- Department of Neurosurgery, University of Kansas Health System, Kansas City, Kansas
- Department of Neurological Surgery, University of Kansas Medical Center, Kansas City, Kansas.
- Department of Plastic Surgery, University of Kansas Medical Center, Kansas City, Kansas.
Correspondence Address:
Luke Weisbrod
Department of Plastic Surgery, University of Kansas Medical Center, Kansas City, Kansas.
DOI:10.25259/SNI_323_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Luke Weisbrod, Kyle Smith, Paul Camarata, Anthony Alvarado, Brian Andrews. Orbital myxoma: A case report. 13-Mar-2020;11:43
How to cite this URL: Luke Weisbrod, Kyle Smith, Paul Camarata, Anthony Alvarado, Brian Andrews. Orbital myxoma: A case report. 13-Mar-2020;11:43. Available from: https://surgicalneurologyint.com/surgicalint-articles/9898/
Abstract
Background: Myxomas are rare, locally infiltrative, benign neoplasms of mesenchymal origin. Although benign, these tumors are locally aggressive with a high rate of recurrence following conservative resection. Their relative infrequency, variable location, and insidious growth present a diagnostic challenge to clinicians. Cases of myxomas have been described throughout the body, but intraosseous myxomas of the orbit are exceedingly rare.
Case Description: We report a case of a 53-year-old male with a history of chronic sinusitis and symptoms of hyposmia and bifrontal headaches refractory medical management who presented for neurosurgical evaluation after radiographic findings of an orbital lesion. Physical examination was unremarkable with intact extraocular movements. Prior radiographic workup demonstrated a 2.4 × 2.7 × 2.2 cm expansile lesion involving the bony left superior and lateral orbit. A prior open biopsy was performed which demonstrated a low-grade spindle cell neoplasm consistent with intraosseous myxoma. Definitive resection was recommended through the left orbitozygomatic craniotomy. The patient tolerated the procedure well without complications. Gross total resection was achieved. Reconstruction of the orbital roof and lateral orbital wall was performed with a frontal bone autograft and titanium plating. Postoperative course was uneventful, and the patient was discharged home postoperative day 2. At 1-month follow-up visit, the patient remained neurologically intact. Surveillance imaging at 6 months and 1 year remained stable without signs of recurrence.
Conclusion: Intraosseous orbital myxomas are exceedingly rare entities. Although they are considered benign neoplasms, myxomas demonstrate high recurrence rates. The authors report a unique case of an orbital myxoma that was successfully treated through an orbitozygomatic approach achieving gross total resection.
