was transferred to our institution. She immediately performed a brain computed tomography (CT) scan that showed multiple left frontotemporo-parietal skull fractures and contusive-hemorrhagic lesions [
She underwent an urgent left fronto-temporo-parietal decompressive craniectomy. At the end of the surgical procedure, the patient was transferred to the pediatric intensive care unit (ICU).
The following day, she underwent surgery with a multidisciplinary team (breast and orthopedic surgery) consisting of curettage and remodeling of the left breast, revision of the multiple lacerated contusive wounds of the left axillary cavity and left wrist with inspection, reduction, and fixation with Kirschner wires of the 1st and 2nd finger fractures. During hospitalization in pediatric ICU, she underwent seriated head CT scan and brain magnetic resonance imaging which documented diffuse cerebral damage in the left frontotemporo-parietal lobe.
After surgery, she presented aphasia nominum and right hemiparesis. Nonetheless, during hospitalization, the patient showed a progressive neurological improvement, recovering also cognitive functions.
She was discharged on postoperative day 15. The patient was able to walk without assistance, with mild right hemiparesis and persistence of aphasia nominum. She was therefore discharged with a program of hospitalization to another country (England) for neurorehabilitation and cranioplasty planning.
DISCUSSION
Every year the water recreation demand is increasing, and that clearly increase the incidence of boating-related injuries.[
Propeller strikes are often an indirect consequence of an evolving in progress accident and the injuries are sustained by the impact of the moving propeller blades.[
Usually, the first event can be represented by: man overboard, collision, running aground, capsizing, sudden acceleration or deceleration, mechanical failure, red wave hit, and high wake hit.[
Water sports, such as skiing and wakeboarding, pose the highest risk of propeller injuries, mainly due to the repeated close interaction with the moving motorboat.[
Wounds include repeated, deep, and sharp parallel lacerations with potential loss of bone and soft-tissue structures, more frequently involving lower limbs.[
In the paper described by Ihama et al., the autopsy reports two patients who died after TBI. In the first case, the patient died after a brain injury due to the chop wound on the head that exposed the cranial vault and the left hemisphere of the brain was missing. In the second case, the patient died after a brain injury due to a severe deep chop wound on the forehead with a skull fracture that exposed the cranial vault and lacerated the frontal lobes bilaterally, slight subarachnoid hemorrhage, and coagulated hematoma in both cerebral lateral ventricles.[
Dhall et al. reported a pediatric case of TBI characterized by intracerebral hemorrhage and edema that underwent a decompressive left-sided hemicraniectomy, evacuation of hemorrhage, and wound debridement.[
The management protocols for these wounds are multidisciplinary and should evaluate several factors such as the size and location of the wounds, the associated lesions, and the level of contamination.[
Diagnostic imaging is essential to evaluate a patient after a traumatic injury. In stable patients, the use of abdominal and pelvis CT scans with contrast is indicated for the evaluation of gynecological lesions, while CT scans with rectal contrast and rigid proctoscopy for the evaluation of colorectal lesions. However, it is important to consider the instability of the trauma patient and evaluate the appropriateness of laparoscopy.[
The first surgical step involves extensive debridement, exploration, and rinsing of the wound in the operating room as soon as possible in highly contaminated open fractures or within 12 h in high-energy exposed fractures that are not highly contaminated.[
The propeller wounds become infested with bacteria from the aquatic environment.[
Therefore, antibiotic prophylaxis was recommended for 5–7 days depending on the severity of the trauma and the extent of the soft-tissue injury, with a combination of a penicillin with anti-pseudomonas/Aeromonas (e.g., piperacillin) with an aminoglycoside (e.g., gentamicin or tobramycin) or a third-generation cephalosporin with anti-pseudomonas activity (ceftazidime) or a fluoroquinolone (e.g., ciprofloxacin). Optionally, a third-generation cephalosporin with anti-pseudomonas activity (ceftazidime) or a fluoroquinolone (e.g., ciprofloxacin) is given for penicillin-allergic patients. For saltwater injuries, however, an aminoglycoside with the addition of doxycycline is recommended to cover the infection caused by Vibrio spp., which can cause early infections associated with saltwater environments.[
Necrotizing fasciitis is the most severe consequence of wound that were exposed to the water.[
The current public health measures to prevent traumatic injuries in marine environments include the use of life jackets, the installation of engine cutoff switches (ECOS), and the prohibition of hazardous activities. The life jacket can not only save life, but also preserve body heat and clarity of mind by raising the head and chest above the water surface, as well as make it easier to locate and rescue an injured person.[
However, due to poor legislation mandating their use, most swimmers and boaters do not regularly wear a life jacket during water activities. Furthermore, it has been noted that one of the reasons mariners do not wear life jackets is out of concern that it may make them appear inexperienced or unable to swim. Another safety device is the use of ECOS on boats or on water scooters. It is a physical or wireless connections, that is connected to the boat operator and that automatically shut off the engine if the connection is even temporarily interrupted. However, the use of such a device is completely circumvented because of the lack of sufficient consideration and explanation on how to use it properly.[
CONCLUSION
Motorboat propeller injuries can result in extensive damage to soft tissue and bones with severe functional disability, amputation, and even exitus. To date, there are still no recommendations and protocols for the management of motorboat propeller-related injuries.
