- Department of Biomedical Sciences, Boise State University, Boise, United States.
Correspondence Address:
Mohammed A Azab, Department of Biomedical Sciences, Boise State University, Boise, United States.
DOI:10.25259/SNI_367_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammed A Azab. Neurosurgical intervention in an unusual case of extensive acute disseminated encephalomyelitis – A case report and literature review. 19-May-2023;14:176
How to cite this URL: Mohammed A Azab. Neurosurgical intervention in an unusual case of extensive acute disseminated encephalomyelitis – A case report and literature review. 19-May-2023;14:176. Available from: https://surgicalneurologyint.com/surgicalint-articles/12329/
Abstract
Background: The clinical presentations of demyelinating diseases are variable and can range from mild symptoms to fulminant presentations. Acute disseminated encephalomyelitis is one of those diseases which usually follow an infection or vaccination.
Case Description: We report a case of extensive acute demyelinating encephalomyelitis (ADEM) with massive brain swelling. A 45-year-old female presented to the emergency room with status epilepticus. Patient has no history of any associated medical problems. Glasgow coma scale (GCS) was 15/15. CT brain was normal. Lumbar puncture was done and cerebrospinal fluid showed pleocytosis and increased protein content. About 2 days after admission, the conscious level rapidly deteriorated and GCS was 3/15, with the right pupil fully dilated and unreactive to light. Computed tomography and magnetic resonance imaging brain were done. We performed an urgent decompressive craniectomy as a life-saving procedure. Histopathological examination was suggestive of ADEM.
Conclusion: Few cases of ADEM with brain swelling were reported, but there is no solid consensus about the appropriate management of these cases. Decompressive hemicraniectomy is a possible choice, but further research is needed to evaluate the proper timing, and indication of surgery.
Keywords: Acute demyelinating encephalomyelitis (ADEM), Brain edema, Decompressive craniectomy, Demyelinating, Herniation
INTRODUCTION