Keywords: Intraosseous, Myxoma, Orbit
INTRODUCTION
Myxomas are rare, benign neoplasms of mesenchymal origin.[
Myxomas have been described throughout the body, but within the head-and-neck region, they most often occur in the mandible and less commonly in the maxilla.[
MATERIALS AND METHODS
We report a case of a 53-year-old male who presented with a history of chronic sinusitis after the failure of three courses of antibiotics. Initial symptoms included 3 months of purulent rhinorrhea, hyposmia, cough, and bifrontal headache.
Physical examination was unremarkable and extraocular movements were intact.
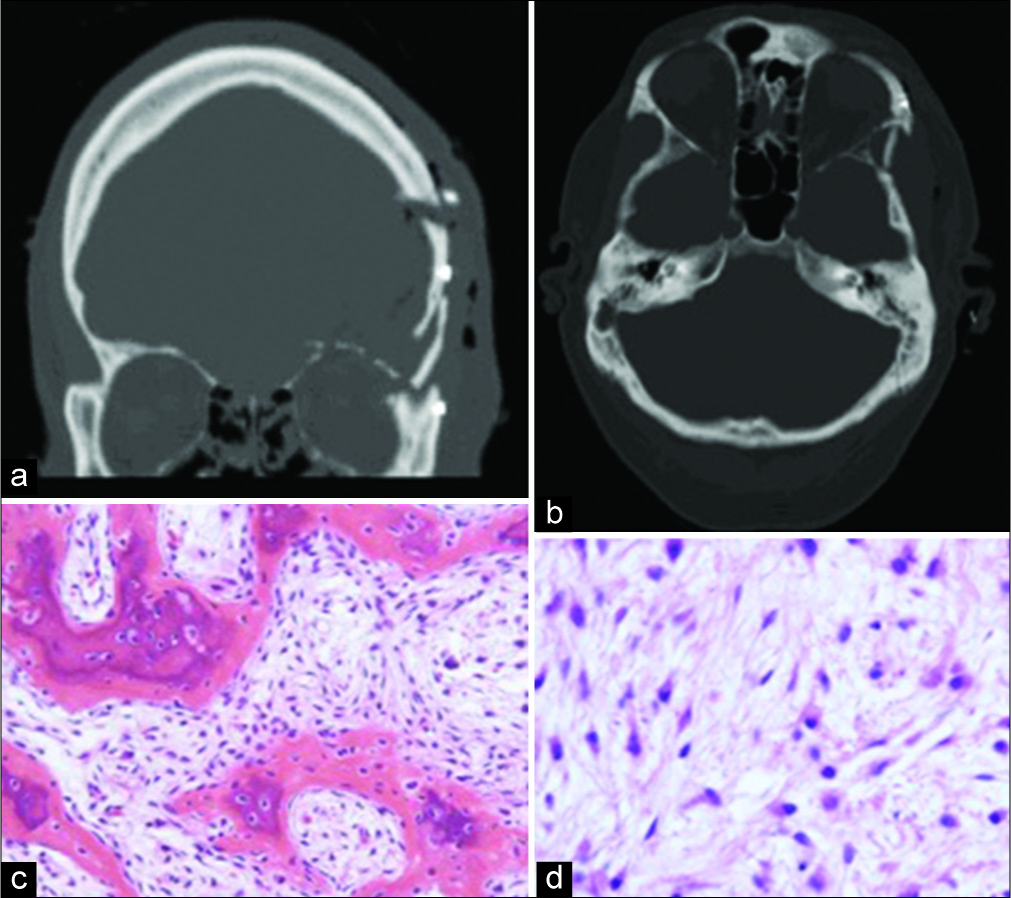
Computed tomography and magnetic resonance imaging were subsequently obtained. Imaging revealed a 2.4 × 2.7 × 2.2 cm expansile lesion involving the bony superior and lateral orbit [
Figure 1:
(a and b) Coronal and axial views of non-contrast computed tomography sinus revealing a 2.4 × 2.7 × 2.2 cm expansile lesion involving the bony superior and lateral orbit. There are cortical thinning and loss of portions of the cortical margin, expansion into the left anterior cranial fossa table, and a central matrix with chondroid density, (c and d) T2 coronal and axial magnetic resonance imaging demonstrating the T2 hyperintense and T1 hypointense lesion involving the greater wing of the sphenoid, lateral orbital wall, and orbital roof. Faint dural enhancement of the left anterior cranial fossa overlying the mass was also noted.
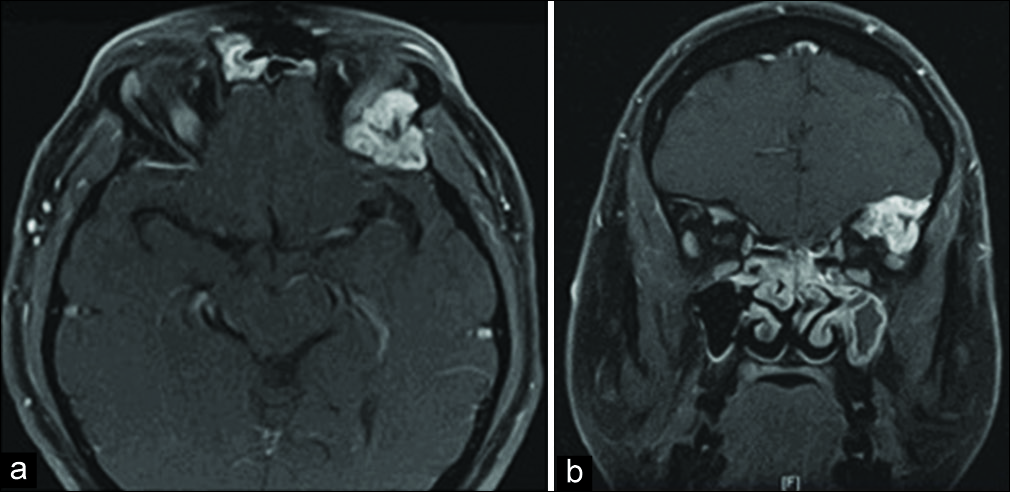
Operative biopsy through an infrabrow approach was done in conjunction with functional endoscopic sinus surgery. With respect to the biopsy, dissection was carried along the periosteum of the superior-lateral orbital rim until the lesion was encountered approximately 1.5 cm posterior to the superior orbital rim. The lesion was soft and friable compared to the surrounding bone. Specimen was sent for pathology. Frozen specimens were reported to be positive for low-grade spindle cell neoplasm. Permanent pathology later revealed intraosseous myxoma [
Figure 2:
H and E stained sections of the biopsied lesion. (a) Histopathologic analysis of biopsy specimens revealed a hypocellular tumor composed of spindle, stellate, and polyhedral cells within a myxoid stroma, (b) Low-power image reveals reactive woven bone within the myxoma. Immunohistochemistry was positive for vimentin and CD68 and negative for BER-EP4, SMA, S100, MSA, CAM-5.2, PAN-CK, CD34, CD138, and CD1A. These findings were consistent with intraosseous myxoma.