Although there are several potential solutions that aim to prevent or ease motorboat-propeller injuries, there are still lack of consistent regulations.
Enhancing safety measures through education and a strong law enforcement support, in conjunction with the development of effective safety devices, has the potential to decrease the incidence of these injuries.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Dhall SS, Lin FJ, Tumialan LM, Mapstone TB. Significant neurologic recovery following a catastrophic open head injury from a motorboat propeller: Case illustration. J Trauma. 2008. 65: 249-50
2. Ehrhardt JD, Newsome K, Das S, McKenney M, Elkbuli A. Evaluation and management of watercraft-related injuries for acute care surgeons: Towards improving care and implementing effective public health prevention policies. Ann Surg. 2022. 3: e149
3. Garg H, Twerenbold R, Zellweger R. Propeller and jet-ski injuries during Christmas and New Year in Western Australia. Med J Aust. 2011. 195: 704-5
4. Hargarten SW, Karlson T, Vernick JS, Aprahamian C. Motorboat propeller injuries in Wisconsin: Enumeration and prevention. J Trauma. 1994. 37: 187-90
5. Hoexum F, van Delft EA, van Couwelaar G, van der Steeg AF, Ang CW, Geeraedts LG. Motorboat propeller injuries: A case series and review of the literature. Trauma Mon. 2017. 22: e40270
6. Ihama Y, Ninomiya K, Noguchi M, Fuke C, Miyazaki T. Fatal propeller injuries: Three autopsy case reports. J Forensic Leg Med. 2009. 16: 420-3
7. Janda S, Perez C, Hospital B, Rast AM, Cherry D, Hunteman J, editors. From the Centers for Disease Control and Prevention Leads from the Morbidity and Mortality Weekly Report. Atlanta, GA: CDC; 1998. 47: 47
8. Keijzer R, Smith GF, Georgeson KE, Muensterer OJ. Watercraft and watersport injuries in children: Trauma mechanisms and proposed prevention strategies. J Pediatr Surg. 2013. 48: 1757-61
9. Mann RJ. Propeller injuries. South Med J. 1976. 69: 567-9
10. Mendez-Fernandez MA. Motorboat propeller injuries. Ann Plast Surg. 1998. 41: 113-8
11. Price CT, Muszynski MJ, Zielinski JA, Stewart C. Motorboat propeller injuries: Report of thirteen cases with review of mechanism of injury and bacterial considerations. J Trauma Treat. 2014. 4: 267
12. Semeraro D, Passalacqua NV, Symes S, Gilson T. Patterns of trauma induced by motorboat and ferry propellers as illustrated by three known cases from Rhode Island. J Forensic Sci. 2012. 57: 1625-9
13. Sladden D, Casha AR, Manche’ A. Chest wall reconstruction following a speedboat propeller injury. Malta Med J. 2014. 26: 48-51
14. Typical Propeller Accident Scenarios. Propeller Safety. Available from: http://www.propellersafety.com/propeller-accident-scenarios [Last accessed on 2023 Feb 28].