- Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma, United States.
Correspondence Address:
Ian F. Dunn, Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma, United States.
DOI:10.25259/SNI_26_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Arpan R. Chakraborty, Panayiotis E. Pelargos, Camille K. Milton, Michael D. Martin, Andrew M. Bauer, Ian F. Dunn. Occipital condyle screw fixation after posterior decompression for Chiari malformation: Technical report and application. 02-Nov-2021;12:543
How to cite this URL: Arpan R. Chakraborty, Panayiotis E. Pelargos, Camille K. Milton, Michael D. Martin, Andrew M. Bauer, Ian F. Dunn. Occipital condyle screw fixation after posterior decompression for Chiari malformation: Technical report and application. 02-Nov-2021;12:543. Available from: https://surgicalneurologyint.com/surgicalint-articles/11215/
Abstract
Background: Surgical techniques for stabilization of the occipital cervical junction have traditionally consisted of screw-based techniques applied in conjunction with occipital plating and rods connected to subaxial instrumentation in the form of pars, pedicle, or lateral mass screws. In patients with type 1 Chiari malformation (CM-1) and evidence of occipital cervical junction instability who have undergone posterior decompression, the occipital condyle (OC) represents a potential alternative cranial fixation point. To date, this technique has only been described in pediatric case reports and morphometric cadaver studies.
Methods: Patients underwent posterior fossa decompression for treatment of CM. Subsequently, patients received occipital cervical stabilization using OC screws.
Results: Patients were successfully treated with no post-operative morbidity. Patient 2 was found to have pseudoarthrosis and underwent revision. Both patients continue to do well at 1-year follow-up.
Conclusion: Placement of the OC screw offers advantages over traditional plate-based occipital fixation in that bone removal for suboccipital decompression is not compromised by the need for hardware placement, screws are hidden underneath ample soft tissue in patients with thin skin which prevents erosion, and the OC consists of primarily cortical bone which provides for robust tricortical fixation. These cases demonstrate the novel application of the OC screw fixation technique to the treatment of occipital cervical junction instability in adult patients undergoing simultaneous posterior fossa decompression.
