- Department of Neurosurgery, University of Pennsylvania, Perelman School of Medicine, Philadelphia, Pennsylvania, United States.
Correspondence Address:
Canada T. Montgomery, Department of Neurosurgery, University of Pennsylvania, Perelman School of Medicine, Philadelphia, Pennsylvania, United States.
DOI:10.25259/SNI_100_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Canada T. Montgomery, Rachel Blue, Michael Spadola, Sonia Ajmera, Rashad Jabarkheel, James Schuster. Navigated lumbar drain placement: A description of technique and case example. 31-Mar-2023;14:116
How to cite this URL: Canada T. Montgomery, Rachel Blue, Michael Spadola, Sonia Ajmera, Rashad Jabarkheel, James Schuster. Navigated lumbar drain placement: A description of technique and case example. 31-Mar-2023;14:116. Available from: https://surgicalneurologyint.com/surgicalint-articles/12226/
Abstract
Background: Lumbar drain (LD) placement can be a difficult procedure leading to postprocedure complications, particularly in patients with persistent cerebrospinal fluid leaks or a large body habitus. The objective of this technical case report is to describe the use of Medtronic’s SureTrak Navigation system for navigated LD placement.
Case Description: The patient was an 18-year-old morbidly obese male who initially underwent a suboccipital craniectomy with duraplasty and a C1 laminectomy for Chiari Malformation. Postoperatively, he developed a pseudomeningocele and was taken to the operating room for wound revision, duraplasty repair, and LD placement. Medtronic’s SureTrak Navigation system was used for LD placement before wound revision. Successful LD placement was achieved in a single pass using the SureTrak Navigation. The patient did well postoperatively, and LD removal occurred on postoperative day 6. The patient was discharged in good condition without evidence of a cerebral spinal fluid leak.
Conclusion: Navigation using the SureTrak system is a reasonable option to use in patients with a high body mass index and a persistent cerebrospinal fluid leak. When the patient is already undergoing an operative procedure, it can aid in an efficient low-risk intervention completed in a single prone positioning.
Keywords: Cerebrospinal fluid leak, Cerebrospinal fluid, Lumbar drain, Medtronic SureTrak, Navigation, Neurosurgery
INTRODUCTION
Lumbar cerebrospinal fluid (CSF) access is critical for the management and treatment of neurosurgical conditions. Lumbar access including both punctures and drains is often indicated for diagnostic workup to evaluate CSF, to treat diseases complicated by hydrocephalus, and to aid in cranial procedures to prevent the development of CSF fistulas and the need for brain retraction.[