He received definite resection through the left orbitozygomatic craniotomy and gross total resection was achieved. Tumor was densely adherent to periorbita and dura; involved tissue was resected. Reconstruction of orbital roof and lateral orbital wall was done through frontal bone autograft and titanium plating.
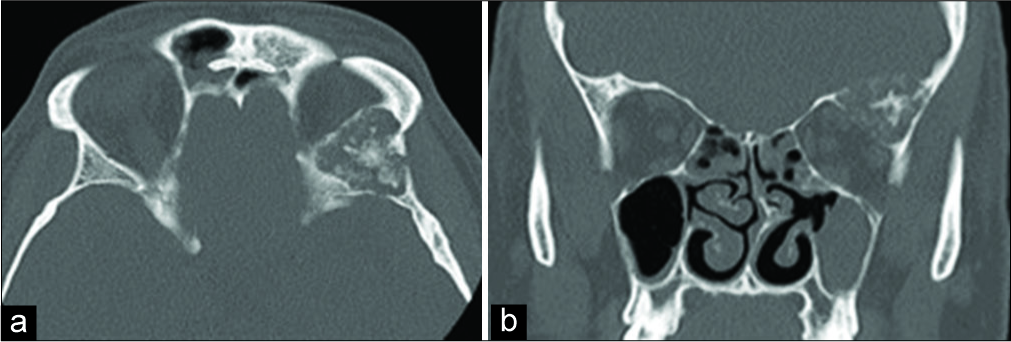
The patient recovered well. No residual bony lesions have been identified on postoperative imaging [
Figure 3:
(a) Axial and (b) coronal cuts of postoperative computed tomography head without contrast following resection of the left superior orbital rim and lateral orbital wall bony mass lesion show no residual bony lesion. Expected small area of the left frontal and soft-tissue extra-axial gas is also noted on sagittal view.
RESULTS AND DISCUSSION
Myxomas are uncommon, benign, mesenchymal neoplasms that usually arise from soft tissues, most commonly from the left atrium of the heart.[
Typically slow-growing, painless masses, these tumors may become quite large before detection, typically presenting with slowly progressive painless proptosis. Our patient did not present with proptosis, instead, the mass was only discovered during the work-up of chronic sinusitis.
Radiographic characteristics of myxoma include[
Definitive diagnosis depends on histopathology and is pivotal to eliminate the possibility of a sarcomatous component. Many reactive and neoplastic processes may show prominent myxoid degeneration and must be separated from the benign myxoma.[
Wide local excision with safety margins is the recommended treatment for both primary and recurrent cases due to the radioresistant and locally invasive nature of myxomas.[
Regardless of location, complete resection is indicated, as recurrence rates are high with conservative surgical management. Myxomas of the head and neck have recurrence rates as high as 28% with conservative surgical interventions, including enucleation and curettage, in contrast to 6% for local or wide excision.[
CONCLUSION
Our case presented above illustrates a unique surgical challenge given its proximity to both the orbit and middle cranial fossa. A multidisciplinary approach with otolaryngology and plastic surgery was utilized to achieve complete resection and reconstruction with desired outcome.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Andrews T, Kountakis SE, Maillard AA. Myxomas of the head and neck. Am J Otolaryngol. 2000. 21: 184-9
2. Bajaj MS, Mehta M, Kashyap S, Pushker N, Lohia P, Chawla B. Clinical and pathologic profile of angiomyxomas of the orbit. Ophthalmic Plast Reconstr Surg. 2011. 27: 76-80
3. Batsakis JG. Myxomas of soft tissues and the facial skeleton. Ann Otol Rhinol Laryngol. 1987. 96: 618-9
4. Candy EJ, Miller NR, Carson BS. Myxoma of bone involving the orbit. Arch Ophthalmol. 1991. 109: 919-20
5. Court-Payen M, Ingemann Jensen L, Bjerregaard B, Schwarz Lausten G, Skjoldbye B. Intramuscular myxoma and fibrous dysplasia of bone--mazabraud’s syndrome. A case report. Acta Radiol. 1997. 38: 368-71
6. Craig NM, Putterman AM, Roenigk RK, Wang TD, Roenigk HH. Multiple periorbital cutaneous myxomas progressing to scleromyxedema. J Am Acad Dermatol. 1996. 34: 928-30
7. DeFatta RJ, Verret DJ, Ducic Y, Carrick K. Giant myxomas of the maxillofacial skeleton and skull base. Otolaryngol Head Neck Surg. 2006. 134: 931-5
8. Hansen TS, Danielsson LI, Fast S, Thygesen TH. Odontogenic myxoma involving the orbit in a 3-year-old boy: Removal, reconstruction and review of the literature. BMJ Case Rep. 2016. 2016: bcr2015212465-
