- Department of Neurosurgery, Neuroscience Research Center, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon
- Faculty of Medicine, American University of Beirut, Beirut, Lebanon
- Department of Biology, Faculty of Arts and Sciences, American University of Beirut, Beirut, Lebanon
Correspondence Address:
Jawad Fares, Youssef Fares
Department of Neurosurgery, Neuroscience Research Center, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon
DOI:10.4103/sni.sni_445_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jawad Fares, Mohamad Y. Fares, Youssef Fares. Musculoskeletal neck pain in children and adolescents: Risk factors and complications. 10-May-2017;8:72
How to cite this URL: Jawad Fares, Mohamad Y. Fares, Youssef Fares. Musculoskeletal neck pain in children and adolescents: Risk factors and complications. 10-May-2017;8:72. Available from: http://surgicalneurologyint.com/surgicalint-articles/musculoskeletal-neck-pain-in-children-and-adolescents-risk-factors-and-complications/
Abstract
Background:Neck pain is a major public health concern that has been extensively studied in adults but not in children and adolescents. Therefore, the purpose of this article is to explore musculoskeletal neck pain in children and adolescents, as well as to discuss its possible risk factors and complications.
Methods:Participants were patients under 18 years of age, who had presented to the clinic (Beirut, Lebanon) in 2015, with nonspecific neck pain. They were examined and asked to evaluate and localize the pain. Neck positioning during various activities along with other complications were explored. Patients reporting pain associated with congenital or systemic diseases and fractures were excluded.
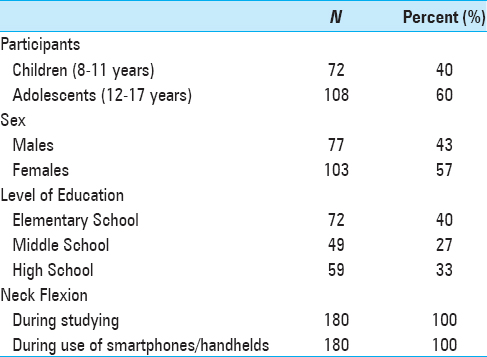
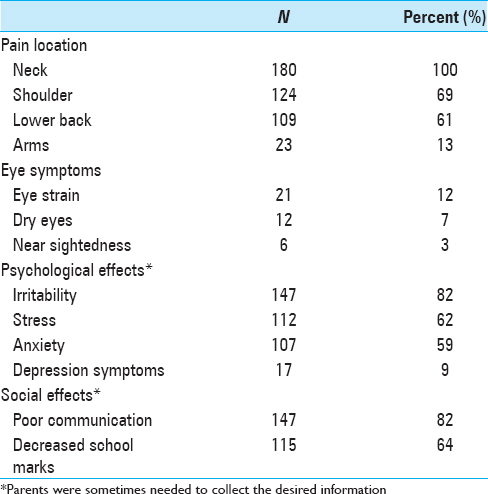
Results:Two-hundred-and-seven children and adolescents presented with nonspecific neck pain. Musculoskeletal neck pain with spasm was diagnosed in 180 patients (N = 180). Participants did not show any findings on physical examination and radiological studies, and had no comorbidities. More females (57%) than males (43%) and more adolescents (60%) than children (40%) were affected. All the 180 participants (100%) reported flawed flexion of their back and neck while studying and/or using smartphones and tablets. Eye symptoms were reported in 21% of the cases, and parents of most participants (82%) reported a change in the psychological and social behavior of their children.
Conclusions:Musculoskeletal neck pain is an important disease in children and adolescents with numerous risk factors contributing to its development. Increased stresses regarding the cervical spine may lead to cervical degeneration along with other developmental, medical, psychological, and social complications.
Keywords: Adolescents, children, neck flexion, neck pain, smartphones, text neck
INTRODUCTION
Neck pain is a major public health problem in modern societies.[
Prevalence data have shown that, in a general population, the 1-year incidence of neck pain can be as high as 40%.[
Although the epidemiology, burden, and treatment of musculoskeletal pain have been extensively explored in adults, the same is not true for children. The lack of clinical research pertinent to children and adolescents has been emphasized by multiple studies.[
As the surge in prevalence of musculoskeletal conditions occurs in childhood and adolescence, it may be necessary to investigate the condition at these stages of life.[
Therefore, the purpose of this article is to explore musculoskeletal neck pain in children and adolescents under 18 years of age, and to discuss possible risk factors and complications related to this pain.
