Ossifying fibroma of the ethmoid and sphenoid sinuses: A report of a rare case and literature review
- Department of Neurosurgery, Cairo University, Cairo, Egypt.
Correspondence Address:
Mohammed A. Azab, Department of Neurosurgery, Cairo University, Cairo, Egypt.
DOI:10.25259/SNI_182_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammed A. Azab. Ossifying fibroma of the ethmoid and sphenoid sinuses: A report of a rare case and literature review. 09-Feb-2024;15:38
How to cite this URL: Mohammed A. Azab. Ossifying fibroma of the ethmoid and sphenoid sinuses: A report of a rare case and literature review. 09-Feb-2024;15:38. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12737
Abstract
Background: Fibro-osseous lesions include a variety of bone lesions with different clinical and histopathological features.
Case Description: We report a case of cemento-ossifying lesion involving the left ethmoid and sphenoid sinus in a 17-year-old male patient. Computed tomography showed an expansile hyperdense lesion with sclerosed peripheral mantle epicentered on the left ethmoid and sphenoid sinus and extending into the left nasal cavity. Magnetic resonance imaging was done for preoperative planning. Transnasal endoscopic resection was performed and histopathological examination confirmed the diagnosis of ossifying fibroma (OF).
Conclusion: Involvement of the ethmoid sinus with OF is a rare condition; therefore, we examined the literature for similar cases to highlight the possible clinical presentation and management. Endoscopic management is a safe, effective approach with a low rate of complications.
Keywords: Endoscopic management, Ethmoid, Fibro-osseous, Ossifying fibroma, Proptosis
INTRODUCTION
