- Department of Neurosurgery, Hospital da Restauracao, Av Agamenon Magalhaes, Recife, Pernambuco, Brazil.
DOI:10.25259/SNI_218_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fernando Henrique Souza, Silvya Nery Bernardino, Auricelio Batista Cezar Junior, Hugo André de Lima Martins, Isabel Nery Bernardino Souza, Regina Nery Bernardino Souza, Hildo Rocha Cirne Azevedo-Filho. Nerves transfers for functional hand recovery in traumatic lower brachial plexopathy. 29-Oct-2020;11:358
How to cite this URL: Fernando Henrique Souza, Silvya Nery Bernardino, Auricelio Batista Cezar Junior, Hugo André de Lima Martins, Isabel Nery Bernardino Souza, Regina Nery Bernardino Souza, Hildo Rocha Cirne Azevedo-Filho. Nerves transfers for functional hand recovery in traumatic lower brachial plexopathy. 29-Oct-2020;11:358. Available from: https://surgicalneurologyint.com/surgicalint-articles/10365/
Abstract
Background: Distal nerve transfers are an innovative modality for the treatment of C8-T1 brachial plexus lesions. The purpose of this case series is to report the authors’ results with hand restoration function by nerve transfer in patients with lower brachial plexus injury.
Methods: Three consecutive nerve transfers were performed in a series of 11 patients to restore hand function after injury to the lower brachial plexus: brachialis motor branch to anterior interosseous nerve (AIN) and supinator branch to the posterior interosseous nerve (PIN) in a first surgical procedure, and AIN to pronator quadratus branch of ulnar nerve between 4 and 6 months later.
Results: In all, 11 male patients underwent 33 surgical procedures. Time between brachial plexus injury and surgery was a mean of 11 months (range 4–13 months). Postoperative follow-up ranged from 12 to 24 months. We observed recovery of M3 or better finger flexion strength (AIN) and wrist extension (PIN) in 8 of the 11 surgically treated upper limbs. These patients recovered full thumb and finger extension between 6 and 12 months of surgery, without significant loss of donor function.
Conclusion: Nerve transfers represent a way of restoring volitional control of upper extremity function in patients with C8-T1 brachial plexus injury.
Keywords: Brachial plexus, Hand functional recovery, Musculocutaneous transfer, Nerve transfer, Peripheral nerve
INTRODUCTION
Lesions of the two lower brachial plexus roots (C8, T1) are a rare entity, known as DejerineKlumpke’s palsy. It accounts for <3% of the supraclavicular injuries of the brachial plexus.[
While the effects of these lesions are variable, shoulder and elbow functions are normal, and wrist extension and flexion are generally preserved due to the intact flexor carpi radialis and extensor carpi radialis longus. The flexors of the elbow are controlled by the musculocutaneous nerve formed mainly from C5 and C6 fibers, located above the level of the spinal lesion.[
The main mechanism of injury in the C8-T1 brachial plexus palsies is the traction of the abducted arm, leading to rupture of the lower roots. As a result, there is a motor and functional loss equivalent to paralysis of the ulnar nerve and the median nerve component derived from the medial cord. In these lesions, spontaneous recovery is an unlikely event, since motor and sensory deficits are far from the location of nerve lesions. Several methods were used to restore flexion and extension of the fingers. In recent years, attention has been focused on tendon transfer,[
This study was performed to report the authors’ results with hand function restoration in 11 patients with C8-T1 brachialis plexus injury through two simultaneous transfers: brachialis motor branch (BRMB) to anterior interosseous nerve (AIN), supinator branch to the posterior interosseous nerve (PIN); and a third subsequent transfer performed between 4 and 6 months after the first surgical procedure: AIN to deep motor branch of ulnar nerve.
MATERIALS AND METHODS
Clinical data
This prospective study was performed between September 2013 and July 2017. Three consecutive nerve transfers were performed in a series of 11 patients (male; mean age 35), to restore hand function after lower brachialis plexus injury, with a follow-up ranging from 12 to 24 months.