MATERIALS AND METHODS
This study explored cases that presented to our clinic in Beirut, Lebanon, in 2015 with nonspecific neck pain. Demographic information including age, sex, level of education, use of technology, and study habits were collected from individuals and their parents.
Interviewed individuals were under 18 years of age. Those whose ages ranged between 8 and 11 years were considered children, and those whose ages ranged between 12 and 17 years were considered adolescents. Patients were asked to localize the pain on themselves and on a model provided to them. Neurological assessment was conducted to test for sensory and motor deficits. Individuals were also asked about their pertinent daily habits, studying conditions, sitting positions, and sleeping positions. Further investigation explored the use of technology such as cell phones, tablets, computers, and television; participants were asked to show their usual neck position when engaged in these activities. All interviewees underwent radiological studies by radiography to rule out scoliosis or any other pathologies at the cervical spine level. In addition, psychological and social symptoms were investigated.
For the purposes of this study, we did not include patients reporting pain associated with congenital or systemic diseases, such as scoliosis. We also excluded patients reporting pain resulting from frank injuries, such as fractures, and pain following surgical interventions. Chronic neck pain was defined as continuous neck complaints for more than 6 months.
RESULTS
In total, 207 children and adolescents presented with nonspecific neck pain. All patients reported having cervical neck pain of more than 6 months’ duration that radiates dorsally down the back and to the shoulders. None had sensory or motor deficits. Twenty-seven patients were found to have dorsolumbar scoliosis and were excluded from the study. The remaining 180 patients did not show any finding on physical examination and radiological studies, and had no comorbidities. They were diagnosed with musculoskeletal neck pain with spasm, and were the focus of our study (N = 180). Ages ranged between 8 and 17 years, with a mean age of 14 years. Demographics of the children and adolescents participating in the study are presented in
All the 180 participants (100%) reported flawed flexion of their back and neck while studying. They also admitted to using smartphones and/or tablets. When asked to demonstrate how they used these devices, all participants (100%) showed strong flexion of the neck (≥45 degrees) when engaged in the activity. Children and adolescents in our sample spent an average of 5 and 7 hours a day, respectively, on their smartphones and handheld devices.
A change in behavior, defined by a change in daily habits and usual social interactions, as noticed by parents, was reported in 147 young participants (82%). They were described as having become more irritable and alienated. Parents of 115 participants (64%) reported that their grades in school have been declining.
DISCUSSION
Musculoskeletal neck pain in children and adolescents is very common. Almost 87% (180 of 207) of the children and adolescents presented in our study were diagnosed with musculoskeletal neck pain. Other studies and reviews have shown 1-year incidences of 28% and 40% for neck pain.[
All our participants reported flexing their back and neck while studying. Ariëns et al.[
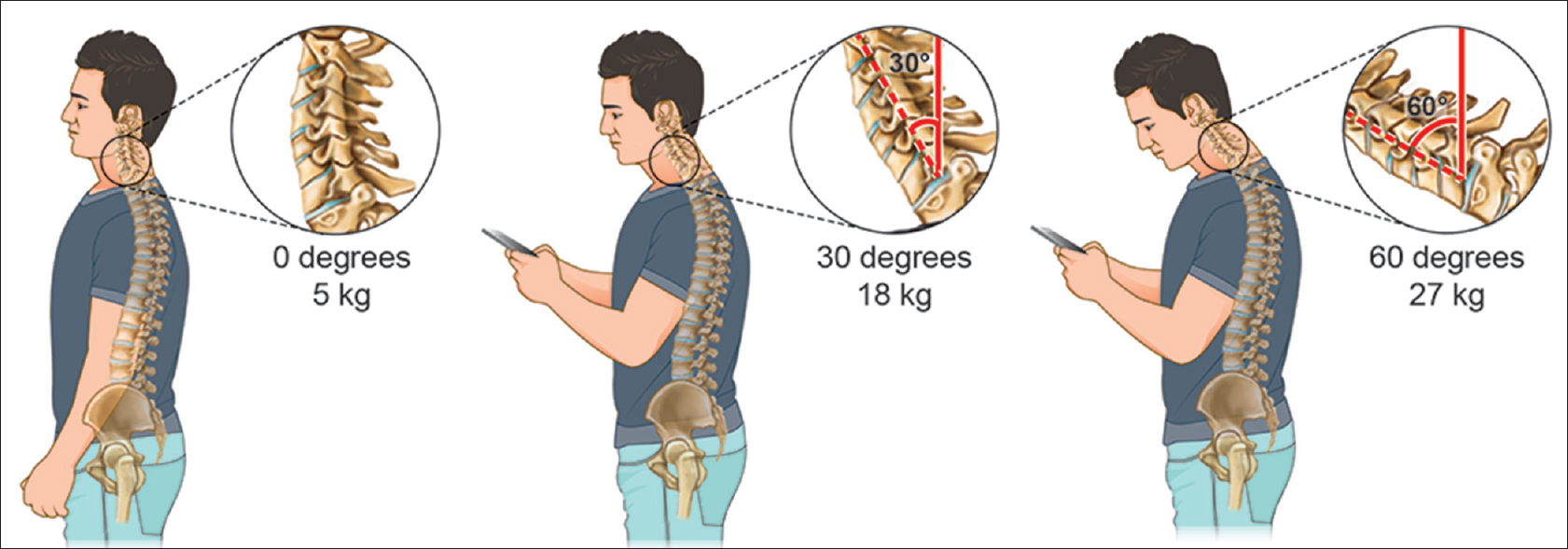
The weight put on the spine dramatically increases when flexing the head forward at varying degrees [
Figure 1
