- Division of Neurosurgery, Toronto Western Hospital, University of Toronto, Toronto, Ontario, Canada
Correspondence Address:
Mohammed F. Shamji
Division of Neurosurgery, Toronto Western Hospital, University of Toronto, Toronto, Ontario, Canada
DOI:10.4103/2152-7806.172531
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Guha D, Mohanty C, Tator CH, Shamji MF. Occipital neuralgia secondary to unilateral atlantoaxial osteoarthritis: Case report and review of the literature. Surg Neurol Int 23-Dec-2015;6:186
How to cite this URL: Guha D, Mohanty C, Tator CH, Shamji MF. Occipital neuralgia secondary to unilateral atlantoaxial osteoarthritis: Case report and review of the literature. Surg Neurol Int 23-Dec-2015;6:186. Available from: http://surgicalneurologyint.com/surgicalint_articles/occipital-neuralgia-secondary-to-unilateral-atlantoaxial-osteoarthritis-case-report-and-review-of-the-literature/
Abstract
Background:Atlantoaxial osteoarthritis (AAOA), either in isolation or in the context of generalized peripheral or spinal arthritis, presents most commonly with neck pain and limitation of cervical rotational range of motion. Occipital neuralgia (ON) is only rarely attributed to AAOA, as fewer than 30 cases are described in the literature.
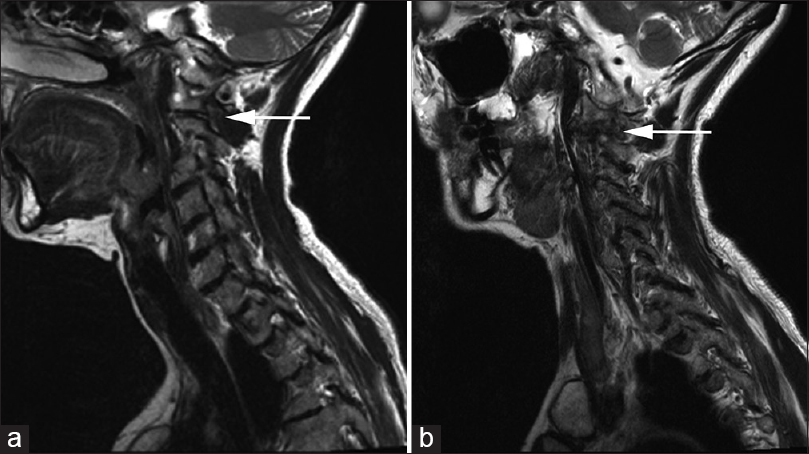
Case Description:A 64-year-old female presented with progressive incapacitating cervicalgia and occipital headaches, refractory to medications, and local anesthetic blocks. Computed tomography and magnetic resonance imaging studies documented advanced unilateral atlantoaxial arthrosis with osteophytic compression that dorsally displaced the associated C2 nerve root. Surgical decompression and atlantoaxial fusion achieved rapid and complete relief of neuralgia. Ultimately, postoperative spinal imaging revealed osseous union.
Conclusions:Atlantoaxial arthrosis must be considered in the differential diagnosis of ON. Surgical treatment is effective for managing refractory cases. Intraoperative neuronavigation is also a useful adjunct to guide instrumentation and the intraoperative extent of bony decompression.
Keywords: Atlantoaxial fusion, occipital neuralgia, osteoarthritis
INTRODUCTION
Atlantoaxial osteoarthritis (AAOA) typically presents with neck pain and restricted cervical rotation. Occipital neuralgia (ON), characterized by lancinating pain and dysesthesia in the distribution of the greater and lesser occipital nerves, is most commonly idiopathic but may occur when the C2 or C3 nerve roots are statically or dynamically compressed. Potential surgical etiologies include instability following prior trauma or surgery, compression from neoplasms, gross atlantoaxial instability secondary to rheumatoid arthritis, nerve entrapment by a hypertrophic atlanto-epistrophic ligament, or mechanical compression from a severely congested C2 venous plexus, or ectatic vertebral artery.[
Here, we present a patient who has ON and severe upper cervical pain was attributed to unilateral AAOA. As she was refractory to medical therapy, she underwent osteophyte decompression with posterior atlantoaxial fusion utilizing a frameless stereotactic navigation system.