9. Hidayat AA, Flint A, Marentette L, Torczynski E, Al-Qahtani JM, Ahl NC. Myxomas and angiomyxomas of the orbit: A clinicopathologic study of 6 cases. Ophthalmology. 2007. 114: 1012-9
10. Jakobiec FA, Callahan AB, Stagner AM, Lee NG, Rashid A, Mendoza P. Malignant rhabdoid transformation of a longstanding, aggressive, and recurrent orbital angiomyxoma. Surv Ophthalmol. 2015. 60: 166-76
11. Kumar SR. Myriad manifestations of myxoma. J Thorac Cardiovasc Surg. 2017. 154: 1383-4
12. Large ND, Niebel HH, Fredricks WH. Myxoma of the jaw: Report of two cases. Oral Surg Oral Med Oral Pathol. 1960. 13: 1462-8
13. Lieb WE, Goebel HH, Wallenfang T. Myxoma of the orbit: A clinicopathologic report. Graefes Arch Clin Exp Ophthalmol. 1990. 228: 28-32
14. Lo Muzio L, Nocini P, Favia G, Procaccini M, Mignogna MD. Odontogenic myxoma of the jaws: A clinical, radiologic, immunohistochemical, and ultrastructural study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996. 82: 426-33
15. Maiuri F, Corriero G, Galicchio B, Angrisani P, Bonavolontà G. Myxoma of the skull and orbit. Neurochirurgia (Stuttg). 1988. 31: 136-8
16. Manjandavida FP, Chahar S, Dave B. Isolated intraosseous extra-gnathic orbital myxoma: A clinicopathologic case report. Orbit. 2019. 38: 401-6
17. Maria DL, Marwa V. Myxoma of the orbit. J All India Ophthalmol Soc. 1967. 15: 75-6
18. Mishulin A, Lever JF, Porter W, Servat JJ, Gladstone G, Black E. Aggressive glabellar angiomyxoma with orbital extension. Orbit. 2012. 31: 361-3
19. Mupas-Uy J, Kitaguchi Y, Takahashi Y, Takahashi E, Kakizaki H. Orbital myxoma comorbid with acute myelomonocytic leukemia. Orbit. 2017. 36: 465-7
20. Pahl S, Henn W, Binger T, Stein U, Remberger K. Malignant odontogenic myxoma of the maxilla: Case with cytogenetic confirmation. J Laryngol Otol. 2000. 114: 533-5
21. Parikh D, Mukherjee B. Lacrimal gland myxoma. Indian J Ophthalmol. 2017. 65: 887-9
22. Petscavage-Thomas JM, Walker EA, Logie CI, Clarke LE, Duryea DM, Murphey MD. Soft-tissue myxomatous lesions: Review of salient imaging features with pathologic comparison. Radiographics. 2014. 34: 964-80
23. Rambhatla S, Subramanian N, Gangadhara Sundar JK, Krishnakumar S, Biswas J. Myxoma of the orbit. Indian J Ophthalmol. 2003. 51: 85-7
24. Rodríguez-Uña I, Troyano-Rivas JA, González-García C, Chícharo-de-Freitas R, Ortiz-Zapata JJ, Ortega-Medina L. Orbital nerve seath myxoma with extraocular muscle involvement: A rare case. Semin Ophthalmol. 2015. 30: 316-20
25. Sánchez-Orgaz M, Grabowska A, Arbizu-Duralde A, Romero-Martín R, Patrón M, Diéguez E. Orbital nerve sheath myxoma: A case report. Ophthalmic Plast Reconstr Surg. 2011. 27: e106-8
26. Stout AP. Myxoma, the tumor of primitive mesenchyme. Ann Surg. 1948. 127: 706-19
27. Tawfik HA, Elraey HZ. Orbital myxoma: A case report. Orbit. 2013. 32: 200-2
28. Ting SL, Koay CL, Ngo CT, Chieng LL, Chua CN. Orbital myxoma--an unusual cause of inferoorbital mass. Med J Malaysia. 2010. 65: 224-6
29. Yin H, Cai BW, An HM, You C. Huge primary myxoma of skull base: A report of an uncommon case. Acta Neurochir (Wien). 2007. 149: 713-7
30. Zimmerman DC, Dahlin DC. Myxomatous tumors of the jaws. Oral Surg Oral Med Oral Pathol. 1958. 11: 1069-80
31. Zubilewicz A, Dolar-Szczasny J, Rakowska E, Mackiewicz J. Optical coherence tomography in monitoring of choroidal folds after surgical excision of ethmoidal myxoma. Klin Oczna. 2013. 115: 141-3