- Department of NeuroScience, Chief of Neurosurgical Spine and Education, Winthrop University Hospital, Mineola, NY 11501, USA
- Vice President Operative Services, Winthrop University Hospital, Mineola, NY 11501, USA
- Chief Executive Officer, Winthrop University Hospital, Mineola, NY 11501, USA
Correspondence Address:
Nancy E. Epstein
Chief Executive Officer, Winthrop University Hospital, Mineola, NY 11501, USA
DOI:10.4103/2152-7806.156574
Copyright: © 2015 Epstein NE. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Epstein NE, Roberts R, Collins J. Operative costs, reasons for operative waste, and vendor credit replacement in spinal surgery. Surg Neurol Int 07-May-2015;6:
How to cite this URL: Epstein NE, Roberts R, Collins J. Operative costs, reasons for operative waste, and vendor credit replacement in spinal surgery. Surg Neurol Int 07-May-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/operative-costs-reasons-operative-waste-vendor-credit/
Abstract
Background:In 2012, Epstein et al. documented that educating spinal surgeons reduced the cost of operative waste (explanted devices: placed but removed prior to closure) occurring during anterior cervical diskectomy/fusion from 20% to 5.8%.[
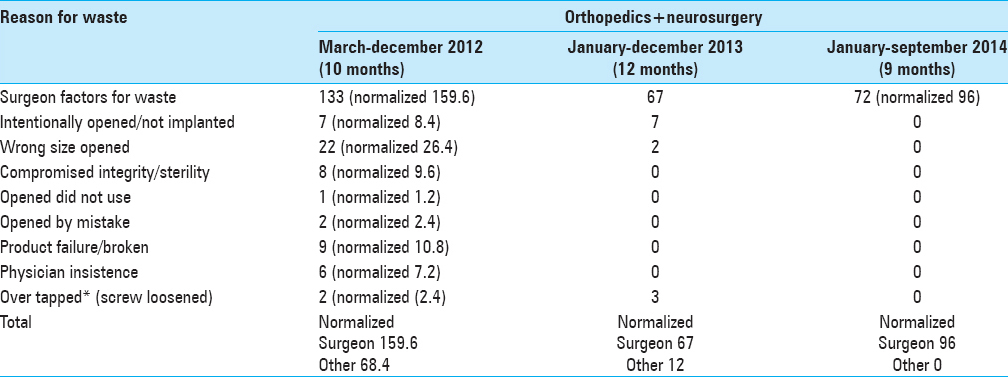
Methods:The spine surgeon-education program involved posting the data for operative costs of waste and the nine reasons for operative waste over the neurosurgery/orthopedic scrub sinks every quarter. These data were compared for 2012 (latter 10 months), 2013 (12 months), and 2014 (first 9 months) (e.g. data were normalized). Savings from a 2013 Vendor Credit Replacement program were also calculated.
Results:From 2012 to 2013 and 2014, spinal operative costs for waste were, respectively reduced by 64.7% and 61% for orthopedics, and 49.4% and 45.2% for neurosurgery. Although reduced by the program, the major reason for operative waste for all 3 years remained surgeon-related factors (e.g. 159.6, to 67, and 96, respectively). Alternatively, the eight other reasons for operative waste were reduced from 68.4 (2012) to 12 (2013) and finally to zero by 2014. Additionally, the Vendor Replacement program for 2013 netted $78,564.
Conclusions:The spine surgeon-education program reduced the costs/reasons for operative waste for 2012 to lower levels by 2013 and 2014. Although the major cost/reasons for operative waste were attributed to surgeon-related factors, these declined while the other eight reasons for operative waste were reduced to zero by 2014.
Keywords: Cost operative waste, education program, nine reasons, spine surgeon, surgeon-related factors, vendor replacement program
INTRODUCTION
Based on prior studies, we determined that the high incidence of operative waste in spinal surgery substantially adds to its total costs (costs to the hospital without overhead, not charges that include overhead). Epstein et al. documented that the total costs for instrumentation implanted by 15 spinal surgeons performing 102 anterior cervical diskectomy and fusion (ACDF) in 2008 at one institution was $355,863; the total cost of wasted devices (explanted devices; implanted but removed prior to closure) unnecessarily added $32,850 (9.2%) to that cost.[
MATERIALS AND METHODS
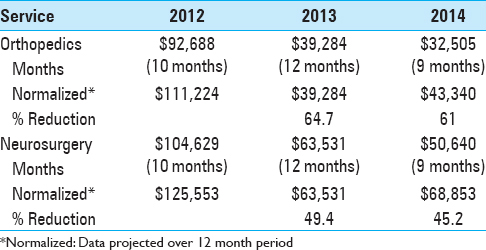
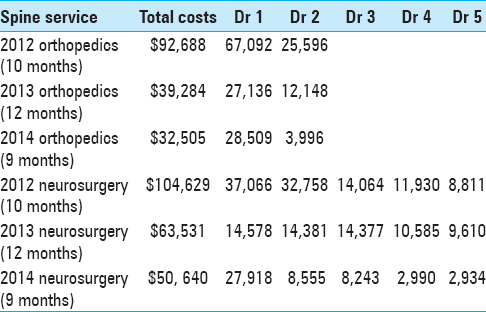
The spine surgeon-education program included recording the cost of wasted materials (without overhead, not charges that include overhead) and the nine reasons for operative waste occurring in 2012 (latter 10 months), 2013 (12 months), and 2014 (first 9 months) [Tables
RESULTS
Costs of waste in spinal orthopedics and spinal neurosurgery
For 2012-2014 (Normalized Data) [Tables 1 and 2 ]
The costs of operative waste for all spinal orthopedic and spinal neurosurgery procedures performed in 2012 (latter 10 months) were reduced in 2013 (12 months) and 2014 (first 9 months) to 64.7% and 61% for orthopedics, and to 49.4% and 45.2% for neurosurgery, respectively (data were normalized) [
Reasons for waste in spinal orthopedic and spinal neurosurgery 2012-2014
Of the nine reasons for operative waste recorded for 2012-2014, surgeon-related factors decreased but were still the most responsible for waste; 159.6 (2012) to 67 (2013), and 96 (2014) [
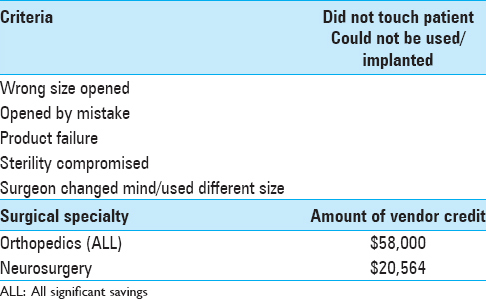
Results of vendor credit replacement for all of orthopedics and spinal neurosurgery in 2013 [ Table 4 ]
The Vendor Credit Replacement netted $58,000 for all of orthopedics (including joint replacement and spinal surgery), and $20,564 for spinal neurosurgery in 2013; the total was $78,564 [
DISCUSSION
United States trends in lumbar fusion surgery for degenerative conditions
