- School of Medicine, Georgetown University, Washington, DC, United States.
- Department of Neurosurgery, MedStar Georgetown University Hospital, Washington, DC, United States.
Correspondence Address:
V. Peter Abdow III, School of Medicine, Georgetown University, Washington, DC, United States.
DOI:10.25259/SNI_593_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: V. Peter Abdow III1, Jeffrey M. Breton2, Vikram V. Nayar2. Multiple craniotomies for the resection of symptomatic multifocal intracranial metastatic cardiac myxoma: A case report. 08-Sep-2023;14:322
How to cite this URL: V. Peter Abdow III1, Jeffrey M. Breton2, Vikram V. Nayar2. Multiple craniotomies for the resection of symptomatic multifocal intracranial metastatic cardiac myxoma: A case report. 08-Sep-2023;14:322. Available from: https://surgicalneurologyint.com/surgicalint-articles/12533/
Abstract
Background: Myxomas, rare benign mesenchymal lesions, are the most common cardiac tumors. Patients may rarely develop hematogenous metastasis to the brain, which can present as new-onset neurological deficits that correlate with multifocal hemorrhagic lesions on imaging. Limited guidelines presently exist for the treatment of such lesions. This report outlines a unique case involving three craniotomies and failed radiation therapy in the treatment of metastatic cardiac myxoma.
Case Description: A 63-year-old woman presented with a right middle cerebral artery embolic stroke secondary to a left atrial myxoma and multifocal hemorrhagic lesions consistent with intracranial metastasis. She had a right frontal craniotomy for tumor resection, followed by stereotactic radiosurgery, though this did not arrest disease progression. She later had a left occipital craniotomy for a symptomatic lesion. More than two years after her initial presentation, she returned with acute-onset symptoms correlating to growth in a left frontal lesion requiring another resection. Following this third craniotomy, imaging has not revealed the progression of metastatic intracranial disease. She is pursuing further treatment through primary cardiac tumor resection.
Conclusion: Although rare, hematogenous seeding with subsequent formation of hemorrhagic metastasis is a possible complication of atrial myxoma. While surgical resection, radiation therapy, and chemotherapy have historically been used, no standard of care currently exists. This case demonstrates repeat tumor resection as effective for managing symptomatic intracranial metastatic myxoma in a patient with poor response to radiation therapy and multiple recurrences, with follow-up showing improvement in neurological symptoms and mass effect and absence of recurrence on imaging.
Keywords: Case report, Craniotomy, Metastatic myxoma, Recurrent myxoma
INTRODUCTION
Myxomas, rare benign lesions believed to derive from multipotent mesenchymal cells, are the most common cardiac tumors. Current estimates suggest that about 75% of myxomas develop in the left atrium, putting patients at greater risk for systemic thromboembolic events.[
This report outlines a detailed description of a unique case involving a patient requiring three craniotomies for myxoma resection for symptomatic lesions after radiation therapy failed to halt disease progression.
CASE DESCRIPTION
A 63-year-old woman initially presented with acute onset of left-sided facial droop, numbness, and weakness concerning for right middle cerebral artery stroke. Computed tomography (CT) of the head was unremarkable, and CT angiography (CTA) showed occlusion of the distal right M1 segment. She received tissue plasminogen activator (tPA) and was transferred to our facility for endovascular thrombectomy with thrombolysis in cerebral infarction (TICI) 2a recanalization. The etiology was determined to be thromboembolic and a cardiac workup revealed a large left atrial mass attached to the interatrial septum, consistent with the left atrial myxoma. This was later confirmed histopathologically following urgent surgical resection of the myxoma and repair of an associated atrial septal defect.