Keywords: Chiari malformation, Occipital condyle screw, Posterior decompression
INTRODUCTION
The occipitocervical junction (OCJ) is a complex anatomical site that poses an operative challenge due to multiple axes of movement and limited available bone surface for fusion. The OCJ consists of the occiput, the atlas, and the axis. Instability of the OCJ may lead to permanent neurological deficits, devastating injury, or death.[
Surgical fixation of pathologies of the OCJ has evolved over time. Methods of fixation include plates and screws, rods and screws, and wire-based techniques.[
In the present report, we describe two patients who underwent successful posterior fossa decompression followed in the same operation by OC screw placement for evidence of craniocervical instability. To the best of our knowledge, these are the first documented cases of adults with CM-1 and craniocervical instability who received such treatment.
MATERIALS AND METHODS
Surgical technique
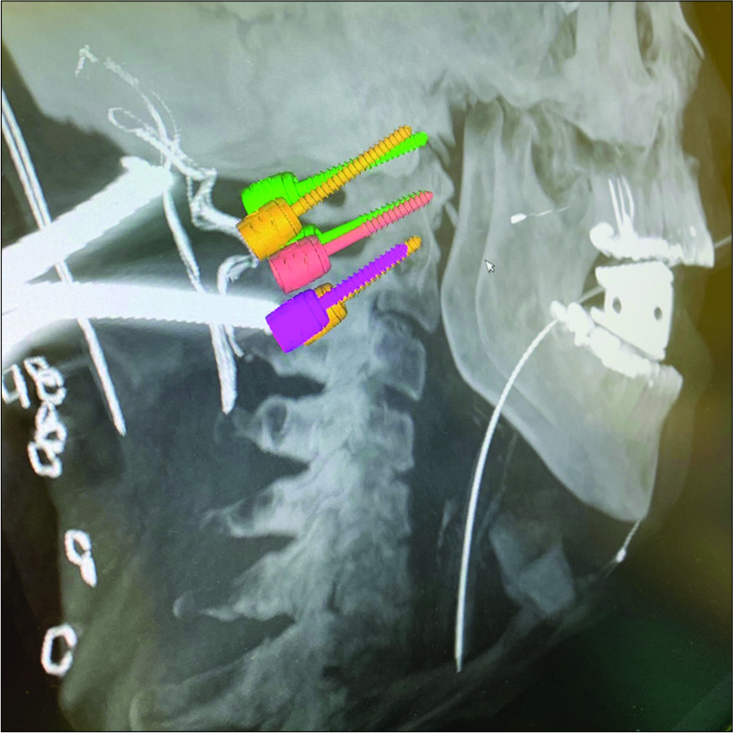
Informed consent was obtained from both patients for all procedures. Patients were intubated carefully given concern for degrees of instability at the cranio-cervical junction, and then placed in the prone position with the head fixed. The imaging guidance system optical camera was placed at the head of the bed and the cranial reference frame was secured to the head clamp for use during screw placement (Medtronic Stealth S8, Minneapolis, MN). A standard posterior fossa Chiari decompression was performed with suboccipital craniectomy, C1 laminectomy, and duraplasty. Subsequently, the lateral masses of C2, lateral masses of C1, and the posterior portion of the OC were exposed. Using navigation, the desired entry point, trajectory, and depth to avoid violating the atlanto-occipital joint and vertebral artery caudally, the hypoglossal canal cranially, or the condylar fossa laterally was identified (Medtronic O-Arm, Minneapolis, MN) [
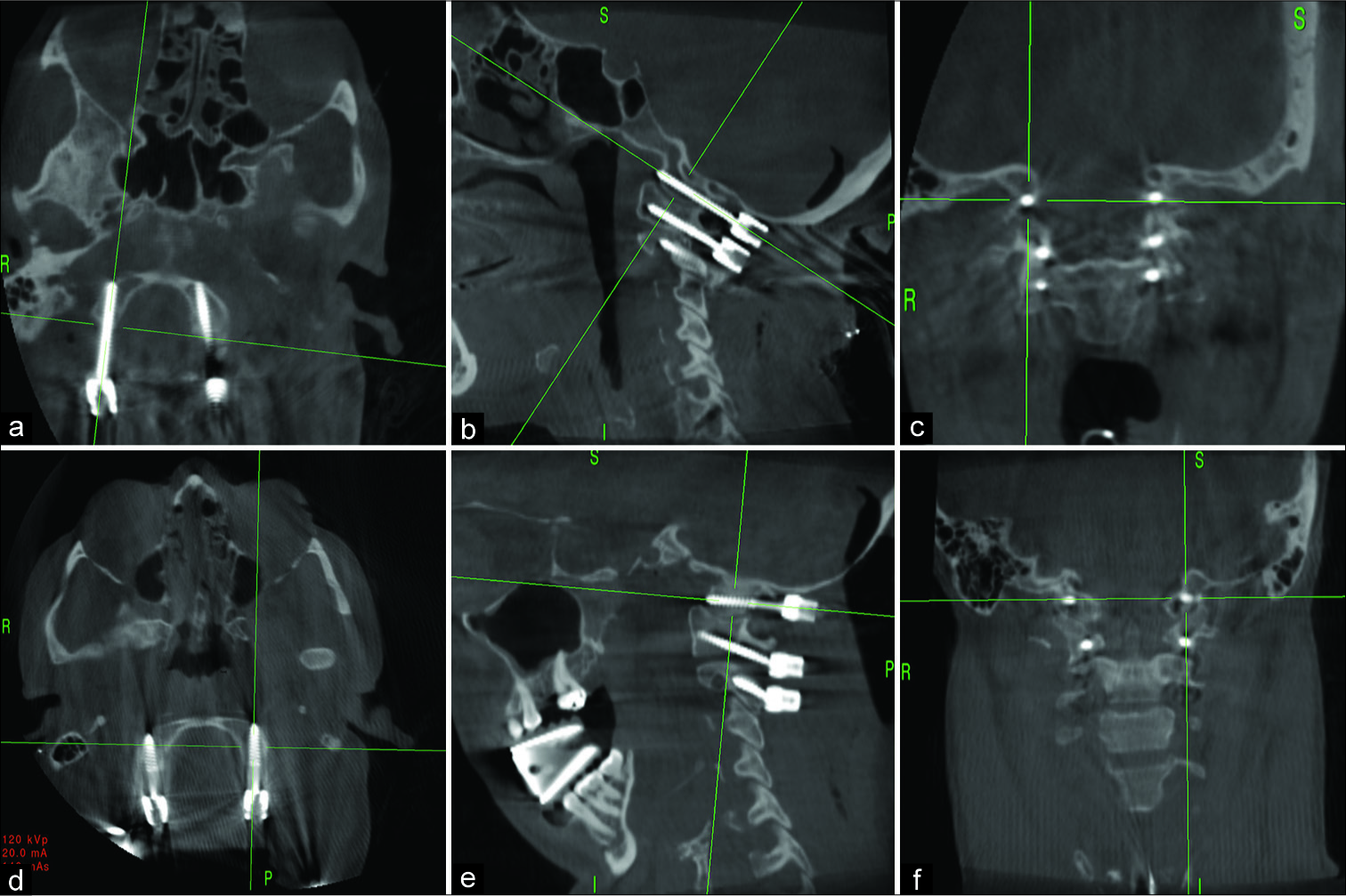
Figure 2:
(a-c) Axial, sagittal, and coronal views of intra-operative computed tomography showing secure screw placement in the occipital condyle, C1 and C2 of patient 1; and (d-f) Axial, sagittal, and coronal views of intra-operative computed tomography showing secure screw placement in the occipital condyle, C1 and C2 of patient 2.