For this case series, research ethics approval was obtained from the local institutional review committee. The patients were informed regarding all surgical details and informed consent before participation was provided, in accordance with the Declaration of Helsinki. The functional clinical assessment of patients was based on the Medical Research Council (MRC) Scale for Muscle Strength.[
Electrophysiological testing or magnetic resonance imaging (MRI) was performed on all patients preoperatively. Electroneuromyography was performed 4 weeks after traumatic injury (due to Wallerian degeneration during this period). It could determine the distribution and extent of the injury, evaluate muscles that are difficult to test clinically, and quantify the extent of denervation. MRI showed indirect signs of traumatic injury to the brachialis plexus, such as pseudomeningoceles in T2-weighted images, spinal cord edema (an indirect sign of nerve root avulsion), and postganglionic lesions such as postinjury fibrosis, neuromas, and associated inflammation or edema. Preoperatively, the muscle strengths of the supinator and brachialis were at least graded M4, and electromyography revealed normal compound muscle action potential, confirming good functional status of the upper plexus. Pronator quadratus had no motor function (grade M0), through these same preoperative assessments.
Surgical technique
Transfer: Brachialis nerve to AIN
The procedure was usually performed under general anesthesia without neuromuscular blockade or tourniquet control (to avoid a temporary neurapraxia). For finger flexion restoration, the recipient nerve was the AIN in 11 limbs. The donor was the BRMB. This technique was originally described in 1997 by Wang and Zhu[
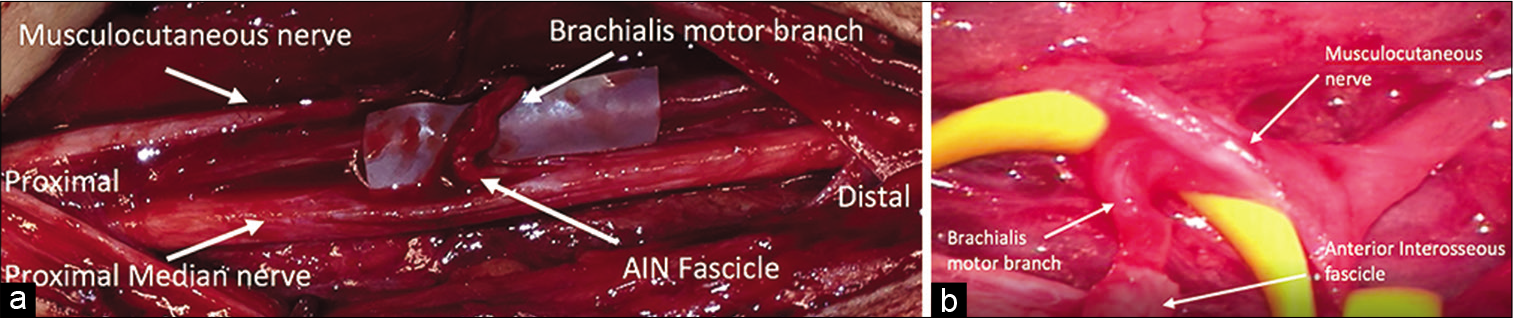
Once the musculocutaneous nerve and its branch to the brachialis muscle (donor) are identified, the latter is then sectioned distally and transferred to the recipient AIN fascicle, which was proximally transected [
Figure 1:
Figure 1: a: The donor brachialis motor branch (upper right white arrow) was transected distally and the anterior recipient interosseous nerve (AIN) fascicle (lower right white arrow) transected proximally to mobilize for an end-to-end nerve transfer, without significant retraction. b: Magnified view of terminal-to-terminal transfer from brachialis motor branch (lower left white arrow) to AIN (lower right white arrow).