CASE HISTORY
A 64-year-old female presented with several years of progressive intractable cervicalgia and occipital headache; there was no trauma history. She had restricted cervical rotation/left head tilt and neck spasms, accompanied by pain in the left suboccipital region, radiating to the left occipital scalp, and left ear (paraorbital region). There was no history of peripheral or spinal osteoarthritis or any other rheumatologic conditions.
Notably, two attempts at left occipital nerve blocks were made in the year prior to surgery; both resulted in clear albeit modest immediate improvement, but without lasting benefit.
On examination, the patient was neurologically intact but demonstrated exquisite tenderness to light touch over the left occipital scalp.
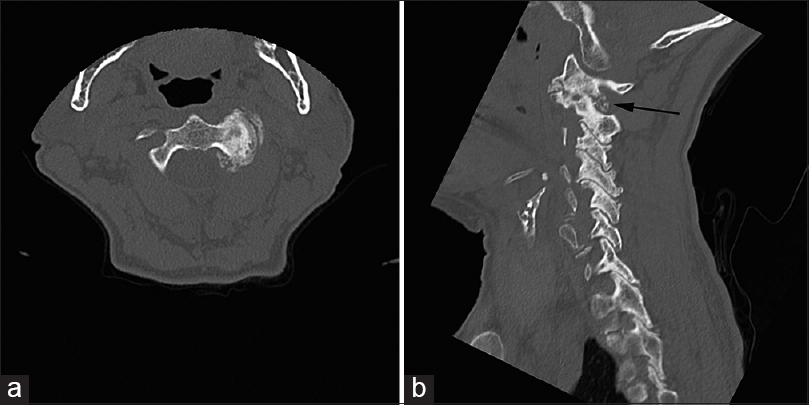
The computed tomography (CT) of the cervical spine revealed advanced unilateral arthrosis on the left involving the C1–C2 facet joint, accompanied by significant posterior osteophytic protrusion into the left C1–C2 foramen [
Figure 1
Axial (a) and left paramedian sagittal (b) preoperative computed tomography of the cervical spine. Unilateral arthrosis of the left C1–C2 facet joint is shown with obliteration of the joint space and extensive osteophyte formation. The posterior osteophyte encroaches into the expected site of the left C2 dorsal ramus (black arrow)
Surgical procedure
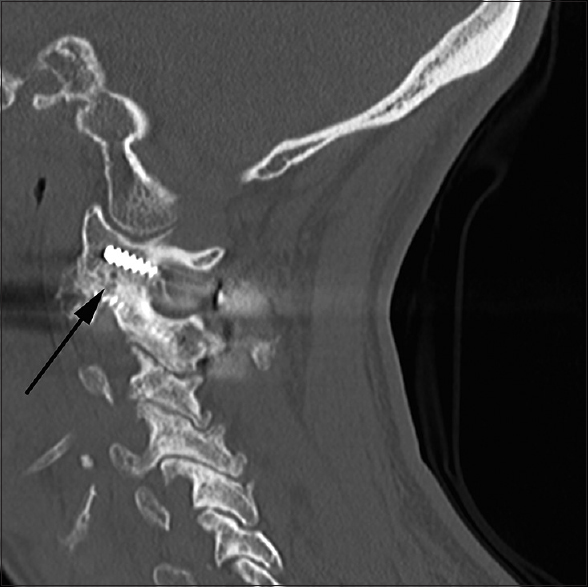
A posterior upper cervical approach was implemented, and intraoperative CT three-dimensional stereotactic navigation was utilized. At surgery, the C2 nerve root was retracted while the osteophytic complex was removed. Autograft was placed into both C1–C2 facet joints and with navigation, bilateral C1 lateral mass, and C2 pedicle screws/rods were placed without complication.[
Postoperative course
Postoperatively, the patient remained neurologically intact with a complete and immediate resolution of her cervicalgia and lancinating occipital headache. She was placed in an Aspen cervical orthosis for 12 weeks after which it was weaned, and active neck physiotherapy was implemented. At 3-month postoperative follow-up, she remained free of her ON and neck pain with radiographic confirmation of osseous union across the C1–C2 facet joints and excellent foraminal decompression [
DISCUSSION