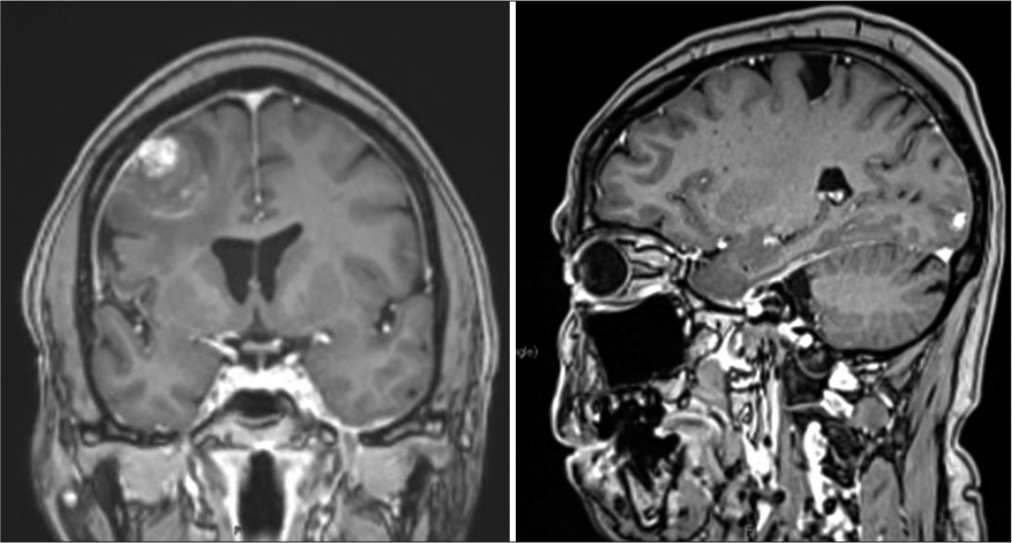
Eight months later, she presented again after a fall and possible seizure. CT showed the right frontal intracranial hemorrhage (ICH) in her prior stroke bed, as well as small left frontal and occipital ICHs. Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) confirmed multifocal hemorrhagic lesions in these areas concerning hemorrhagic metastatic lesions [
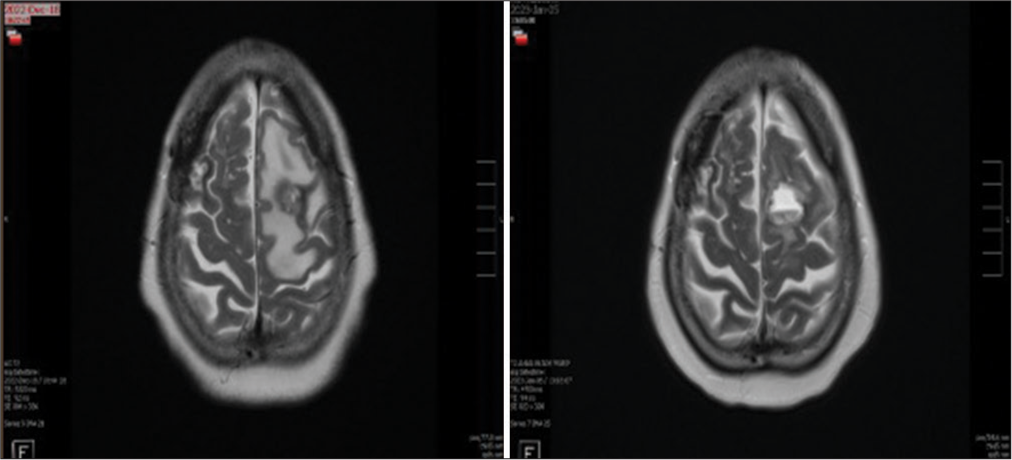
She underwent stereotactic radiosurgery (SRS) to the postoperative right frontal region and left frontal and occipital lesions, though this did not arrest disease progression. She did not undergo chemotherapy given a paucity of data to guide oncological recommendations. Thirteen months after her initial presentation, she experienced blurry vision and a right visual field defect, with associated interval growth in the left occipital lesion and significant vasogenic edema, for which she underwent a left occipital craniotomy. One year later, she presented with delays in speech, cognition, and movement and was found to have interval growth in the left frontal lesion [
MRI 4 months postoperatively showed no signs of disease. The right ventricular mass has been stable on repeat imaging and she has remained hemodynamically stable. Cardiac workup has not revealed cardiac or pulmonary right-to-left shunting, making paradoxical embolization less likely as an etiology for new metastatic lesions. She awaits further evaluation for repeat cardiac surgery.
CONCLUSION
Although rarely encountered, hematogenous seeding with subsequent formation of hemorrhagic metastasis is a possible complication of atrial myxoma, a classically benign lesion that should not be ignored. The potential for myxomatous embolism is thought to be due to the tumor’s friable and villous qualities, as well as its tendency to degenerate, either through fibrosis, necrosis, thrombosis, calcification, or Gamna–Gandy body formation.[
Surgical resection can be considered in patients with relatively few metastases, unstable conditions, or progressive neurologic deficits.[
In summary, this unique case report demonstrates repeat tumor resection as an effective method for managing symptomatic intracranial metastatic myxoma in a patient with poor response to radiation therapy and multiple recurrences, with follow-up showing improvement in neurological symptoms and mass effect secondary to her intracranial lesions, as well as the absence of recurrence on imaging.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Côté I, Sinclair J, Woulfe J, Glikstein R, Veinot J. Cerebral metastasis presenting after complete primary resection of atrial myxoma: Case report. Can J Neurol Sci. 2015. 42: 457-60
2. Giannoni S, Pizzanelli C, Frosini D, Canovetti S, Mancuso M, Siciliano G. Hemorrhagic cerebral metastases presenting after complete resection of atrial myxoma: A case report with a favorable outcome and review of the literature. J Case Rep Imaging. 2021. 5: 42
3. Kabir R, Qamer SZ, Shadman S, Ben-Dor I, Slack MC Shults CC. Recurrent cardiac myxoma complicated by brain metastases: Role of multimodality imaging in diagnosis and management. J Am Coll Cardiol. 2022. 79: 3098
4. Ma K, Zhao D, Li X, Duan H, Yan C, Wang S. Case report: Multiple brain metastases of atrial myxoma: Clinical experience and literature review. Front Neurol. 2023. 13: 1046441
5. Maas JA, Menes M, Siomin V. Cardiac myxoma with cerebral metastases and chronic lymphocytic leukemia/small lymphocytic lymphoma: A case report and review. J Neurol Surg Rep. 2020. 81: e1-6
6. Nguyen T, Vaidya Y, editors. Atrial myxoma. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. p. Available from: https://ncbi.nlm.nih.gov/books/NBK556040 [Last accessed on 2023 Aug 22]
7. Rajeshwari M, Subramanian P, Suri V, Nambirajan A, Garg A, Vibha D. Metastatic lesions of atrial myxoma. A pathologist can clinch them all. Neuropathology. 2020. 40: 295-301
8. Wan Y, Du H, Zhang L, Guo S, Xu L, Li Y. Multiple cerebral metastases and metastatic aneurysms in patients with left atrial myxoma: A case report. BMC Neurol. 2019. 19: 249