The PT branch is not very recommended as a donor for reinnervation because pronation is essential for many daily living activities and because this muscle can be used for a tendon transfer in case the nerve transfer is unsuccessful.[
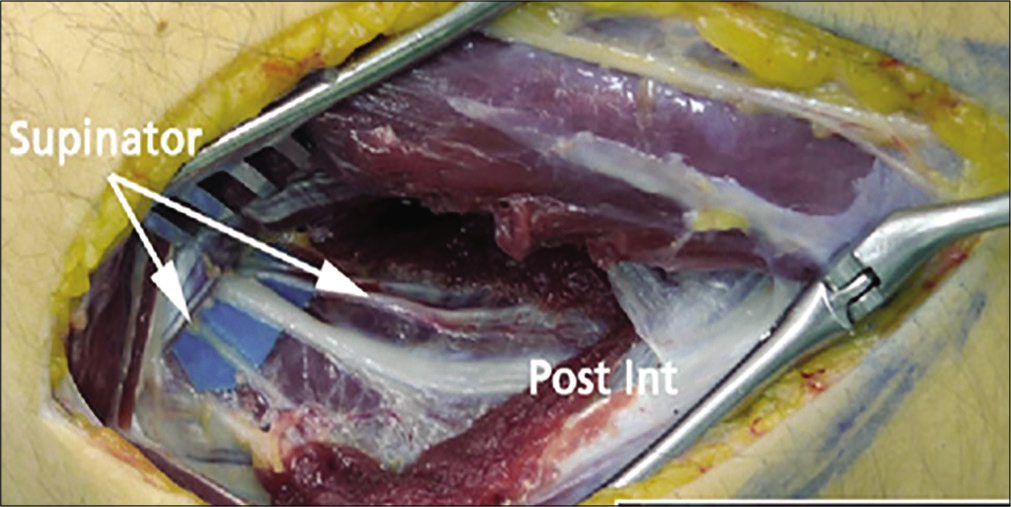
Transfer: Supinator motor branch to PIN
After the transfer of brachialis to the AIN, the rotation and pronation of the forearm is performed. A longitudinal incision was performed on the proximal third of the dorsal forearm. The supinator muscle (SM) was exposed after separation of the extensor carpi radialis brevis (ECRB) and extensor digitorum communis. After that, its motor branches originating from the PIN, proximal to the Frohse arcade, were identified.[
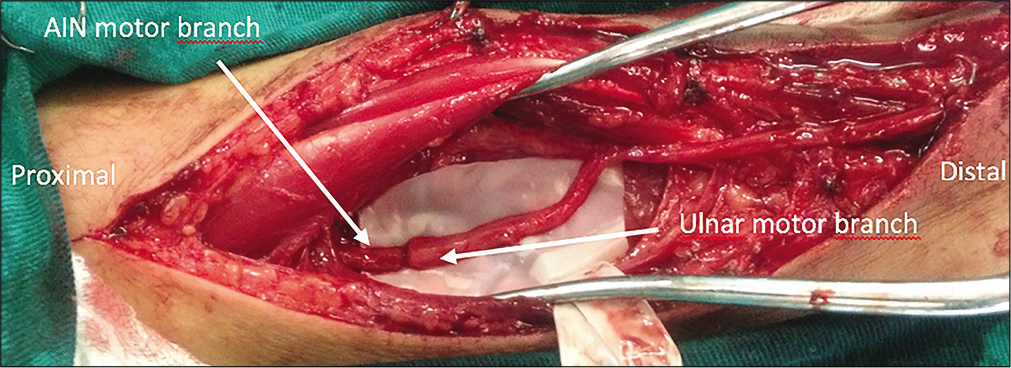
Transfer: AIN to ulnar
To try to recover the ulnar motor function, AIN to ulnar transfer was performed in a second surgical time, between 4 and 6 months later. The surgical technique proposed by Brown et al. was performed, associated with a Taleisnik incision[
RESULTS
In total, 33 operative procedures were performed on 11 male patients. Mean age at the time of surgery was 35.5 years (range 24–59 years). Time between brachial plexus injury and surgery was a mean of 11 months (range 4–13 months). Postoperative follow-up ranged from 12 to 24 months. All patients have a brachial plexus lesion involving the roots of C8 and T1.
Nerve transfer procedures were selected based on available donor nerves. Functional and electrodiagnostic evaluation was performed in the preoperative period. At a minimum, all patients required intact volitional elbow flexion and arm supination (MRC Grade ≥4) so that the brachialis and the supinator nerve branches could be utilized as a donor nerve.
