- Department of Neurosurgery, Tokyo Women's Medical University Medical Center East, Tokyo, Japan
Correspondence Address:
Shigeru Tani
Department of Neurosurgery, Tokyo Women's Medical University Medical Center East, Tokyo, Japan
DOI:10.4103/sni.sni_370_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shigeru Tani, Mayuko Inazuka, Tatsuya Maegawa, Yuichi Takahashi, Asami Kikuchi, Suguru Yokosako, Chika Yoshimura, Hirokazu Koseki, Hidenori Ohbuchi, Kengo Hirota, Shinji Hagiwara, Motohiro Hirasawa, Atsushi Sasahara, Hidetoshi Kasuya. Nonspastic hemifacial spasm confirmed by abnormal muscle responses. 05-Jun-2017;8:96
How to cite this URL: Shigeru Tani, Mayuko Inazuka, Tatsuya Maegawa, Yuichi Takahashi, Asami Kikuchi, Suguru Yokosako, Chika Yoshimura, Hirokazu Koseki, Hidenori Ohbuchi, Kengo Hirota, Shinji Hagiwara, Motohiro Hirasawa, Atsushi Sasahara, Hidetoshi Kasuya. Nonspastic hemifacial spasm confirmed by abnormal muscle responses. 05-Jun-2017;8:96. Available from: http://surgicalneurologyint.com/surgicalint-articles/nonspastic-hemifacial-spasm-confirmed-by-abnormal-muscle-responses/
Abstract
Background:Hemifacial spasm is usually diagnosed by inspection which mainly identifies involuntary movements of orbicularis oculi. Assessing abnormal muscle responses (AMR) is another diagnostic method.
Case Description:We report a case of left hemifacial spasm without detectable involuntary facial movements. The patient was a 48-year-old man with a long history of subjective left facial twitching. On magnetic resonance imaging (MRI), the left VIIth cranial nerve was compressed by the left anterior inferior cerebellar artery (AICA), which was in turn compressed by the left vertebral artery. We initially treated him with botulinum toxin. We were able to record AMR, and hemifacial spasm occurred after AMR stimulation, although no spasm was detectable by inspection. Subsequently, we performed microvascular decompression with transposition of the AICA that compressed the VIIth cranial nerve. His hemifacial spasm resolved by 5 weeks after surgery and was not induced by AMR stimulation.
Conclusion:Hemifacial spasm can sometimes be diagnosed by detecting AMR rather than by visual inspection. We propose that such hemifacial spasm should be termed nonspastic hemifacial spasm.
Keywords: Abnormal muscle response, hemifacial spasm, nonspastic hemifacial spasm
INTRODUCTION
Hemifacial spasm (HFS) is defined as involuntary, irregular, clonic or tonic contraction of muscles innervated by the VIIth cranial nerve. It usually commences as twitching of the lower eyelid, followed by involvement of other periorbital, facial, and perioral muscles, as well as platysma, often leading to social embarrassment and/or interference with vision due to involuntary eye movements.[
CASE REPORT
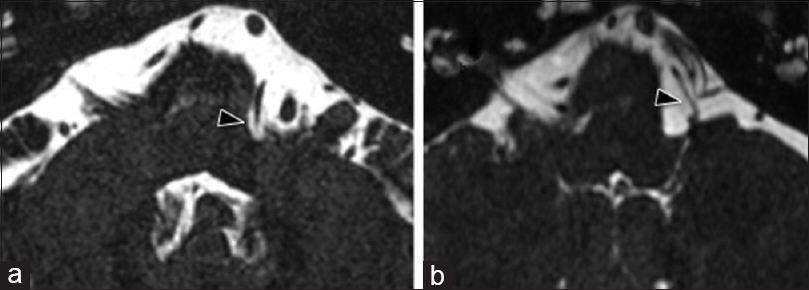
A 48-year-old man complained of a twitching feeling on the left side of the face for more than 3 years. He had been treated with botulinum toxin (BTX), although there were no clear symptoms of HFS. He was then referred to our outpatient clinic for diagnosis and further treatment. He complained of twitching that mainly affected the infraorbital region of the left face, however, HFS was not apparent by inspection. Magnetic resonance imaging (MRI) with fast imaging employing steady-state acquisition (FIESTA) showed that the left anterior inferior cerebellar artery (AICA) compressed the root exit zone (REZ) of the left VIIth nerve [
Figure 2