Fibro-osseous lesions represent a variety of proliferative bone diseases, with each type representing a specific biological and morphological pattern. In these lesions, the normal bone is replaced by fibroblasts and they can be classified into dysplasia or bone tumors.[
In this article, we report a case of juvenile OF involving the sphenoid and ethmoid sinuses and review the literature to expose the clinical and radiologic features of this lesion. It is crucial for a skull base surgeon to differentiate between OF and the other osseous lesions.
Methods
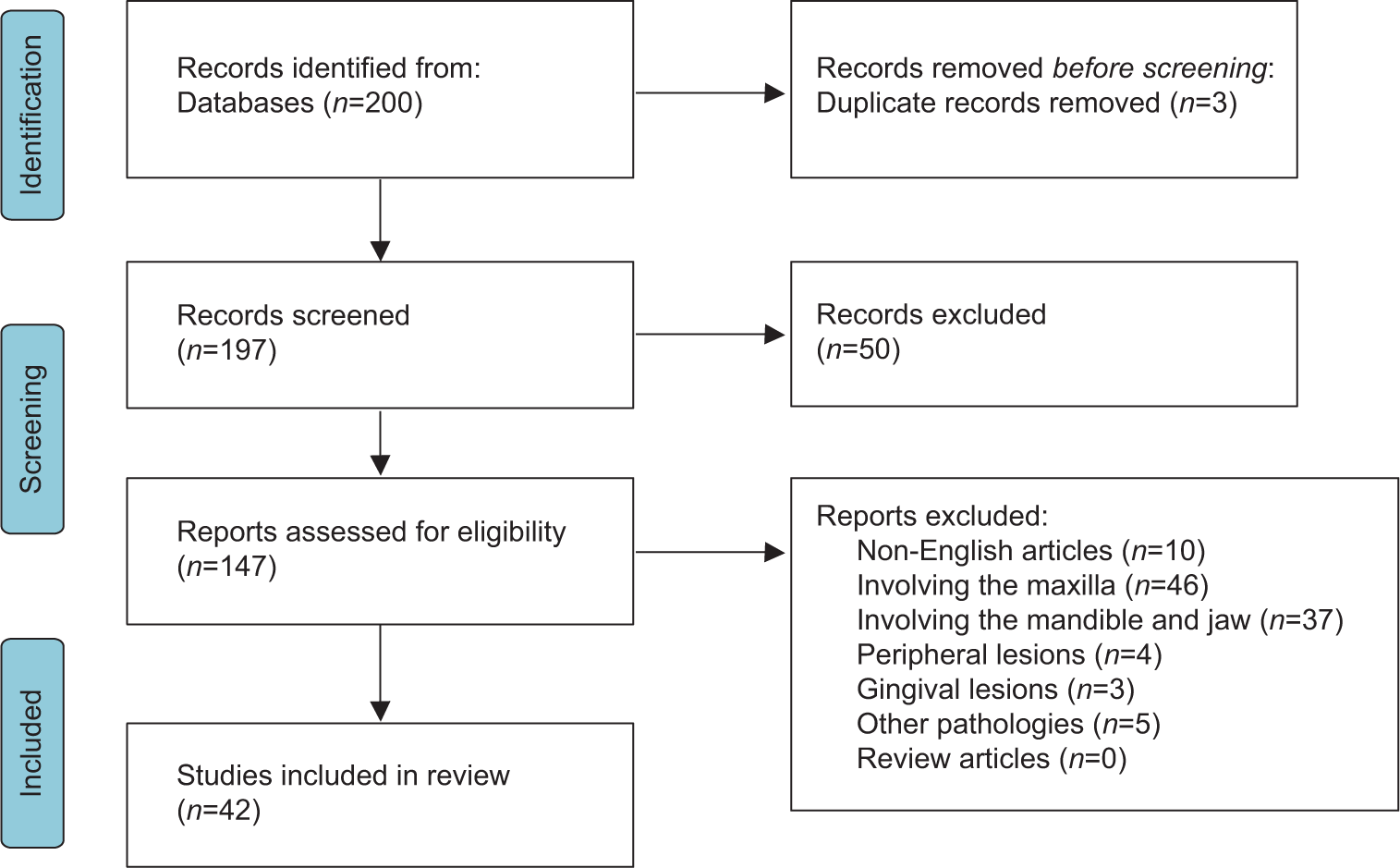
This review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement and PRISMA checklist [
CASE DESCRIPTION
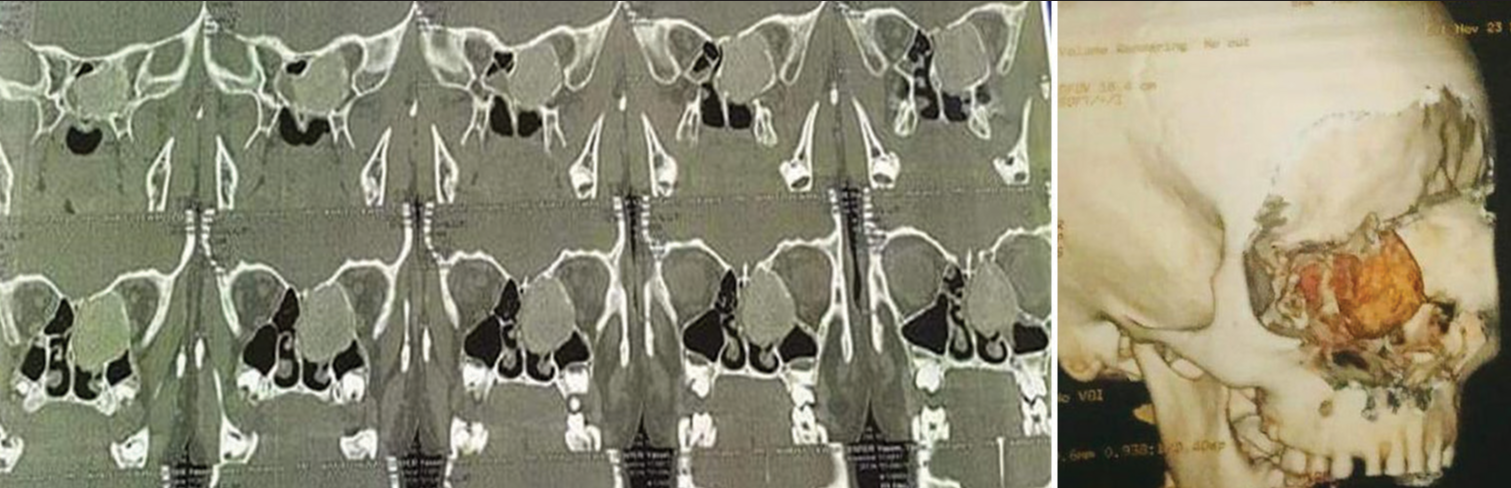
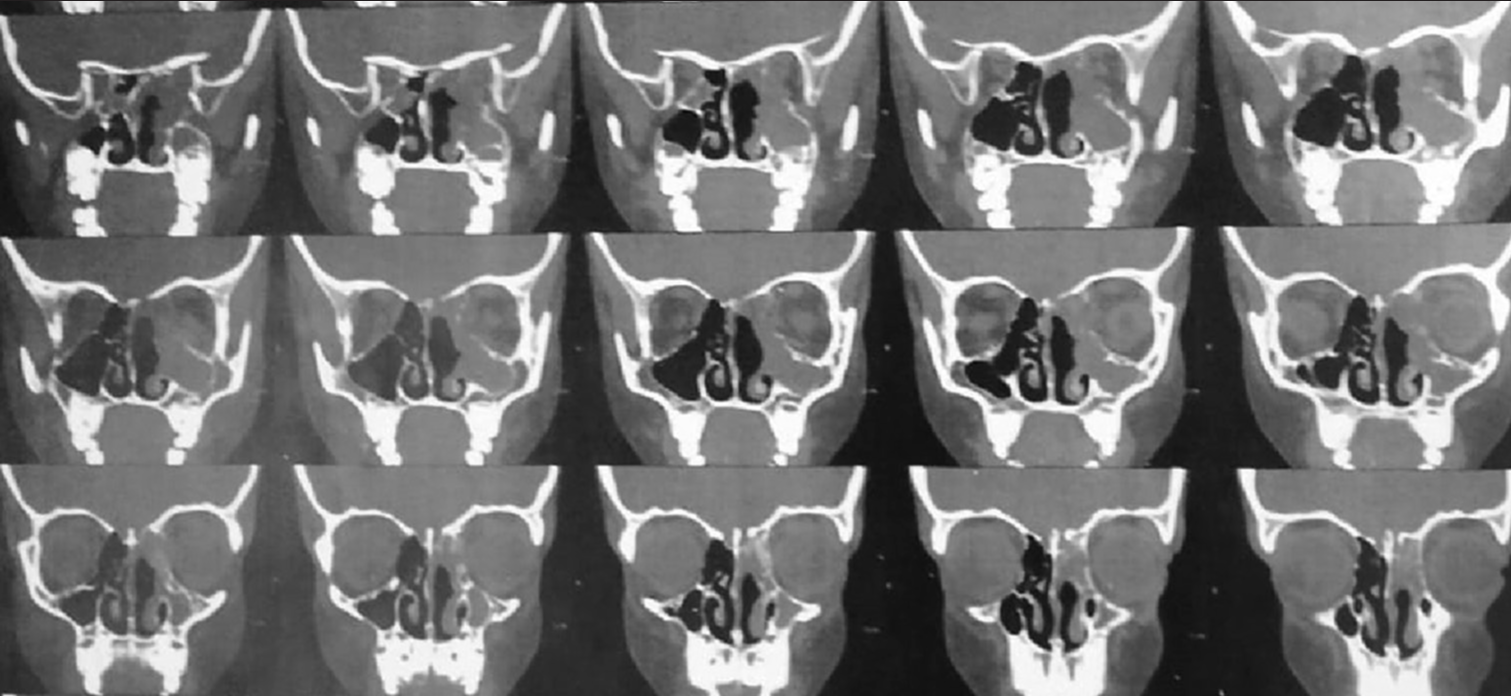
A 17-year-old male patient was referred to the otorhinolaryngology outpatient clinic with symptoms suggestive of recurrent nasal obstruction over eight months. He also complained of 1 year of progressive left eye proptosis. There was no history of epistaxis, anosmia, or