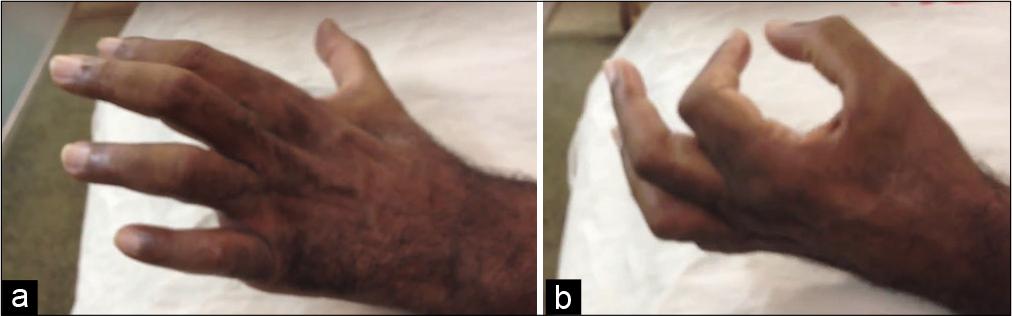
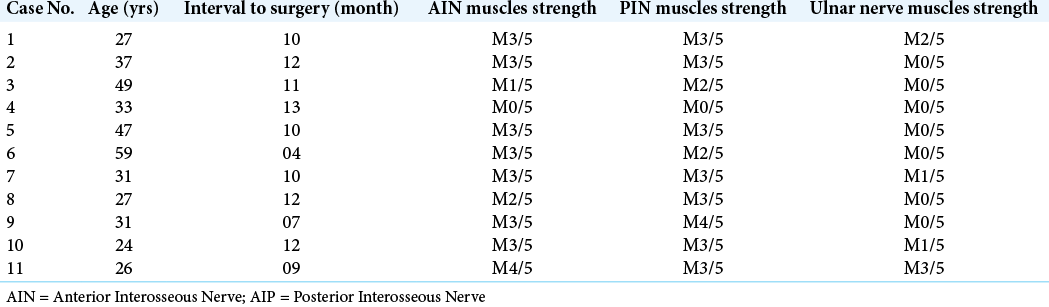
We observed recovery of M3 or better finger flexion strength in muscles innervated by AIN (flexor digitorum profundus and flexor pollicis longus) and in wrist extension supplied by PIN (ECRB and extensor carpi ulnaris) in 8 of the 11 surgically treated upper limbs [
DISCUSSION
Nerve transfers to restore hands and the arm functions are a challenge in the surgical treatment of low brachial plexus lesions. The restoration of the manual functions is fundamental for the independence and improvement of the quality of life of the affected individuals. Several different nerve transfers have been attempted for this purpose.
Supinator motor branch transfer to the PIN[
Forearm supination is produced by two major muscles: the biceps brachii and supinator, which are both functioning muscles in C8–T1 palsies. Therefore, some authors have suggested that brachialis innervation is not critical for elbow flexion, due to its redundant function.[
Proximal dissection of the AIN was associated with better outcomes, presumably because section of nerve fiber interconnections during dissection resulted in a more direct axonal regrowth, thus decreasing axonal dispersion. Motor fibers dispersion within the median nerve might be responsible for spontaneous recovery and improved results after nerve transfer, using the nerve to the brachialis as the donor nerve and the AIN as the recipient. The supinator nerve branch to PIN transfer gives great hand and first web space opening. Differential thumb and finger extension are possible, and reanimation of extensor carpi ulnaris centralizes an otherwise radially deviated wrist.
BRMB to AIN transfer showed satisfactory results in the clinical application, as published by some authors. Gu et al.[
Dong et al.[
Our results of AIN transfer to the ulnar nerve were modest. We observed an unsatisfactory functional recovery during the 12–24 months of follow-up; we obtained M3 ulnar nerve function in only one case. Consistent with our results, Brown et al.[
It is known that incorporating the distal AIN to ulnar motor transfer into the treatment plan for lower brachial plexus injuries is functionally ineffective. In this case, transfer of residual axons to the pronator quadratus is insufficient to provide a motor response of the ulnar nerve, in lesions of the lower brachial plexus (C8-T1). Therefore, this article proposed a sequence of surgical techniques aimed at a functional recovery of the hand in C8 and T1 avulsion. An advantage of the nerve transfer set described in our series is the opportunity for recovery of a group of extensors that may become potential donor sources for tendon transfer in reconstructions of intrinsic functions of the hand.