RESULTS
Patient 1
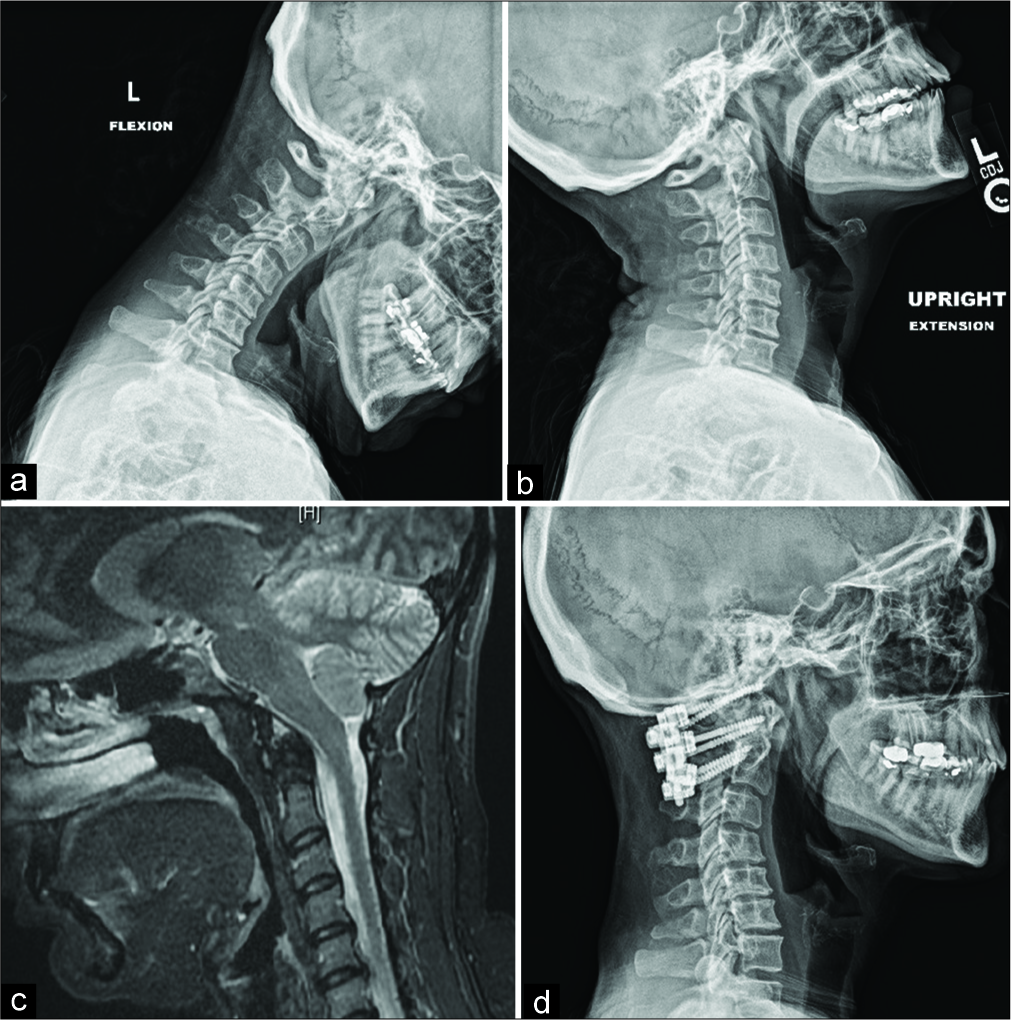
A 53-year-old woman with history of hypothyroidism and cervical spondylosis presented with suboccipital headaches for several years which worsen with exertion and bilateral paresthesia in her hands. Work-up revealed CM-1 with 1.5 cm of tonsillar ectopia, and cervical imaging revealed cervical spondylosis and a pannus behind the odontoid suggesting chronic craniocervical instability. Despite lack of obvious movement on flexion and extension lateral X-rays [
Figure 3:
(a-b) Flexion and extension X-ray of patient 1 film showing no evidence of instability and (c) C-spine magnetic resonance imaging of patient 1 showing pannus formation at C1 and (d) sagittal upright X-ray of patient 1 at 1-year follow-up demonstrating secure screw placement and stability of C-spine.