trauma to the face. On examination, a polypoid irregular mass filling the left posterior nasal cavity was observed. It was a whitish mass, and when palpated by the forceps, it had a semisolid consistency. There were no other remarkable findings on general examination. Computed tomography (CT), in
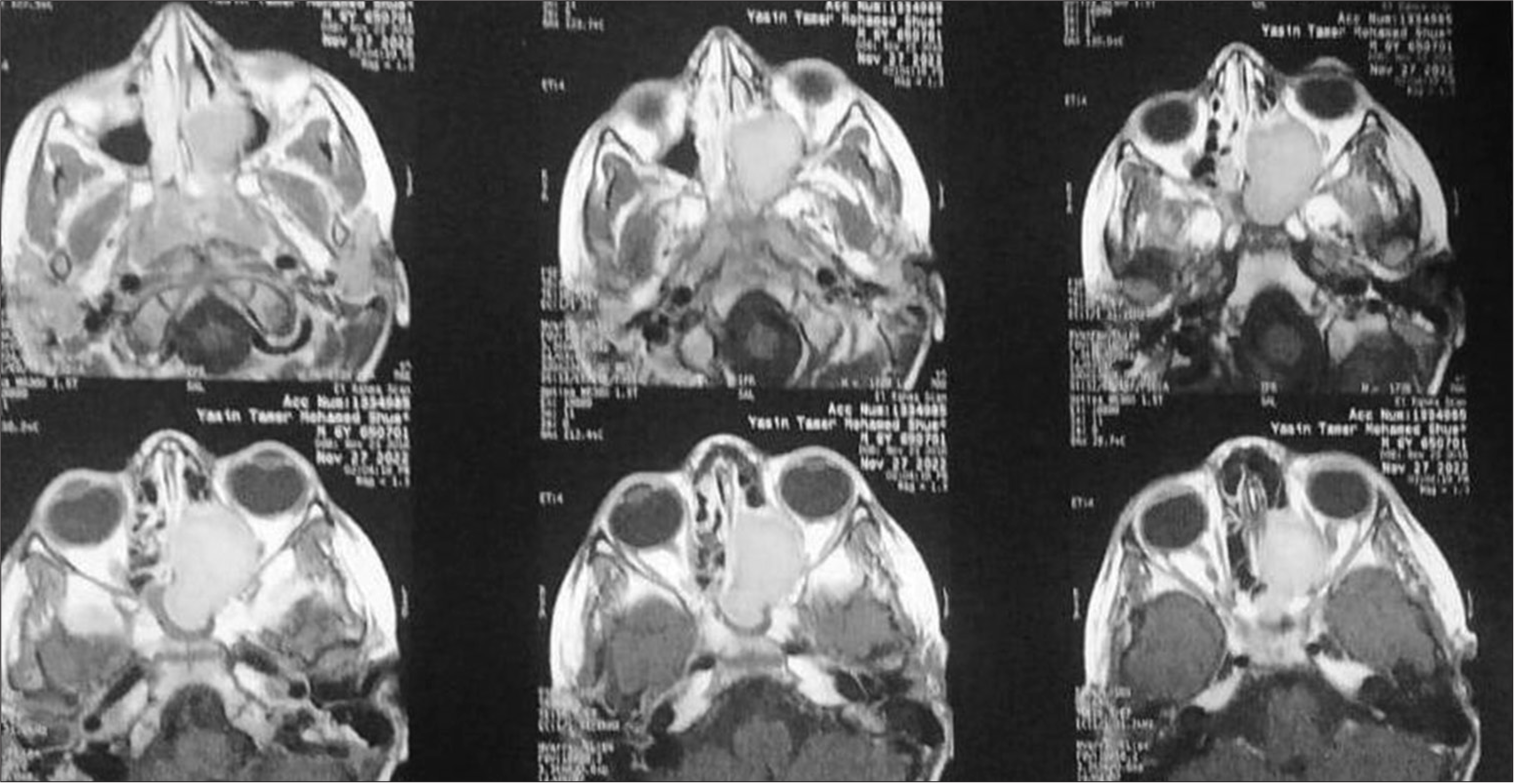
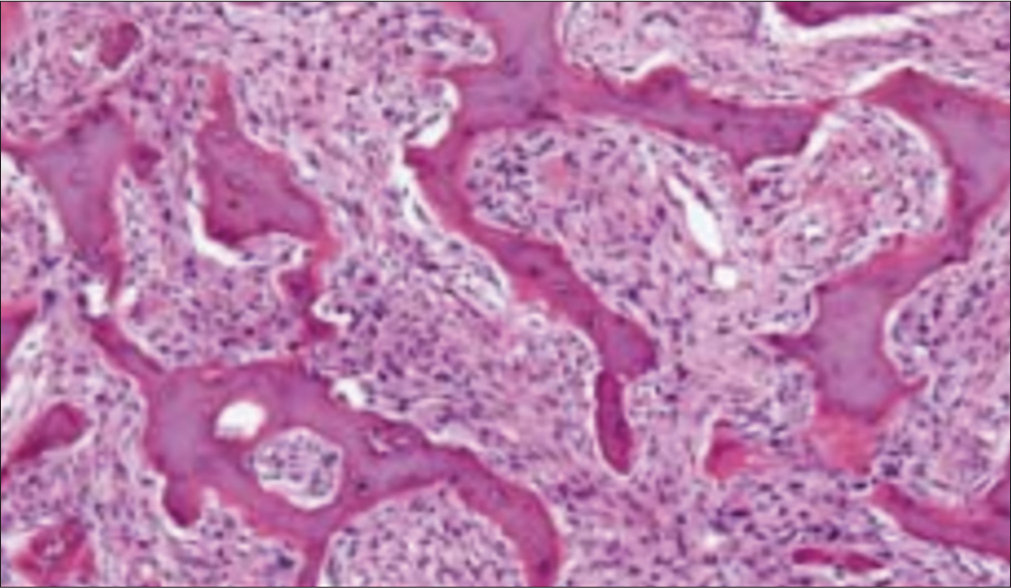
The optic nerve displayed a normal signal intensity. The patient was prepared for surgery. The patient was operated on in a supine position under general hypotensive anesthesia. We performed a left ethmoidosphenoidectomy under general anesthesia using an endoscope. The nasal cavity was decongested with 1:10,000 adrenaline-soaked cotton pledgets. The 30° endoscope was introduced in the left nasal cavity. The bulla ethmoidalis is encountered medially and penetrated using the powered debrider. The lamina papyracea was identified laterally, and we