One bias of our results was the long interval between the traumatic event and the surgical intervention, due to the limitations related to the public health system related to the assessed sample. The timing of surgery is a key point when considering nerve transfers. In fact, the chance of a functional recovery falls progressively after 6 months–2 years.[
CONCLUSION
The brachialis-to-AIN and supinator branch to the PIN transfer technique offers the potential for restoration of intrinsic hand function in patients with C8-T1 brachial plexus injury. The application of a multidisciplinary team approach in addition to peripheral nerve service may improve the outcomes and the functional recovery of these patients.[
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (name of institute/committee) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alizo G, Sciarretta JD, Gibson S, Muertos K, Holmes S, Denittis F. Multidisciplinary team approach to traumatic spinal cord injuries: A single institution’s quality improvement project. Eur J Trauma Emerg Surg. 2018. 44: 245-50
2. Bertelli JA, Ghizoni MF, Tacca CP. Transfer of the teres minor motor branch for triceps reinnervation in tetraplegia. J Neurosurg. 2011. 114: 1457-60
3. Bertelli JA, Ghizoni MF. Brachialis muscle transfer to reconstruct finger flexion or wrist extension in brachial plexus palsy. J Hand Surg Am. 2006. 31: 190-6
4. Bertelli JA, Ghizoni MF. Nerve transfers for restoration of finger flexion in patients with tetraplegia. J Neurosurg Spine. 2017. 26: 55-61
5. Bertelli JA, Ghizoni MF. Transfer of supinator motor branches to the posterior interosseous nerve in C7-T1 brachial plexus palsy. J Neurosurg. 2010. 113: 129-32
6. Bertelli JA, Kechele PR, Santos MA, Besen BA, Duarte H. Anatomical feasibility of transferring supinator motor branches to the posterior interosseous nerve in C7-T1 brachial plexus palsies. J Neurosurg. 2009. 111: 326-31
7. Bertelli JA, Tacca CP, Ghizoni MF, Kechele PR, Santos MA. Transfer of supinator motor branches to the posterior interosseous nerve to reconstruct thumb and finger extension in tetraplegia: Case report. J Hand Surg Am. 2010. 35: 1647-51
8. Brown JM, Yee A, Mackinnon SE. Distal median to ulnar nerve transfers to restore ulnar motor and sensory function within the hand. Neurosurgery. 2009. 65: 966-78
9. Carlsen BT, Kircher MF, Spinner RJ, Bishop AT, Shin AY. Comparison of single versus double nerve transfers for elbow flexion after brachial plexus injury. Plast Reconstr Surg. 2011. 127: 269-76
10. Davidge KM, Yee A, Kahn LC, Mackinnon SE. Median to radial nerve transfers for restoration of wrist, finger, and thumb extension. J Hand Surg Am. 2013. 38: 1812-27
11. Doi K, Hattori Y, Kuwata N, Soo-heong T, Kawakami F, Otsuka K. Free muscle transfer can restore hand function after injuries of the lower brachial plexus. J Bone Joint Surg Br. 1998. 80: 117-20
12. Dong Z, Gu YD, Zhang CG, Zhang L. Clinical use of supinator motor branch transfer to the posterior interosseous nerve in C7-T1 brachial plexus palsies. J Neurosurg. 2010. 113: 113-7
13. Fox IK, Novak CB, Kahn LC, Mackinnon SE, Ruvinskaya R, Juknis N. Using nerve transfer to restore prehension and grasp 12 years following spinal cord injury: A case report. Spinal Cord Ser Cases. 2018. 4: 37
14. Fu SY, Gordon T. Contributing factors to poor functional recovery after delayed nerve repair: Prolonged axotomy. J Neurosci. 1995. 15: 3876-85
15. Fu SY, Gordon T. Contributing factors to poor functional recovery after delayed nerve repair: Prolonged denervation. J Neurosci. 1995. 15: 3886-95
16. García-López A, Fernández E, Martínez F. Transfer of brachioradialis motor branch to the anterior interosseous nerve in C8-T1 brachial plexus palsy. An anatomic study. Microsurgery. 2013. 33: 297-300
