- Department of Neurosurgery Baylor College of Medicine, Houston, Texas, United States.
- Department of Opthalmology, Baylor College of Medicine, Houston, Texas, United States.
Correspondence Address:
Akash J. Patel, Department of Neurosurgery, Baylor College of Medicine, Houston, Texas, United States.
DOI:10.25259/SNI_498_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Eric A. Goethe1, Juliet Hartford2, Rod Foroozan2, Akash J. Patel1. Oscillopsia following orbitotomy for intracranial tumor resection. 13-Sep-2021;12:459
How to cite this URL: Eric A. Goethe1, Juliet Hartford2, Rod Foroozan2, Akash J. Patel1. Oscillopsia following orbitotomy for intracranial tumor resection. 13-Sep-2021;12:459. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11114
Abstract
Background: Oscillopsia is a visual phenomenon in which an individual perceives that their environment is moving when it is in fact stationary. In this report, we describe two patients with pulsatile oscillopsia following orbitocranial approaches for skull base meningioma resection.
Case Description: Two patients, both 42-year-old women, underwent orbitocranial approaches for resection of a right sphenoid wing (Patient 1) and left cavernous sinus (Patient 2) meningioma. Patient 1 underwent uncomplicated resection and was discharged home without neurologic or visual complaints; she presented 8 days later with pulsatile oscillopsia. This was managed expectantly, and MRA revealed no evidence of vascular pathology. She has not required intervention as of most recent follow-up. Patient 2 developed trochlear and trigeminal nerve palsies following resection and developed pulsatile oscillopsia 4 months postoperatively. After patching and corrective lens application, the patient’s symptoms had improved by 26 months postoperatively.
Conclusion: Oscillopsia is a potential complication following skull base tumor resection about which patients should be aware. Patients may improve with conservative management alone, although the literature describes repair of orbital defects for ocular pulsations in traumatic and with some developmental conditions.
Keywords: Meningioma, Orbital osteotomy, Orbitocranial, Orbitopterional, Oscillopsia, Skull base tumors
INTRODUCTION
Oscillopsia is a visual phenomenon in which an individual perceives that the stationary environment is moving.[
CASE DESCRIPTIONS
Patient #1
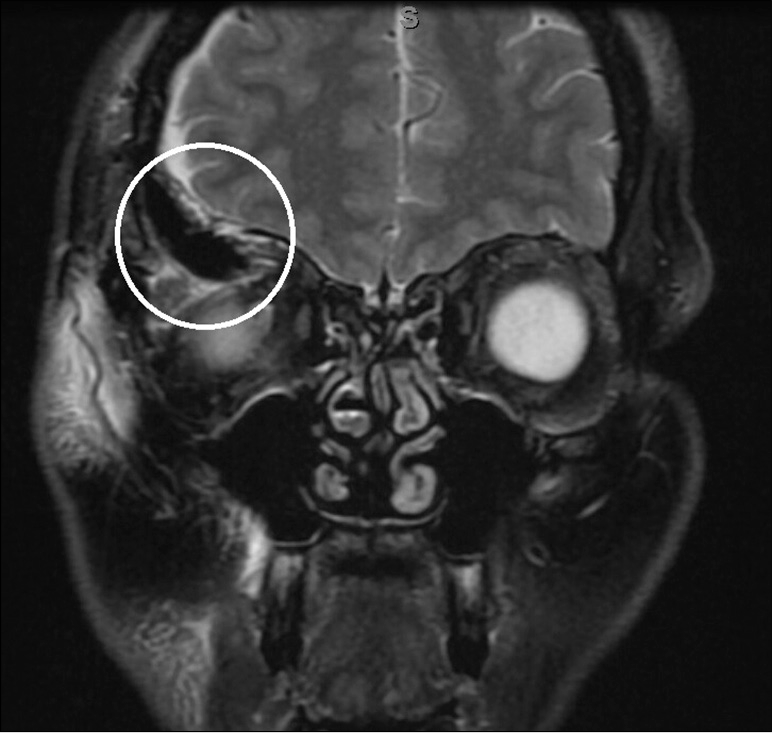
A 42-year-old woman with no significant medical history presented to an outside facility with progressive right eye proptosis and diplopia on the left gaze over 2 years. An MRI demonstrated a right sphenoid wing mass with extension into the temporalis muscle and orbit. She was found to have normal visual acuity, no evidence of optic neuropathy, restricted right ocular motility, and proptosis on the right of 5 mm compared to her left eye. She was fully oriented with intact cranial nerves, normal ocular alignment, motor, and sensory function throughout. Gait was normal. She underwent a right orbitocranial approach for resection of the mass, requiring complete removal of the greater wing of the sphenoid and the lesser wing lateral to the anterior clinoid process. Her postoperative course was unremarkable and she was discharged home on postoperative day 4. Postoperative MRI demonstrated gross total resection of the mass and a superior orbital wall defect [