tried to preserve its mucosa. We continued dissection posteriorly until we identified the basal lamella and the posterior ethmoid cells. Complete dissection of the ethmoid cells was done under the guidance of a 45° endoscope. The lesion was excised in a piecemeal fashion. The mucosa in the sphenoid sinus was polypoidal and congested due to recurrent inflammation and obstruction. Routine postoperative endoscopic examination of the left sinonasal cavity was performed, and no evidence of cerebrospinal fluid leaks was present. Histopathological examination revealed the proliferation of stromal spindle fibroblasts presence with woven and lamellar bone deposits composed of scattered osteoblasts and osteocytes [
RESULTS
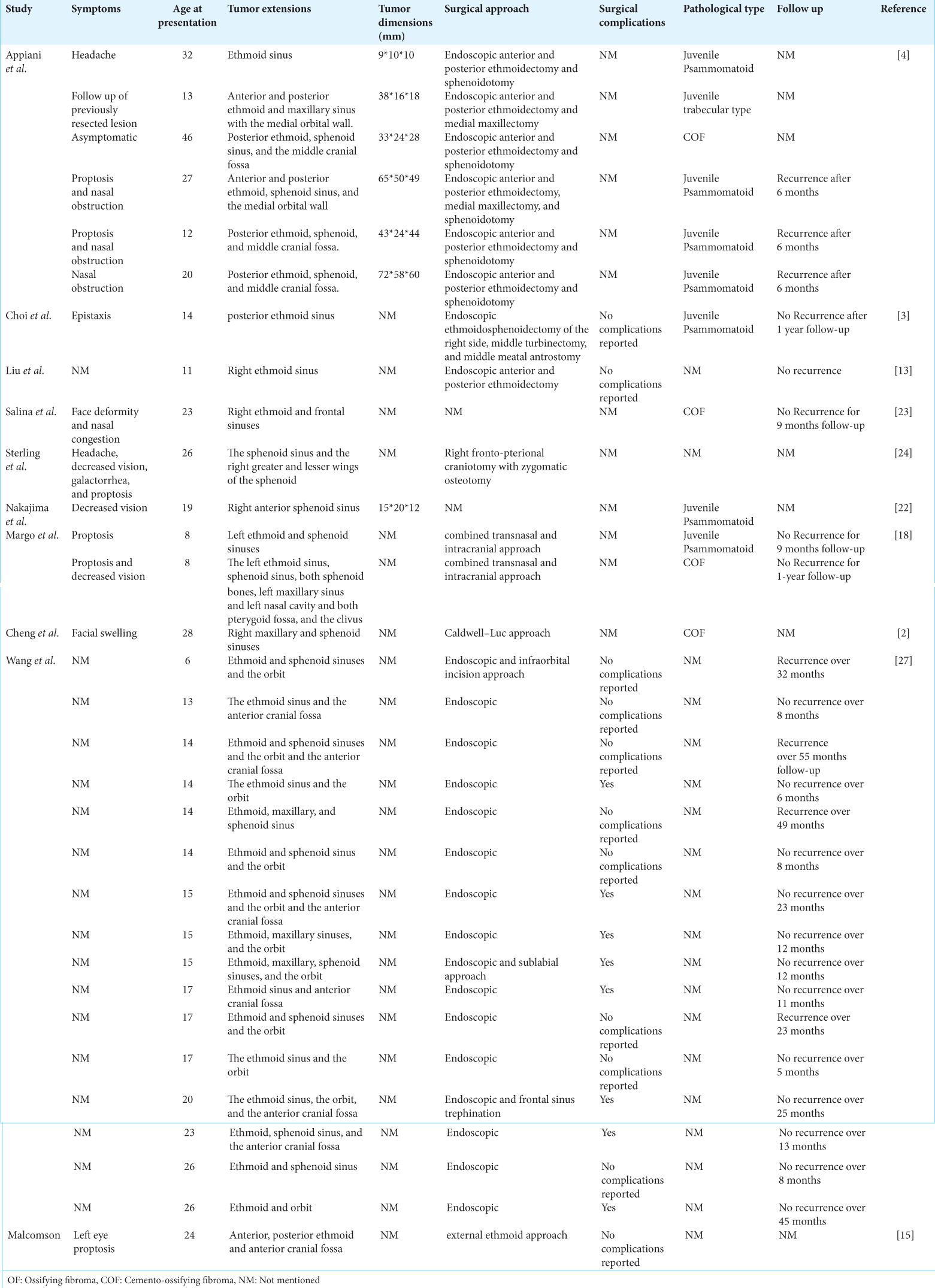
A total of 200 articles were identified from different databases. About 197 records were screened for different inclusion and exclusion criteria. About 50 reports