A chart depicting the stress and weight put on the neck and spine as a result of hunching over a smartphone and handheld devices at varying degrees. The neck flexion angle is the angle between the global vertical and the vector pointing from C7 to the occipitocervical joint. A full-grown head weighs 5 kg in the neutral position. As the head bends forward, the weight seen by the neck increases to 18 kg at 30° and 27 kg at 60°
The effects of forward flexion of the neck transcend pain to contribute to more associated complications. Often times, the effects of prolonged neck flexion can contribute to nearsightedness, eye strain, or dry eyes, as the eyes are forced to focus on an object placed nearby.[
Emre et al.[
Parents of most of our participants reported that their children have become more isolated and easily irritable. In addition, their grades in school have been negatively affected. Children who use more than the expert recommended 1–2 hours per day of technology, have a 60% increase in psychological disorders.[
The lack of validated instruments to measure musculoskeletal neck pain and its consequences in children and adolescents is a limitation in similar studies. This is due to the fact that it becomes difficult to draw conclusions and compare between different samples, populations, and cultures. In addition, the method of administration is critical because self-administered instruments cannot be conducted among illiterate and young children, and the need for a parent to collect information may hinder the pain evaluation process.
Future studies should aim to find a unified instrument to measure musculoskeletal neck pain, and validation across cultures should occur. The pathways and mechanisms for the association of pain experienced in childhood and pain experienced in adulthood are unknown. It can be hypothesized that a physiological or behavioral trigger is set when a child has a particular painful experience, which predisposes them to pain as an adult. Genetic susceptibility may also underlie the experience of pain. Future studies can aim to explore these mechanisms. Moreover, there is a particular need for studies to investigate the nature of the relationships between neck pain and other adverse health risk factors.
CONCLUSIONS
Musculoskeletal neck pain is a common multifactorial disease in children and adolescents, implying that there are numerous risk factors contributing to its development. Bending the head, neck, and shoulders over cell phones and handheld devices, along with distorted neck positioning when sitting, studying, and watching television, can lead to incrementally increased stresses in the cervical spine area. These stresses may lead to early wear, tear, degeneration, and possibly surgeries. Other developmental, medical, psychological, and social complications are also of concern. While it is nearly impossible to avoid the habits and technologies that cause these issues, young individuals should make an effort to perform activities with a neutral spine and to avoid neck flexion for hours each day.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ariëns GAM, Borghouts JAJ, Koes BW, Crombie IK, Croft PR, Linton SJ, LeResche L, Korff M.editors. Neck pain. Epidemiology of pain. Seattle: IASP Press; 1999. p. 235-6
2. Bogduk N. Neck pain. Aust Fam Physician. 1984. 13: 26-30
3. Bogduk N. Neck pain: An update. Aust Fam Physician. 1988. 17: 75-
4. Bouter LM, van der Wal G. Psychosocial risk factors for neck pain: A systematic review. Am J Ind Med. 2011. 39: 180-93
5. Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain. 2004. 8: 187-99
6. Last accessed on 2016 Sep 01. https://health.clevelandclinic.org/2015/03/text-neck-is-smartphone-use-causing-your-neck-pain/.