Patient #2
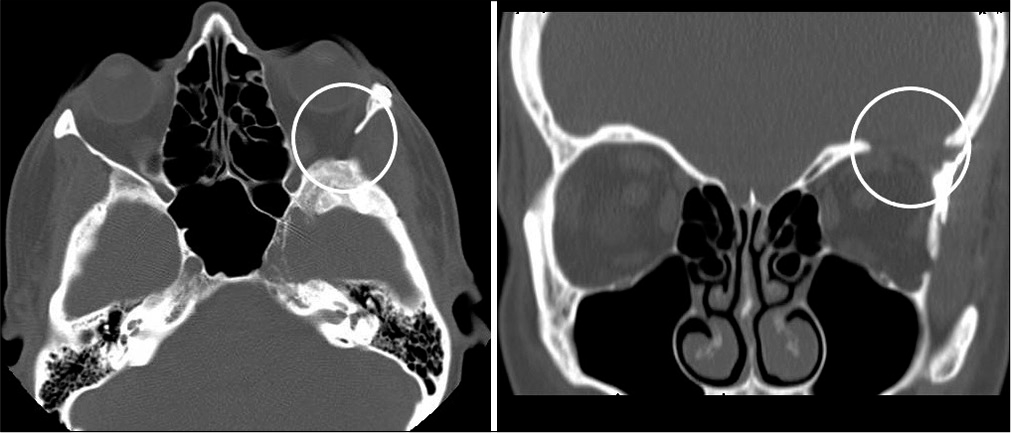
A 42-year-old woman with hypothyroidism presented to our clinic with several months of lip and tongue tingling. MRI revealed an anterior skull base meningioma with extension into the left cavernous sinus. She did not undergo ophthalmologic evaluation preoperatively, as she did not have any visual complaints. She underwent a left one-piece orbitopterional craniotomy with complete removal of the sphenoid wing and lateral orbital wall and partial resection of the superior orbital wall and was brought thereafter to the Neuro ICU, where she was found to have a left trochlear nerve palsy, resulting in double vision, and hypoesthesia in CN V2-V3 distribution. Her postoperative course was complicated by seizures, requiring treatment with levetiracetam for 6 months. She was discharged home on postoperative day 4. At her initial postoperative visit, her diplopia had improved, and on ophthalmologic evaluation 4 months later, she was found to have oscillopsia related to orbital pulsations synchronous with her cardiac cycle [
Video 1
DISCUSSION
Orbitocranial approaches are a critical part of the armamentarium for skull base surgeons to provide access to lesions involving the parasellar region, cavernous sinus, anterior and middle fossa floors, and the orbital apex. These approaches can be tailored to the lesion through various modifications, including the one-piece, two-piece, and supraorbital variations.[
While oscillopsia is often observed in patients with vestibular damage, the primary mechanism of retinal slip in our patients is a mechanical oscillopsia for which the vestibulo-ocular reflex cannot compensate.[
One of the patients in our study had spontaneous resolution of her oscillopsia. A similar course was observed by Fayers et al. following lateral orbital decompression.[
The extent of bony work is an important consideration in orbital osteotomy. It is generally accepted that at least a third of the orbital roof and lateral wall should be preserved to avoid postoperative pulsatile enophthalmos.[
While considered unnecessary by some authors, the practice of intraoperative orbital reconstruction to avoid postoperative enophthalmos and oscillopsia and to minimize cosmetic defects in patients with sphenoid wing or spheno-orbital meningioma has been described and is associated with good outcomes.[
CONCLUSION
Oscillopsia is the visual perception of movement of a stationary visual field; it may occur due to vestibular dysfunction, neurovascular compression, or mechanical pressure on the orbit itself. Pulsatile oscillopsia is a rare, but debilitating complication following orbital osteotomy for intracranial mass resection. This should be taken into consideration when deciding whether or not to remove the orbit. If orbital osteotomy is necessary, then patients should be counseled appropriately. While symptoms may resolve spontaneously, reconstruction of orbital defects during tumor resection may help prevent the development of this condition.