Patient 2
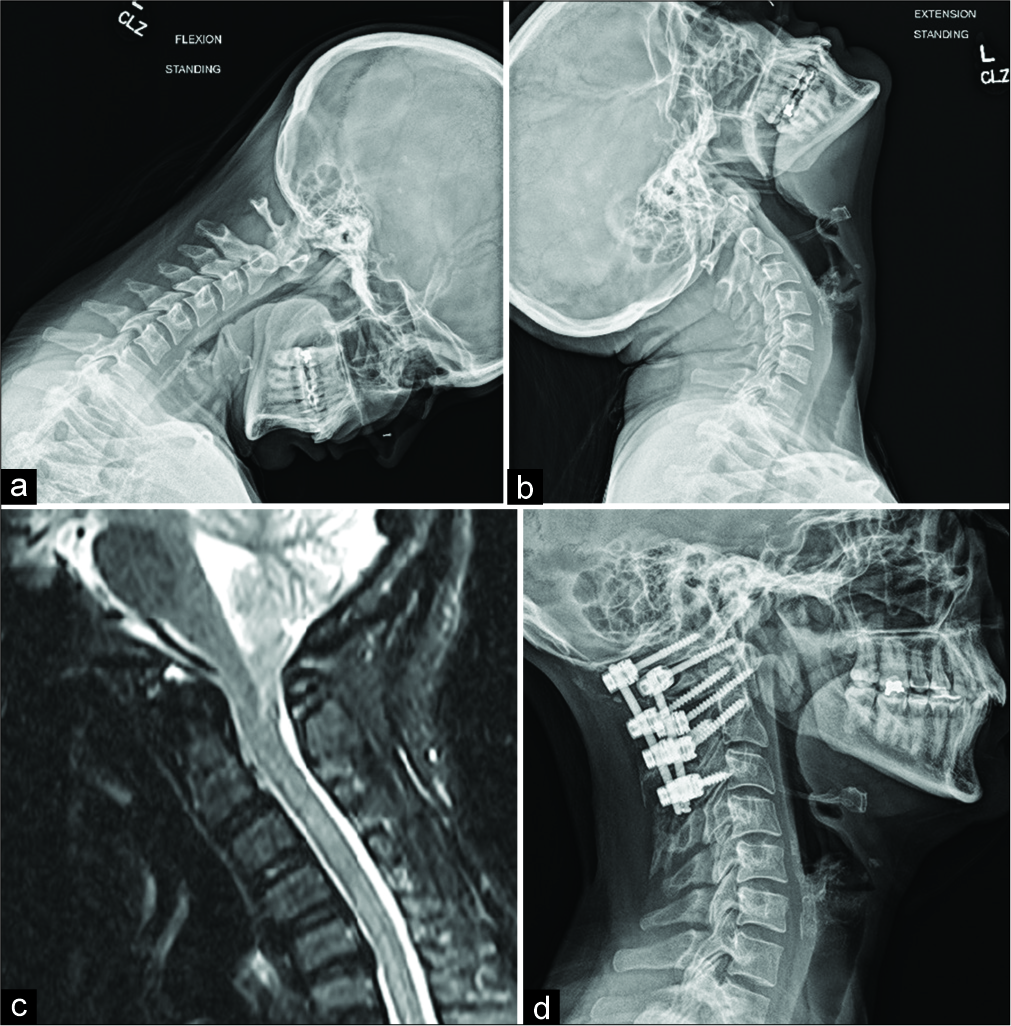
A 31-year-old woman with a history of Factor V thrombophilia, neck pain with intermittent right arm paresthesia, and post-tussive headaches was found to have CM-1 with 9.4 mm of tonsillar ectopia. Conservative management with two separate neurologists failed to relieve her headaches. Further workup revealed a small amount of pannus formation behind the dens [
Figure 4:
(a-b) Flexion and extension X-ray of patient 2 showing signs of instability and (c) C-spine magnetic resonance imaging of patient 2 showing pannus formation at behind dens of C2 and (d) sagittal upright X-ray of patient 2 at 1-year follow-up demonstrating secure screw placement and stability of C-spine.