Primary demyelinating diseases include multiple sclerosis and less frequently encountered diseases as acute demyelinating encephalomyelitis (ADEM), neuromyelitis optica, tumefactive demyelinating disease, Marburg’s disease, Balo’s disease, and Schilder’s disease. ADEM is an inflammatory demyelination process of the central nervous system that usually occurs after a viral or bacterial infection or vaccination. The presentation varies from mild neurological deficit to severe fulminant disease.[
The acute deterioration could be caused by seizures, disturbed conscious level, and brain herniation. In rare occasions, ADEM can cause severe life-threatening brain edema and increased intracranial pressure (ICP).[
Herein, we describe a case of fulminant ADEM, where the rapid development of severe cerebral edema and brain herniation was treated with decompressive hemicraniectomy and temporal polectomy. We tried to report similar cases in the literature to determine the optimal management in those cases and to highlight the heterogeneity of clinical presentations and outcome.
CASE DESCRIPTION
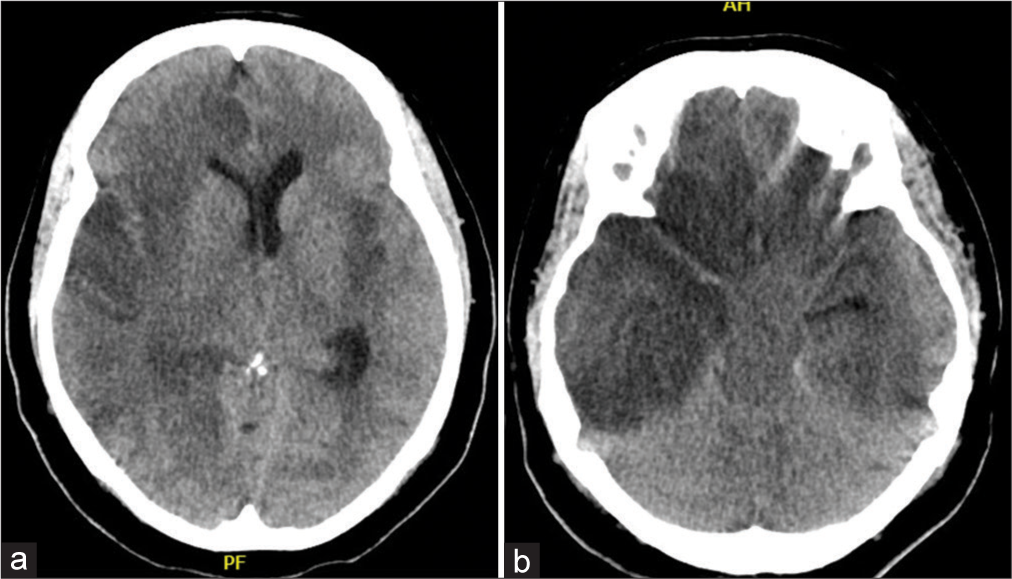
A 45-year-old female presented to the emergency room with status epilepticus. The patient has no relevant history for any associated medical problems. Initial resuscitation was done and midazolam and loading phenytoin was given to the patient. The patient improved and glasgow coma scale (GCS) was 15/15. CT brain was normal. The patient was admitted to the intensive care unit (ICU) for further examination. By history reviewing, she had a fever 4 days before admission. Electroencephalogram (EEG) was done and revealed generalized slowing of electric activity. Lumbar puncture was done and cerebrospinal fluid (CSF) was sent for analysis which showed pleocytosis and increased protein content. About 2 days after admission, the conscious level rapidly deteriorated and GCS was 3/15, with the right pupil fully dilated and unreactive to light. CT brain is shown in
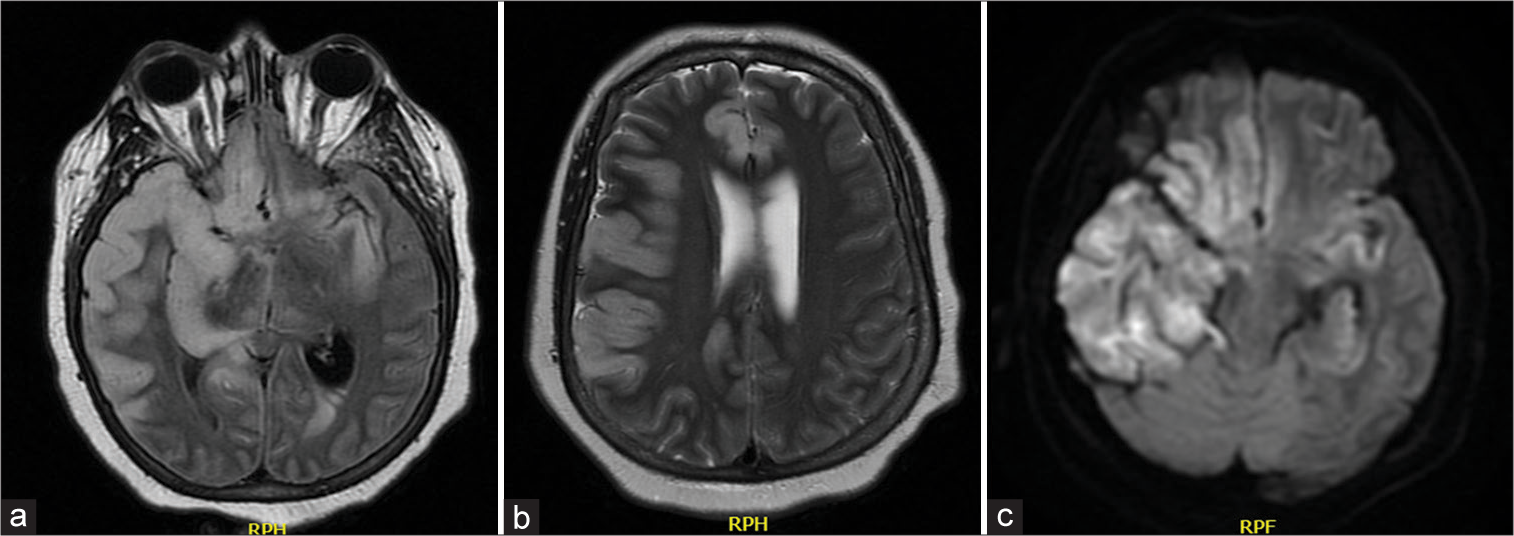
Figure 2:
(a-c) Magnetic resonance imaging (MRI) fluid-attenuated inversion recovery, T2MRI, diffusion-weighted imaging MRI, brain showing diffuse scattered patchy hyperintensities affecting mainly the right temporal and parietal lobes, and left hippocampus. RPH: Relative peak height, RPF: Relative peak flow.