LDs are typically placed at bedside or intraoperatively. In each situation, sterile technique is used with a designated LD toolkit. Yet, placement of the needle and catheter is performed blindly by the proceduralist. This blind approach introduces additional risks for the patient when multiple attempts are required. Multiple attempts at insertion can damage the dura and adjacent structures leading to unnecessary pain and distress for the patient, increased infection rate, extended length of the procedure, and potentially lasting neurological deficits.[
CASE DESCRIPTION
Navigation systems provide a reasonable adjunct for LD placement, particularly in cases, in which the patient is already going to the operating room for a concurrent CSF leak repair and in cases, where factors make LD placement a high-risk procedure, such as body habitus.
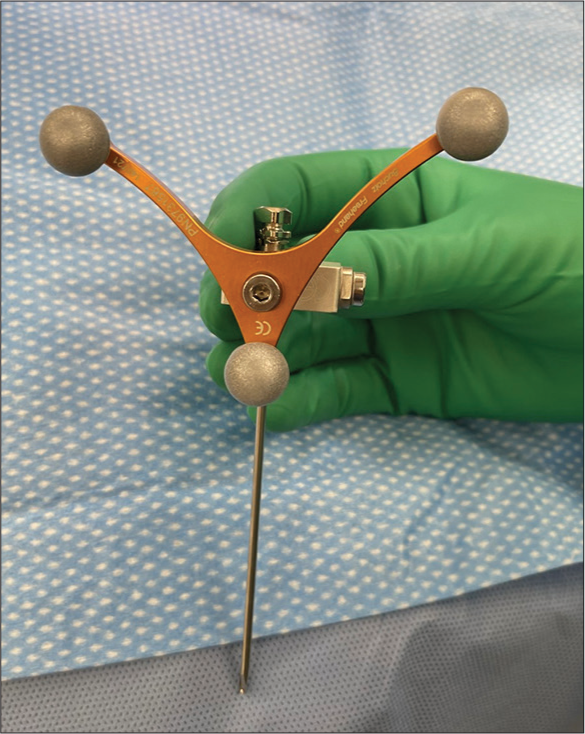
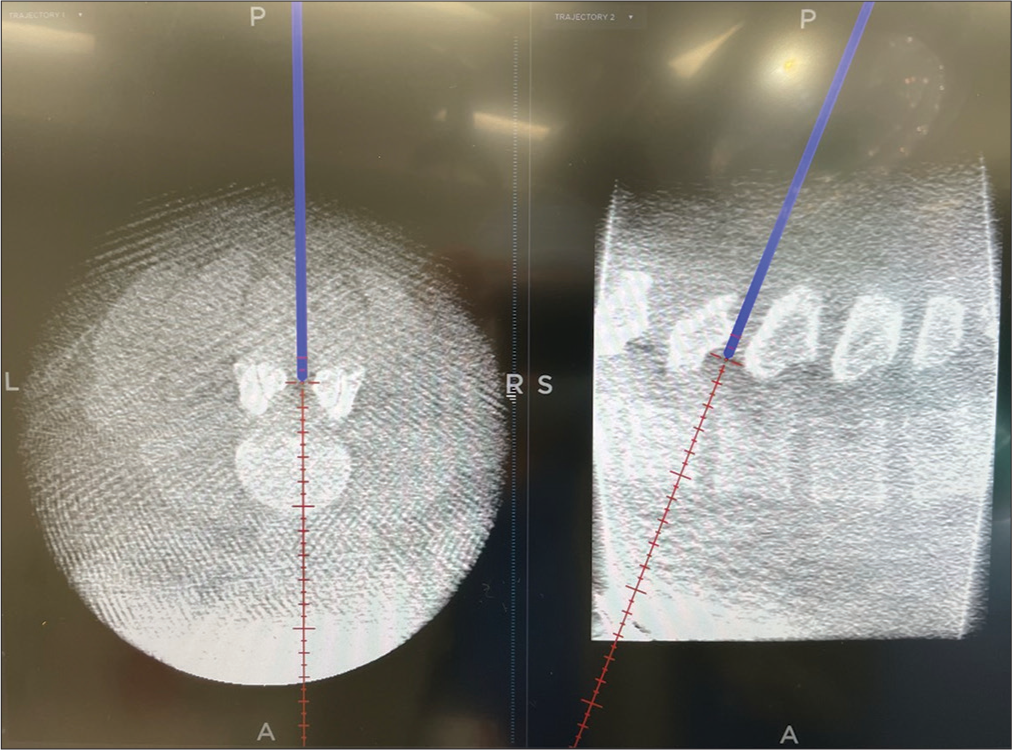
We utilize the Medtronic SureTrak system in patients undergoing CSF leak repair in the operating room. Patients are placed in the prone position and the reference frame is either secured with Ioban over the bony prominences of the thoracic spine, with care taken not to move the frame or patient during the procedure, or secured to the Mayfield headframe, if it is being used in the procedure. The optical array is placed at the head of the patient’s bed, facing the procedure field. An O-arm spin is completed and the SureTrak frame is then registered to the top portion of the spinal needle, ensuring the bevel and the frame are facing the head of the bed and optical array. The needle is tested on several anatomical points to ensure accuracy and LD placement is completed in typical fashion.[
CASE EXAMPLE
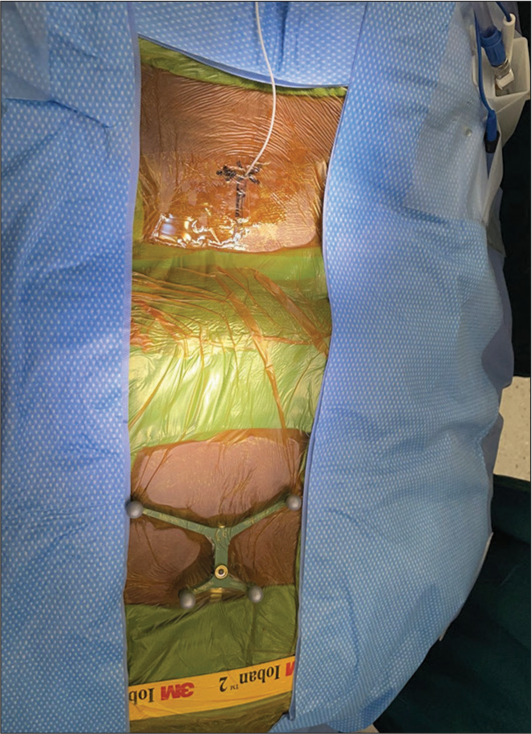
The patient was an 18-year-old male who was morbidly obese with a body mass index (BMI) of 46. He initially underwent a suboccipital craniectomy with duraplasty and a C1 laminectomy for Chiari Malformation and associated cervicothoracic syrinx. Postoperatively, he developed a pseudomeningocele with incisional drainage and was subsequently taken to the operating room for wound revision, duraplasty repair, and concurrent LD placement. The patient was placed in the prone position and the navigation reference frame was secured with Ioban over the thoracic spine [
DISCUSSION
An approach that may reduce the complications of LD insertion associated with multiple attempts is navigation. Especially in cases, where additional factors make LD placement a high-risk procedure like patient body habitus, utilizing a navigation-guided technique would be preferred. However, these navigation-guided approaches have not been reported for LD placement to our knowledge. In this report, we describe a case where we utilized Medtronic’s SureTrak system for navigated LD placement in an 18-year-old morbidly obese patient who developed a post-operative pseudomeningocele following a suboccipital craniectomy and a C1 laminectomy.