DISCUSSION
We discuss two novel cases of successful OC fusion with OC screws following posterior decompression for two adults with CM-1 and OCJ instability. CM-1 is a syndrome that presents with headache, paresthesia, or cerebellar symptoms due to ectopic presence of cerebellar tonsils below the foramen magnum.[
Posterior fossa decompression is the standard surgical treatment in patients with CM-1, and its use has been shown to improve outcomes.[
The OCJ is a complex anatomical region, the navigation of which has challenged surgeons for decades. It is comprised the atlanto-occipital joint and the atlanto-axial joint. The vertebral arteries also pass through the OCJ, coursing superiorly from the subclavian artery to pass through the OCJ and wrapping around the OCs as they enter the dura near the foramen magnum.[
OC fusion is performed in cases of trauma, rheumatoid arthritis, congenital deformities, tumors, and degenerative disease.[
OC screw fixation for OCJ instability was first described by Uribe et al. in 2008 as a salvage technique for a surgeon’s armamentarium.[
We also hypothesize that use of OC screws may allow for better fusion rates as the technique leads to placement of hardware at each level and decortication of the joint spaces for bony fusion. Placement of autograft or allograft into the decorticated joint spaces allows for increased surface area and compression over the area to encourage fusion. Conventionally, with occipital plating, it is often impossible to instrument the C1 level due to the angle of the rods.
Placement of occipital fixation at the condyle allows for use of a short straight rod without a significant bend, eliminating this point of weakness.
Based on this study and results of our own patients, we suggest that OC screw placement for OCJ stabilization is a safe and feasible option for CM-1 patients who have undergone posterior decompression who either develop instability over time, or have degrees of radiographic evidence preoperatively indicating the possible need for fusion at the same time as the decompression.
CONCLUSION
OC screw fixation is a viable treatment for OCJ instability in patients who have undergone posterior fossa decompression. This technique may be especially applicable to patients with CM-1 receive posterior fossa decompression and who either have preoperative or postoperative evidence of OCJ instability as well.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahmadian A, Dakwar E, Vale FL, Uribe JS. Occipitocervical fusion via occipital condylar fixation: A clinical case series. J Spinal Disord Tech. 2014. 27: 232-6
2. Bekelis K, Duhaime AC, Missios S, Belden C, Simmons N. Placement of occipital condyle screws for occipitocervical fixation in a pediatric patient with occipitocervical instability after decompression for Chiari malformation. J Neurosurg Pediatr. 2010. 6: 171-6
3. Bosco A, Venugopal P, Shetty AP, Shanmuganathan R, Kanna RM. Morphometric evaluation of occipital condyles: Defining optimal trajectories and safe screw lengths for occipital condyle-based occipitocervical fixation in Indian population. Asian Spine J. 2018. 12: 214-23
4. de Oliveira Sousa U, de Oliveira MF, Heringer LC, Barcelos AC, Botelho RV. The effect of posterior fossa decompression in adult Chiari malformation and basilar invagination: A systematic review and meta-analysis. Neurosurg Rev. 2018. 41: 311-21
5. Finn MA, Bishop FS, Dailey AT. Surgical treatment of occipitocervical instability. Neurosurgery. 2008. 63: 961-8
6. Flanagan MF. The role of the craniocervical junction in craniospinal hydrodynamics and neurodegenerative conditions. Neurol Res Int. 2015. 2015: 794829
7. Foerster O.editors. Die Leitungsbahnen des Schmerzgefühls und die Chirurgische Behandlung der Schmerzzustände. Germany: Urban and Schwarzenberg; 1927. p.