17. García-López A, Sebastian P, Martinez F, Perea D. Transfer of the nerve to the brachioradialis muscle to the anterior interosseous nerve for treatment for lower brachial plexus lesions: Case Report. J Hand Surg Am. 2011. 36: 394-7
18. Goubier JN, Teboul F. Management of hand palsies in isolated C7 to T1 or C8, T1 root avulsions. Tech Hand Up Extrem Surg. 2008. 12: 156-60
19. Gu Y, Wang H, Zhang L, Zhang G, Zhao X, Chen L. Transfer of brachialis branch of musculocutaneous nerve for finger flexion: Anatomic study and case report. Microsurgery. 2004. 24: 358-62
20. Hawasli AH, Chang J, Reynolds MR, Ray WZ. Transfer of the brachialis to the anterior interosseous nerve as a treatment strategy for cervical spinal cord injury: Technical note. Global Spine J. 2015. 5: 110-7
21. Kobayashi J, Mackinnon SE, Watanabe O, Ball DJ, Gu XM, Hunter DA. The effect of duration of muscle denervation on functional recovery in the rat model. Muscle Nerve. 1997. 20: 858-66
22. Krasuski M, Kiwerski J. An analysis of the results of transferring the musculocutaneous nerve onto the median nerve in tetraplegics. Arch Orthop Trauma Surg. 1991. 111: 32-3
23. Mackinnon SE, Novak CB. Nerve transfers. New options for reconstruction following nerve injury. Hand Clin. 1999. 15: 643-66
24. Mackinnon SE, Yee A, Ray WZ. Nerve transfers for the restoration of hand function after spinal cord injury. J Neurosurg. 2012. 117: 176-85
25. .editors. Aids to the Examination of the Peripheral Nervous System, Memorandum No 45. London: Medical Research Council; 1976. p.
26. Midha R. Epidemiology of brachial plexus injuries in a multitrauma population. Neurosurgery. 1997. 40: 1182-9
27. Ray WZ, Yarbrough CK, Yee A, Mackinnon SE. Clinical outcomes following brachialis to anterior interosseous nerve transfers. J Neurosurg. 2012. 117: 604-9
28. Senjaya F, Midha R. Nerve transfer strategies for spinal cord injury. World Neurosurg. 2013. 80: e319-26
29. Standring S.editors. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. Amsterdam: Elsevier; 2008. p.
30. Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ.editors. Nerves and Nerve Injuries. United States: Academic Press; 2015. p.
31. Vanaclocha-Vanaclocha V, Ortiz-Criado JM, Sáiz-Sapena N, Vanaclocha N.editors. Nerve Transfers in the Treatment of Peripheral Nerve Injuries, in Peripheral Nerve Regeneration-From Surgery to New Therapeutic Approaches Including Biomaterials and Cell-Based Therapies Development. London: InTech; 2017. p.
32. Wang Y, Zhu S. Transfer of a branch of the anterior interosseous nerve to the motor branch of the median nerve and ulnar nerve. Chin Med J (Engl). 1997. 110: 216-9
33. Waters RL, Sie IH, Gellman H, Tognella M. Functional hand surgery following tetraplegia. Arch Phys Med Rehabil. 1996. 77: 86-94
34. Xu B, Dong Z, Zhang CG, Gu YD. Multiple nerve and tendon transfers: A new strategy for restoring hand function in a patient with C7-T1 brachial plexus avulsions. J Neurosurg. 2017. 127: 837-42
35. Yang J, Jia X, Yu C, Gu YD. Pronator teres branch transfer to the anterior interosseous nerve for treating C8T1 brachial plexus avulsion: An anatomic study and case report. Neurosurgery. 2014. 75: 375-9
36. Young D, Papp S, Giachino A. Physical examination of the wrist. Hand Clin. 2010. 26: 21-36
37. Zhao X, Lao J, Hung LK, Zhang GM, Zhang LY, Gu YD. Selective neurotization of the median nerve in the arm to treat brachial plexus palsy, Surgical technique. J Bone Joint Surg Am. 2005. 87: 122-35
38. Zhao X, Lao J, Hung LK, Zhang GM, Zhang LY, Gu YD. Selective neurotization of the median nerve in the arm to treat brachial plexus palsy: An anatomic study and case report. J Bone Joint Surg Ser A. 2004. 86: 736-42
39. Zheng XY, Hou CL, Gu YD, Shi QL, Guan SB. Repair of brachial plexus lower trunk injury by transferring brachialis muscle branch of musculocutaneous nerve: Anatomic feasibility and clinical trials. Chin Med J (Engl). 2008. 121: 99-104