ON was first described formally by Hunter and Mayfield in 1949 and is characterized by paroxysmal lancinating pain in the distribution of the greater or lesser occipital nerves, variably accompanied by a dull ache between episodes.[
AAOA refers to degenerative arthrosis of the lateral (facet) or central atlantoaxial joints, afflicting the facet joint in 12%, atlanto-odontoid articulation in 17%, and both in 71%.[
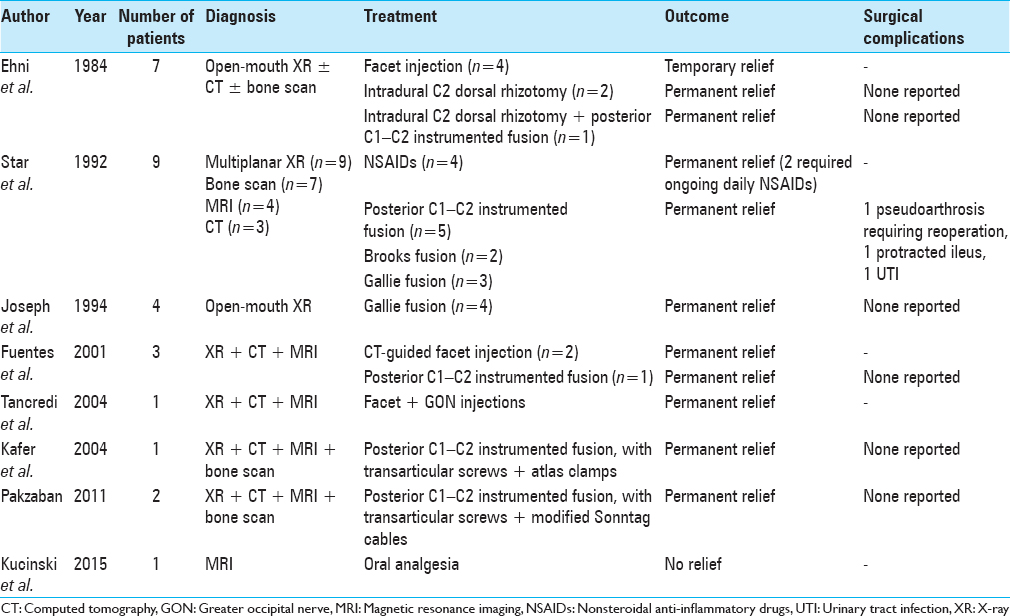
The first formal description of ON secondary to lateral AAOA was by Ehni and Benner in a series of seven patients described in
Our review of the literature revealed 29 cases of true ON secondary to lateral AAOA, 17 treated surgically. Operative treatment included either intradural C2 dorsal rhizotomy or C1–C2 instrumented fusion, without decompression even in cases with clear osteophytic nerve root compression.[
Our case uniquely underwent decompression of a posterior atlantoaxial osteophyte in addition to fusion. This has been replicated in other series of ON secondary to posttraumatic atlantoaxial arthrosis and hyperostosis.[
CONCLUSIONS
ON is a rare sequela of lateral AAOA. Diagnosis is suspected clinically and confirmed with radiographic evidence of facet arthrosis. Workup also includes ruling out other structural lesions with CT and MRI, and investigating instability with dynamic radiographs. Atlantoaxial fusion is an effective option for refractory cases, and intraoperative frameless stereotaxy is a useful adjunct to guide hardware placement as well as to define the extent of osteophyte decompression. Atlantoaxial focal foraminal decompression and instrumented fusion is an effective option.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Clavel M, Clavel P. Occipital neuralgia secondary to exuberant callus formation. Case report. J Neurosurg. 1996. 85: 1170-1
2. Dreyfuss P, Michaelsen M, Fletcher D. Atlanto-occipital and lateral atlanto-axial joint pain patterns. Spine (Phila Pa 1976). 1994. 19: 1125-31
3. Ehni G, Benner B. Occipital neuralgia and the C1-2 arthrosis syndrome. J Neurosurg. 1984. 61: 961-5
4. Elliott RE, Tanweer O, Smith ML, Frempong-Boadu A. Outcomes of fusion for lateral atlantoaxial osteoarthritis: Meta-analysis and review of literature. World Neurosurg. 2013. 80: e337-46