8. Frankel BM, Hanley M, Vandergrift A, Monroe T, Morgan S, Rumboldt Z. Posterior occipitocervical (C0-3) fusion using polyaxial occipital condyle to cervical spine screw and rod fixation: A radiographic and cadaveric analysis. J Neurosurg Spine. 2010. 12: 509-16
9. Garrido BJ, Sasso RC. Occipitocervical fusion. Orthop Clin North Am. 2012. 43: 1-9
10. Gumussoy I, Duman SB. Morphometric analysis of occipital condyles using alternative imaging technique. Surg Radiol Anat. 2020. 42: 161-9
11. Karaaslan B, Börcek AÖ, Uçar M, Aykol Ş. Can the etiopathogenesis of chiari malformation be craniocervical junction stabilization difference? Morphometric analysis of craniocervical junction ligaments. World Neurosurg. 2019. 128: e1096-101
12. Karam YR, Traynelis VC. Occipital condyle fractures. Neurosurgery. 2010. 66: A56-9
13. Kirnaz S, Gerges MM, Rumalla K, Bernardo A, Baaj AA, Greenfield JP. Occipital condyle screw placement in patients with chiari malformation: A radiographic feasibility analysis and cadaveric demonstration. World Neurosurg. 2020. 136: 470-8
14. Kosnik-Infinger L, Glazier SS, Frankel BM. Occipital condyle to cervical spine fixation in the pediatric population. J Neurosurg Pediatr. 2014. 13: 45-53
15. La Marca F, Zubay G, Morrison T, Karahalios D. Cadaveric study for placement of occipital condyle screws: Technique and effects on surrounding anatomic structures. J Neurosurg Spine. 2008. 9: 347-53
16. Langridge B, Phillips E, Choi D. Chiari malformation Type 1: A systematic review of natural history and conservative management. World Neurosurgery. 2017. 104: 213-9
17. Le TV, Burkett C, Ramos E, Uribe JS. Occipital condyle screw placement and occipitocervical instrumentation using three-dimensional image-guided navigation. J Clin Neurosci. 2012. 19: 757-60
18. Le TV, Dakwar E, Hann S, Effio E, Baaj AA, Martinez C. Computed tomography-based morphometric analysis of the human occipital condyle for occipital condyle-cervical fusion. J Neurosurg Spine. 2011. 15: 328-31
19. Lee HJ, Choi DY, Shin MH, Kim JT, Kim IS, Hong JT. Anatomical feasibility for safe occipital condyle screw fixation. Eur Spine J. 2016. 25: 1674-82
20. Lin SL, Xia DD, Chen W, Li Y, Shen ZH, Wang XY. Computed tomographic morphometric analysis of the pediatric occipital condyle for occipital condyle screw placement. Spine (Phila Pa 1976). 2014. 39: E147-52
21. Srivastava A, Nanda G, Mahajan R, Nanda A, Mishra N, Karmaran S. Computed tomography-based occipital condyle morphometry in an Indian population to assess the feasibility of condylar screws for occipitocervical fusion. Asian Spine J. 2017. 11: 847-53
22. Uribe JS, Ramos E, Baaj A, Youssef AS, Vale FL. Occipital cervical stabilization using occipital condyles for cranial fixation: Technical case report. Neurosurgery. 2009. 65: E1216-7
23. Uribe JS, Ramos E, Vale F. Feasibility of occipital condyle screw placement for occipitocervical fixation: A cadaveric study and description of a novel technique. J Spinal Disord Tech. 2008. 21: 540-6
24. Vaccaro AR, Lim MR, Lee JY. Indications for surgery and stabilization techniques of the occipito-cervical junction. Injury. 2005. 36: B44-53
25. Vender JR, Rekito AJ, Harrison SJ, McDonnell DE. The evolution of posterior cervical and occipitocervical fusion and instrumentation. Neurosurg Focus. 2004. 16: E9
26. Wagner A, Grassner L, Kögl N, Hartmann S, Thomé C, Wostrack M. Chiari malformation Type I and basilar invagination originating from atlantoaxial instability: A literature review and critical analysis. Acta Neurochir (Wien). 2020. 162: 1553-63
27. Winegar CD, Lawrence JP, Friel BC, Fernandez C, Hong J, Maltenfort M. A systematic review of occipital cervical fusion: Techniques and outcomes. J Neurosurg Spine. 2010. 13: 5-16
28. Zarghooni K, Boese CK, Siewe J, Rollinghoff M, Eysel P, Scheyerer MJ. Occipital bone thickness: Implications on occipital-cervical fusion. A cadaveric study. Acta Orthop Traumatol Turc. 2016. 50: 606-9
29. Zhou J, Orias AA, Kang X, He J, Zhang Z, Inoue N. CT-based morphometric analysis of the occipital condyle: Focus on occipital condyle screw insertion. J Neurosurg Spine. 2016. 25: 572-9