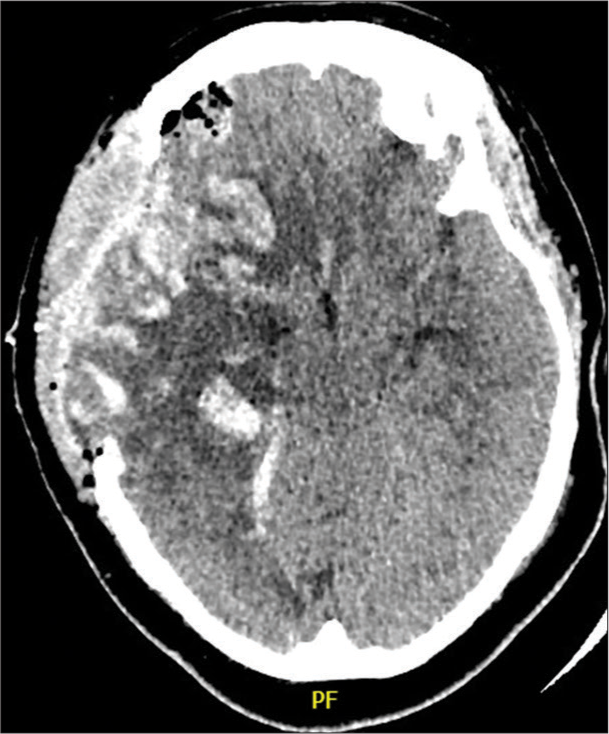
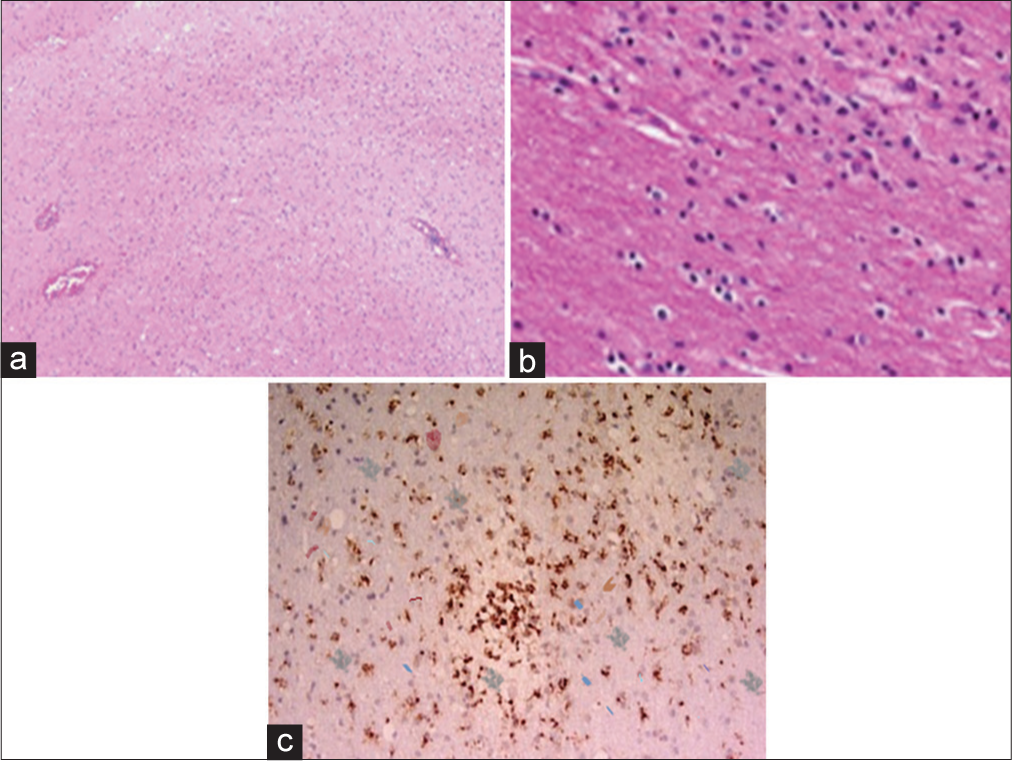
Brain dehydrating measures were started. The patient was given IV mannitol, IV dexamethasone, and deep sedation which were applied. IV acyclovir was given empirically. The patient did not improve and the condition remained the same. Urgent decompressive craniectomy was done. Intraoperatively, the brain was markedly swollen, so we performed frontal and temporal polectomy. Postoperatively, the patient’s conscious level did not improve. The patient is still in the ICU. Histological features are characteristic of ADEM, as shown in
DISCUSSION
ADEM is an inflammatory demyelinating disease that is relatively rare in adults.[
Diagnosis of ADEM is largely dependent on clinical presentation and imaging. Earlier in the disease, CT may be normal, or it may show multifocal white matter changes in clinically advanced cases.[
High dose of intravenous steroids, intravenous immunoglobulin, and plasmapheresis is the main treatment lines in the acute stage.[
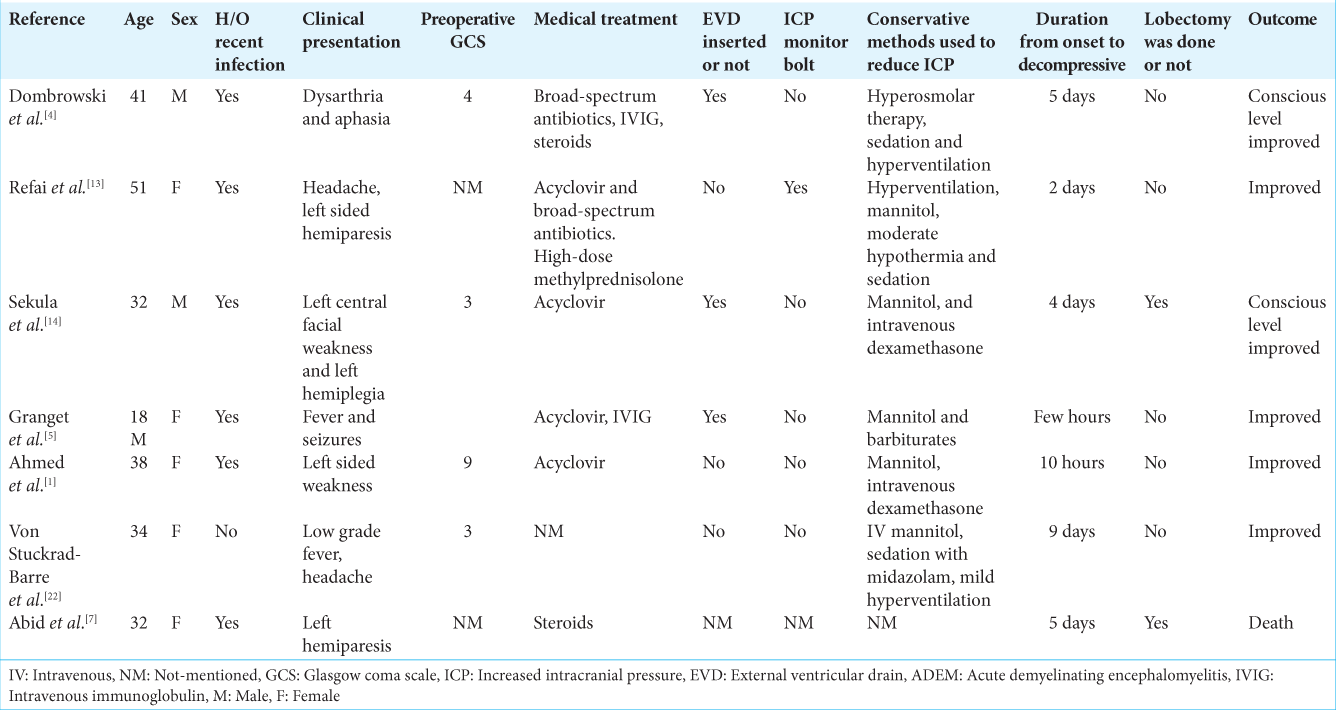
In cases of persistent ICP elevation, decompressive craniectomy is the last option. This can reduce the intracranial pressure, but the effect on the outcome is still undefined. There are no solid criteria for the exact timing and patient selection for decompressive craniectomy for ADEM. The use of decompressive hemicraniectomy has been well described in cases of herpes simplex encephalitis.[
In this case, we tried to reduce the ICP with conservative measures, but the patient’s condition did not improve. Therefore, decompressive hemicraniectomy with frontal and temporal polectomy was done. The patient’s condition did not improve postoperatively. Hossem et al. treated a case of ADEM with decompressive hemicraniectomy, and lobectomy and the patient died.[
CONCLUSION
The reported literature describing the role of decompressive craniectomy in the management of severe cases of ADEM is still lacking. Few cases of ADEM with brain swelling were reported, but there is no solid consensus about the appropriate management. Decompressive hemicraniectomy is a possible choice, but further research is needed to evaluate the proper timing and indication of surgery.
Ethical approval
Consent was obtained by the patient in this study. The Hospital Research Board approved the Institutional Review Board (IRB) for this work.