In 2005, Deyo et al. used the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (1988-2001) to evaluate trends in spinal surgery.[
Surgeon choices, and the choice of surgeons affect total hospital charges for single-level anterior cervical surgery (2008)
In 2008, Epstein et al. examined the variations in total hospital charges (charges defined as including overhead vs. costs without overhead), and determined how surgeons impacted these charges. They retrospectively analyzed the total hospital charges for 15 spinal surgeons performing 102 single-level ACDF (1-ACDF) during a single year (2008) at one institution ([DRG] category 473: cervical spine fusion; Principle Procedure Code [81.02]).[
The incidence and costs of devices explanted during single-level anterior diskectomy/fusions: Data from the 2009 Study
In 2009, Epstein et al. observed that little is known about the costs (without overhead differentiated from charges that include overhead) of devices paid for by the hospitals, and explanted during 87 ACDF procedures performed at one hospital.[
Reducing the cost and frequency of explanations associated with single-level anterior diskectomy and fusion at a single institution through education (2010)
In 2010, Epstein et al. prospectively evaluated the costs (without overhead to the hospital, differentiated from charges that include overhead) and frequency of explanted instrumentation (devices implanted but removed prior to closure) for all single-level ACDF performed by 15 spine surgeons at a single institution before and after surgeon education.[
Costs and frequency of “off-label” use of Bone Morphogenetic Protein/INFUSE (Medtronic, Memphis, TN, USA) for spinal fusions at one institution in 2010
In 2010, Epstein and Schwall evaluated the costs (without overhead to the hospital, differentiated from charges that include overhead) and frequency of “on-label” vs. “off-label” use of Bone Morphogenetic Protein (BMP)/INFUSE (Medtronic, Memphis, TN, USA) utilized in the performance of all types of spinal fusions at one institution in 2010.[
Intraoperative waste in spine surgery: Incidence, cost, and effectiveness of an educational program (2011)
In 2011, Soroceanu et al. examined whether an educational program would reduce the cost (without overhead to the hospital, differentiated from charges that include overhead) of intraoperative waste occurring in spine surgery at one academic medical center, and paid particular attention to the costs of spinal implants.[
Lean principles to optimize instrument utilization for spine surgery in an academic medical center
Lunardini et al. introduced “process improvement systems” to better assess routines/efficiency/uniformity for implanting spinal instrumentation, while reducing costs (without overhead to the hospital, differentiated from charges that include overhead) in an urban level 1 academic medical center.[
Summary
The spine surgeon-education program introduced in the latter part of 2012 (10 months) and continued through 2013 (12 months) and 2014 (first 9 months), substantially reduced the cost of operative waste in spinal orthopedics (64.7% [2013] and 61% [2014]) and spinal neurosurgery (49.4% [2013] and 45.2% [2014]). The major reason for operative waste, attributed to surgeon-related factors, decreased over this time period, while all eight other reasons for operative waste were reduced to 0 by 2014.
References
1. Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005. 30: 1441-5
2. Epstein NE, Schwall GS. Costs and frequency of “off-label” use of INFUSE for spinal fusions at one institution in 2010. Surg Neurol Int. 2011. 2: 115-
3. Epstein NE, Schwall G, Reillly T, Insinna T, Bahnken A, Hood DC. Surgeon choices, and the choice of surgeons, affect total hospital charges for single-level anterior cervical surgery. Spine (Phila Pa 1976). 2011. 36: 905-9
4. Epstein NE, Schwall GS, Hood DC. The incidence and cost of devices explanted during single-level anterior diskectomy/fusions. Surg Neurol Int. 2011. 2: 23-
5. Epstein NE, Schwall GS, Hood DC. Reducing the cost and frequency of explantations associated with single-level anterior diskectomy and fusion at a single institution through education. Spine (Phila Pa 1976). 2012. 37: 414-7
6. Lunardini D, Arington R, Canacari EG, Gamboa K, Wagner K, McGuire KJ. Lean principles to optimize instrument utilization for spine surgery in an academic medical center: An opportunity to standardize, cut costs, and builds a culture of improvement. Spine (Phila Pa 1976). 2014. 39: 1714-7
7. Soroceanu A, Canacari E, Brown E, Robinson A, McGuire KJ. Intraoperative waste in spine surgery: Incidence, cost, and effectiveness of an educational program. Spine (Phila Pa 1976). 2011. 36: E1270-3