Abnormal muscle responses (AMR) were recorded from the orbicularis oculi muscle (upper) and mentalis muscle (lower) at the outpatient clinic (a) and during surgery (b) with 6.5 mA stimulation. AMR disappeared completely after microvascular decompression (c). AMR are not M-responses at 2.9 ms but F-responses at 10–15 ms after stimulation of the nerve to the ipsilateral frontalis muscle
The patient eventually agreed to surgical treatment due to severe discomfort. Microvascular decompression (MVD) was performed via left retrosigmoid lateral suboccipital craniotomy with intraoperative monitoring of AMR. Electromyograms (EMG) were recorded directly from the muscles with needle electrodes under intravenous general anesthesia using propofol and fentanyl. The AMR detected at 20 ms [
DISCUSSION
HFS is defined as involuntary, irregular, clonic or tonic contraction of muscles innervated by the VIIth cranial nerve. Symptoms usually start with twitching of the lower eyelid, which is followed by involvement of other periorbital, facial, perioral, and cervical muscles, often leading to social embarrassment, and interference with vision by involuntary eye movements.[
Two hypotheses for the electrophysiological mechanism of facial spasm have been proposed: (1) compression of the facial nerve by a blood vessel injures the myelin sheath and facilitates ephaptic transmission between nerve fibers to increase spontaneous activity; or (2) spasm is induced by hyperexcitability of the facial motor nucleus itself.[
We propose two possible mechanisms as the cause of atypical HFS. The facial muscles may receive very weak stimulation by current leaking from nerve fibers with demyelination. If nerve fibers undergo demyelination, the action potential is reduced because the intermodal density of sodium channels is too low for action potential propagation in demyelinated axons.[
When we encounter a patient who complains of facial twitching but cannot detect typical HFS by visual inspection, we should remember that the present case might be rare, but such cases can occur. Even if HFS cannot be detected, if MRI apparently shows vascular compression of the facial nerve, we need to check whether AMR and HFS are induced by stimulation. If AMR and HFS are induced, the patient should be treated with BTX or should have surgery if the symptoms are severe enough to be problematic for daily life.
CONCLUSION
In conclusion, we reported a patient who had with HFS without obvious involuntary facial movements. The diagnosis was based on electrophysiological studies and MRI, and symptoms were cured by MVD. We propose that such atypical HFS should be known as “nonspastic hemifacial spasm.”
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Burke D, Kiernan MC, Bostock H. Excitability of human axons. Clin Neurophysiol. 2001. 112: 1575-85
2. Cattaneo L, Giovanni P. The facial motor system. Neurosci Biobehav Rev. 2014. 38: 135-59
3. Fukuda M, Oishi M, Takao T, Hiraishi T, Sato Y, Fujii Y. Monitoring of abnormal muscle response and facial motor evoked potential during microvascular decompression for hemifacial spasm. Surg Neurol Int. 2012. 3: 118-
4. Ishikawa M, Ohira T, Namiki J, Kobayashi M, Takase M, Kawase T. Electrophysiological investigation of hemifacial spasm after microvascular decompression: F waves of the facial nucleus, blink reflexes, and abnormal muscle responses. J Neurosurg. 1997. 86: 654-61
5. Nielsen VK. Pathophysiology of hemifacial spasm: I. Ephaptic transmission and ectopic excitation. Neurology. 1984. 34: 418-26
6. Nielsen VK. Electrophysiology of the facial nerve in hemifacial spasm. Ectopic/ephaptic excitation. Muscle Nerve. 1985. 8: 545-55
7. Wang A, Jankovic J. Hemifacial spasm: Clinical findings and treatment. Muscle Nerve. 1998. 21: 1740-7