Author Contributions
Dr. Mohammed A Azab has contributed to designing the idea, drafting, manuscript writing, and the final review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmed AI, Eynon CA, Kinton L, Nicoll JA, Belli A. Decompressive craniectomy for acute disseminated encephalomyelitis. Neurocrit Care. 2010. 13: 393-5
2. Alexander M, Murthy JM. Acute disseminated encephalomyelitis: Treatment guidelines. Ann Indian Acad Neurol. 2011. 14: S60-4
3. Byun YH, Ha EJ, Ko SB, Kim KH. Decompressive craniectomy for herpes simplex encephalitis complicated by frank intracerebral hemorrhage: A case report and review of the literature. BMC Neurol. 2018. 18: 176
4. Dombrowski KE, Mehta AI, Turner DA, McDonagh DL. Life-saving hemicraniectomy for fulminant acute disseminated encephalomyelitis. Br J Neurosurg. 2011. 25: 249-52
5. Granget E, Milh M, Pech-Gourg G, Paut O, Girard N, Lena G. Life-saving decompressive craniectomy for acute disseminated encephalomyelitis in a child: A case report. Childs Nerv Syst. 2012. 28: 1121-4
6. Höllinger P, Sturzenegger M, Mathis J, Schroth G, Hess CW. Acute disseminated encephalomyelitis in adults: A reappraisal of clinical, CSF, EEG, and MRI findings. J Neurol. 2002. 249: 320-9
7. Houssem A, Jean-Etienne H, Marco M, Jerome S, Leonardo T, Salvatore C. Unusual and dramatic presentation of “Adem”: What could be done in neurosurgical practice?. J Neurol Stroke. 2015. 2: 45-9
8. Kinoshita A, Kaseda S, Yagi K, Oda M, Tanabe H. A case of acute disseminated encephalomyelitis with pathologically-proven acute demyelinating lesion in the peripheral nervous system. Rinsho Shinkeigaku. 1994. 34: 892-7
9. Locatelli C, Ciambra R, Pasini M, Suprani T, Cataldi ML, Pocecco M. Acute disseminated encephalomyelitis (ADEM): Report of a clinical case. Pediatr Med Chir. 2005. 27: 109-14
10. Lukes SA, Norman D. Computed tomography in acute disseminated encephalomyelitis. Ann Neurol. 1983. 13: 567-72
11. Menge T, Hemmer B, Nessler S, Wiendl H, Neuhaus O, Hartung HP. Acute disseminated encephalomyelitis: An update. Arch Neurol. 2005. 62: 1673-80
12. Pavone P, Pettoello-Mantovano M, Le Pira A, Giardino I, Pulvirenti A, Giugno R. Acute disseminated encephalomyelitis: A long-term prospective study and meta-analysis. Neuropediatrics. 2010. 41: 246-55
13. Refai D, Lee MC, Goldenberg FD, Frank JI. Decompressive hemicraniectomy for acute disseminated encephalomyelitis: Case report. Neurosurgery. 2005. 56: E872
14. Sekula RF, Marchan EM, Baghai P, Jannetta PJ, Quigley MR. Central brain herniation secondary to fulminant acute disseminated encephalomyelitis: Implications for neurosurgical management. Case report. J Neurosurg. 2006. 105: 472-4
15. Schwarz S, Mohr A, Knauth M, Wildemann B, StorchHagenlocher B. Acute disseminated encephalomyelitis: A follow-up study of 40 adult patients. Neurology. 2001. 56: 1313-8
16. Singh S, Alexander M, Korah IP. Acute disseminated encephalomyelitis: MR imaging features. AJR Am J Roentgenol. 1999. 173: 1101-7
17. Singhi P, Saini AG, Sahu JK, Kumar N, Vyas S, Vasishta RK. Unusual clinical presentation and role of decompressive craniectomy in herpes simplex encephalitis. J Child Neurol. 2015. 30: 1204-7
18. Stüve O, Nessler S, Hartung HP, Hemmer B, Wiendl H, Kieseier BC. Acute disseminated encephalomyelitis. Pathogenesis, diagnosis, treatment, and prognosis. Nervenarzt. 2005. 76: 701-7
19. Takata T, Hirakawa M, Sakurai M, Kanazawa I. Fulminant form of acute disseminated encephalomyelitis: Successful treatment with hypothermia. J Neurol Sci. 1999. 165: 94-7
20. Todeschi J, Gubian A, Wirth T, Coca HA, Proust F, Cebula H. Multimodal management of severe herpes simplex virus encephalitis: A case report and literature review. Neurochirurgie. 2018. 64: 183-9
21. Van Der Knaap MS, Valk J, editors. Acute disseminated encephalomyelitis and acute hermorrhagic encephalomyelitis. Magnetic Resonance of Myelin. Myelination and Myelin Disorders. Heidelberg: Springer-Verlag; 1995. p. 320-6
22. Von Stuckrad-Barre S, Klippel E, Foerch C, Lang JM, du Mesnil de Rochemont R, Sitzer M. Hemicraniectomy as a successful treatment of mass effect in acute disseminated encephalomyelitis. Neurology. 2003. 61: 420-1