DECLARATIONS
Ethics approval and consent to participate
No ethics committee approval for this retrospective study.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during this study.
Authors’ contributions
Dr. Goethe primarily drafted the article and obtained data from patient records. Drs. Hartford and Foroozan helped critically revise the article. Dr. Patel critically revised the article, supervised its submission, and approved the final draft.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
DECLARATIONS
Ethics approval and consent to participate
No ethics committee approval for this retrospective study.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during this study.
Authors’ contributions
Dr. Goethe primarily drafted the article and obtained data from patient records. Drs. Hartford and Foroozan helped critically revise the article. Dr. Patel critically revised the article, supervised its submission, and approved the final draft.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
www.surgicalneurologyint.com
References
1. Aziz KM, Froelich SC, Cohen PL, Sanan A, Keller JT, van Loveren HR. The one-piece orbitozygomatic approach: The maccarty burr hole and the inferior orbital fissure as keys to technique and application. Acta Neurochir (Wien). 2002. 144: 15-24
2. Bronstein AM.editors. Oscillopsia: Editorial review. Curr Opin Neurol. 2005. 18: 1-3
3. Cheng CM, Chang CF, Ma HI, Chiang YH, McMenomey SO, Delashaw JB. Modified orbitozygomatic craniotomy for large medial sphenoid wing meningiomas. J Clin Neurosci. 2009. 16: 1157-60
4. Demonte F, Tabrizi P, Culpepper SA, Suki D, Soparkar CN, Patrinely JR. Ophthalmological outcome after orbital entry during anterior and anterolateral skull base surgery. J Neurosurg. 2002. 97: 851-6
5. Emerick GT, Shields CL, Shields JA, Eagle RC, de Potter P, Markowitz GI. Chewing-induced visual impairment from a dumbbell dermoid cyst. Ophthalmic Plast Reconstr Surg. 1997. 13: 57-61
6. Fayers T, Barker LE, Verity DH, Rose GE. Oscillopsia after lateral wall orbital decompression. Ophthalmology. 2013. 120: 1920-3
7. Ha AY, Mangham W, Frommer SA, Choi D, Klinge P, Taylor HO. Interdisciplinary management of minimally displaced orbital roof fractures: Delayed pulsatile exophthalmos and orbital encephalocele. Craniomaxillofac Trauma Reconstr. 2017. 10: 11-5
8. Jung SH, Ferrer AD, Vela JS, Granados FA. Spheno-orbital meningioma resection and reconstruction: The role of piezosurgery and premolded titanium mesh. Craniomaxillofac Trauma Reconstr. 2011. 4: 193-200
9. Leake D, Gunnlaugsson C, Urban J, Marentette L. Reconstruction after resection of sphenoid wing meningiomas. Arch Facial Plast Surg. 2005. 7: 99-103
10. Lemole GM, Henn JS, Zabramski JM, Spetzler RF. Modifications to the orbitozygomatic approach: Technical note. J Neurosurg. 2003. 99: 924-30