7. Cohen E, Uleryk E, Jasuja M, Parkin PC. An absence of pediatric randomized controlled trials in general medical journals, 1985–2004. J Clin Epidemiol. 2007. 60: 118-23
8. Last accessed on 2016 Sep 01. http://www.correctvision.com/eye-health/effects-of-texting/.
9. Curtis SLast accessed on 2016 Sep 01. http://www.telegraph.co.uk/technology/mobile-phones/10721014/Texting-for-long-periods-could-lower-lifeexpectancy.html.
10. Emre M, Cetiner S, Zencir S, Unlukurt I, Kahraman I, Topcu Z. Oxidative stress and apoptosis in relation to exposure to magnetic field. Cell Biochem Biophys. 2011. 59: 71-7
11. Fares J, Al Tabosh H, Saadeddin Z, El Mouhayyar C, Aridi H. Stress, burnout and coping strategies in preclinical medical students. N Am J Med Sci. 2016. 8: 75-
12. Fares J, Fares Y. The role of yoga in relieving medical student anxiety and stress. N Am J Med Sci. 2016. 8: 202-
13. Fares J, Saadeddin Z, Al Tabosh H, Aridi H, El Mouhayyar C, Koleilat MK. Extracurricular activities associated with stress and burnout in preclinical medical students. J Epidemiol Glob Health. 2016. 6: 177-85
14. Fares Y. Conseils pour une Colonne Vertebrale Saine. Beirut. 2000. p.
15. Fares Y, Fares J. Neurosurgery in Lebanon: History, Development, and Future Challenges. World Neurosurg. 2017. p.
16. Gandhi OP, Morgan LL, de Salles AA, Han YY, Herberman RB, Davis DL. Exposure limits: The underestimation of absorbed cell phone radiation, especially in children. Electromagn Biol Med. 2012. 31: 34-51
17. Graham JB. Impacts of Text Messaging on Adolescents’ Communication Skills: School Social Workers’ Perceptions. Master of Social Work Clinical Research Papers, Paper 184, St. Catherine University, St. Paul and Minneapolis, Minnesota, US. 2013. p.
18. Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014. 25: 277-9
19. Hestbaek L, Leboeuf-Yde C, Kyvik KO, Manniche C. The course of low back pain from adolescence to adulthood: Eight-year follow-up of 9600 twins. Spine. 2006. 31: 468-72
20. Hossmann KA, Hermann DM. Effects of electromagnetic radiation of mobile phones on the central nervous system. Bioelectromagnetics. 2003. 24: 49-62
21. Last accessed on 2016 Sep 01. http://vizhub.healthdata.org/gbd-compare/.
22. Jeffries LJ, Milanese SF, Grimmer-Somers KA. Epidemiology of adolescent spinal pain: A systematic overview of the research literature. Spine. 2007. 32: 2630-7
23. Jones GT, Silman AJ, Power C, Macfarlane GJ. Are common symptoms in childhood associated with chronic widespread body pain in adulthood?: Results from the 1958 british birth cohort study. Arthritis Rheum. 2007. 56: 1669-75
24. Kamper SJ, Henschke N, Hestbaek L, Dunn KM, Williams CM. Musculoskeletal pain in children and adolescents. Braz J Phys Ther. 2016. 20: 275-84
25. McBeth J, Jones K. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2007. 21: 403-25
26. Michaleff ZA, Kamper SJ, Maher CG, Evans R, Broderick C, Henschke N. Low back pain in children and adolescents: A systematic review and meta-analysis evaluating the effectiveness of conservative interventions. Eur Spine J. 2014. 23: 2046-58
27. Mössle T, Kleimann M, Rehbein F, Pfeiffer C. Media use and school achievement–boys at risk?. Br J Dev Psychol. 2010. 28: 699-725
28. Page AS, Cooper AR, Griew P, Jago R. Children's screen viewing is related to psychological difficulties irrespective of physical activity. Pediatrics. 2010. 126: e1011-7
29. Rodgers A. Managing chronic pain in children and adolescents. BMJ. 2002. 324: 1570-6
30. Taylor JB, Goode AP, George SZ, Cook CE. Incidence and risk factors for first-time incident low back pain: A systematic review and meta-analysis. Spine J. 2014. 14: 2299-319
31. Last accessed on 2016 Aug 29. http://text-neck.com/.
32. Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015. 386: 743-800