5. Fuentes S, Bouillot P, Palombi O, Manera L, Desgeorges M. Atlanto-axial lateral mass osteoarthritis. Three case reports and review of the literature. Neurochirurgie. 2001. 47: 51-4
6. Ghanayem AJ, Leventhal M, Bohlman HH. Osteoarthrosis of the atlanto-axial joints. Long-term follow-up after treatment with arthrodesis. J Bone Joint Surg Am. 1996. 78: 1300-7
7. Halla JT, Hardin JG. Atlantoaxial (C1-C2) facet joint osteoarthritis: A distinctive clinical syndrome. Arthritis Rheum. 1987. 30: 577-82
8. Harata S, Tohno S, Kawagishi T. Osteoarthritis of the alanto-axial joint. Int Orthop. 1981. 5: 277-82
9. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001. 26: 2467-71
10. Hunter CR, Mayfield FH. Role of the upper cervical roots in the production of pain in the head. Am J Surg. 1949. 78: 743-51
11. Joseph B, Kumar B. Gallie's fusion for atlantoaxial arthrosis with occipital neuralgia. Spine (Phila Pa 1976). 1994. 19: 454-5
12. Käfer W, Cakir B, Richter M. Osteoarthritis – A rare indication for atlantoaxial fusion. A case report and review of the literature. Acta Orthop Belg. 2004. 70: 380-5
13. Kucinski T, Schubert J. FOAR: Facet Joint Osteoarthritis with Radiculopathy: A case series and a hypothesis explaining spinal nerve irritation in the absence of osteodiskal compression. Clin Neuroradiol. 2015. 25: 83-7
14. Kuhn WF, Kuhn SC, Gilberstadt H. Occipital neuralgias: Clinical recognition of a complicated headache. A case series and literature review. J Orofac Pain. 1997. 11: 158-65
15. Pakzaban P. Transarticular screw fixation of C1-2 for the treatment of arthropathy-associated occipital neuralgia. J Neurosurg Spine. 2011. 14: 209-14
16. Schaeren S, Jeanneret B. Atlantoaxial osteoarthritis: Case series and review of the literature. Eur Spine J. 2005. 14: 501-6
17. Sharma RR, Parekh HC, Prabhu S, Gurusinghe NT, Bertolis G. Compression of the C-2 root by a rare anomalous ectatic vertebral artery. Case report. J Neurosurg. 1993. 78: 669-72
18. Star MJ, Curd JG, Thorne RP. Atlantoaxial lateral mass osteoarthritis. A frequently overlooked cause of severe occipitocervical pain. Spine (Phila Pa 1976). 1992. 17: S71-6
19. White JB, Atkinson PP, Cloft HJ, Atkinson JL. Vascular compression as a potential cause of occipital neuralgia: A case report. Cephalalgia. 2008. 28: 78-82
20. Zapletal J, de Valois JC. Radiologic prevalence of advanced lateral C1-C2 osteoarthritis. Spine (Phila Pa 1976). 1997. 22: 2511-3