11. López-Elizalde R, Robledo-Moreno E, O’Shea-Cuevas G, Matute-Villaseñor E, Campero Á, Godínez-Rubí M. Modified orbitozygomatic approach without orbital roof removal for middle fossa lesions. J Korean Neurosurg Soc. 2018. 61: 407-14
12. Lotfy M, Xu R, McGirt M, Sakr S, Ayoub B, Bydon A. Reconstruction of skull base defects in sphenoid wing dysplasia associated with neurofibromatosis I with titanium mesh. Clin Neurol Neurosurg. 2010. 112: 909-14
13. Mettu P, Bhatti MT, El-Dairi M, Price EB, Lin AY, Alaraj A. Orbito-masticatory syndrome. J Neuroophthalmol. 2016. 36: 308-12
14. Nguyen CT, Guiney AJ, Iseli TA, King JA, Hardy TG. Spontaneous giant pseudomeningocele in the middle cranial fossa as a cause of pulsatile proptosis. Ophthalmic Plast Reconstr Surg. 2017. 33: S91-2
15. Niu J, Wang J, Wang D, He X, Li Z, Li X. Clinical, radiological features and surgical strategies for 23 NF1 patients with intraorbital meningoencephalocele. Neurol Sci. 2019. 40: 1217-25
16. Pace ST, Koreen IV, Wilson JA, Yeatts RP. Orbital reconstruction via deformable titanium mesh following spheno-orbital meningioma resection: Ophthalmic presentation and outcomes. Ophthalmic Plast Reconstr Surg. 2020. 36: 89-93
17. Porrúa-Tubío L, Sales-Sanz A, de-Arriba-Palomero P, Felix-Espinar B, de-Arriba-Palomero F, Alonso-Formento N. Oscillopsia after isolated lateral wall decompression versus balanced or 3-wall decompression. Ophthalmic Plast Reconstr Surg. 2021. 37: 141-4
18. Prathibha S, Parasar V, Yasmin S, Pramila VV. A multidisciplinary approach to sphenoid wing dysplasia presenting with pulsatile proptosis in neurofibromatosis Type 1: A rare case report. Indian J Ophthalmol. 2018. 66: 157-60
19. Pritz MB, Burgett RA. Spheno-orbital reconstruction after meningioma resection. Skull Base. 2009. 19: 163-70
20. Saito A, Kon H, Haryu S, Mino M, Sasaki T, Nishijima M. Arachnoid cyst in the middle cranial fossa presenting with pulsatile exophthalmos: Case report and literature review. Neurol Med Chir (Tokyo). 2014. 54: 563-6
21. Seçkin H, Avci E, Uluç K, Niemann D, Başkaya MK. The work horse of skull base surgery: Orbitozygomatic approach. Technique modifications, and applications. Neurosurg Focus. 2008. 25: E4
22. Sekhar LN, Kalia KK, Yonas H, Wright DC, Ching H. Cranial base approaches to intracranial aneurysms in the subarachnoid space. Neurosurgery. 1994. 35: 472-83
23. Straube A, Bronstein A, Straumann D. Nystagmus and oscillopsia. Eur J Neurol. 2012. 19: 6-14
24. Taguchi Y, Tanaka K, Matsuzawa M, Sekino H. A surgical technique to avoid postoperative enophthalmos in the cranioorbital approach: Technical note. J Neurosurg. 1996. 85: 514-7
25. Talacchi A, de Carlo A, D’Agostino A, Nocini P. Surgical management of ocular symptoms in spheno-orbital meningiomas. Is orbital reconstruction really necessary? Neurosurg Rev 2014. ;. 37: 301-10
26. Tilikete C, Vighetto A. Oscillopsia: Causes and management. Curr Opin Neurol. 2011. 24: 38-43