Postoperative pseudomeningoceles in the setting of CSF leaks and dural tears are the most common complication of posterior fossa decompression for Chiari malformation given the risk profile for CSF leaks is greater than other intradural spine procedures.[
Limitations
There are a few limitations to our technical case report. First, we only describe a single case example using the navigation SureTrak system for LD placement. Additional case series and comparative effectiveness studies evaluating SureTrak LD navigation to other LD placement techniques are needed to determine superiority. Second, the SureTrak system has its own drawbacks. There is potential for inaccuracy since the SureTrak reference frame is attached to the patient’s thoracic spine, a non-ridge object. Care should be taken to ensure the frame is not moved after the use of the O-arm. However, this is of little concern since the procedure is short and does not involve manipulation. In addition, procedural time and cost can increase with use of the O-arm spin especially if the patient was not originally scheduled for an operating room procedure. Still, we believe that the SureTrak navigation LD placement technique is a viable and likely time saving option for cases with known or perceived challenges.
CONCLUSION
Navigation using the SureTrak system is a reasonable option to use in patients with high BMI and persistent CSF leak. When the patient is already undergoing an operative procedure, it can aid in an efficient intervention completed in a single prone positioning.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Açikbaş SC, Akyüz M, Kazan S, Tuncer R. Complications of closed continuous lumbar drainage of cerebrospinal fluid. Acta Neurochir (Wien). 2002. 144: 475-80
2. Bakhshi SK, Suhail N, Mitha R, Moazzam M, Zahid N, Shamim MS. Lumbar drain for temporary cerebrospinal fluid diversion: Factors related to the risks of complications at a university hospital. World Neurosurg. 2020. 143: e193-8
3. Brook AD, Burns J, Dauer E, Schoendfeld AH, Miller TS. Comparison of CT and fluoroscopic guidance for lumbar puncture in an obese population with prior failed unguided attempt. J Neurointerv Surg. 2014. 6: 324-8
4. Costa F, Tosi G, Attuati L, Cardia A, Ortolina A, Grimaldi M. Radiation exposure in spine surgery using an image-guided system based on intraoperative cone-beam computed tomography: Analysis of 107 consecutive cases [published correction appears in J Neurosurg Spine 2017;26:542]. J Neurosurg Spine. 2016. 25: 654-9
5. Deen HG, Pettit PD, Sevin BU, Wharen RE, Reimer R. Lumbar peritoneal shunting with video-laparoscopic assistance: A useful technique for the management of refractory postoperative lumbar CSF leaks. Surg Neurol. 2003. 59: 473-8 discussion 477-8
6. De Tommasi C, Bond AE. Complicated pseudomeningocele repair after chiari decompression: Case report and review of the literature. World Neurosurg. 2016. 88: 688.e1-7
7. Lee YM, Ordaz A, Durcanova B, Viner JA, Theodosopoulos PV, Aghi MK. Cerebrospinal fluid leaks and pseudomeningocele after posterior fossa surgery: Effect of an autospray dural sealant. Cureus. 2020. 12: e8379
8. Moza K, McMenomey SO, Delashaw JB. Indications for cerebrospinal fluid drainage and avoidance of complications. Otolaryngol Clin North Am. 2005. 38: 577-82
9. Sellin JN, Kolcun JP, Levi AD. Cerebrospinal fluid leak and symptomatic pseudomeningocele after intradural spine surgery. World Neurosurg. 2018. 120: e497-502
10. Slavnic D, Mccabe R, Tong D, Soo TM. Repair of postoperative cervical pseudomeningocele with the use of bone morphogenetic protein. Cureus. 2019. 11: e5200
11. Takai K, Taniguchi M. Targeted epidural blood patch under o-arm-guided stereotactic navigation in patients with intracranial hypotension associated with a spinal cerebrospinal fluid leak and ventral dural defect. World Neurosurg. 2017. 107: 351-7
12. West JL, De Biase G, Abode-Iyamah K, Nottmeier EW, Deen HG, Chen SG. Initial results of precision treatment of postoperative cerebrospinal fluid leak with ultrasound-guided epidural blood patch. World Neurosurg. 2021. 153: e204-12