were excluded due to different reasons such as non-English language, different pathologies, or OF involving locations other than the ethmoid and sphenoid sinus. The clinical presentations, pathological types, and surgical management approaches were reviewed. The PRISMA flow chart for screening and selection of articles is shown in
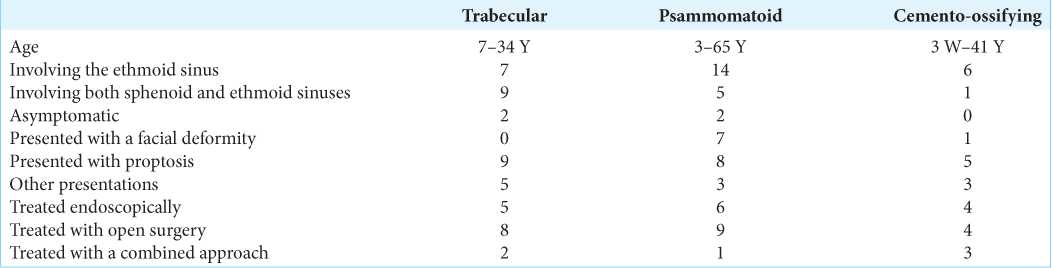
The age of the patients ranged from 3 months to 65 years. Males were more affected than females, and they tended to be younger at presentation. About 60% of male patients presented with OF under the age of 30 years. The patients presented with symptoms related to the expansion of the mass, namely, proptosis, nasal obstruction, headache, facial masses, and deformities. Proptosis was the most common presentation in all types of OF involving the ethmoid and sphenoid sinuses. The asymptomatic presentation was reported only in four cases [
DISCUSSION
Manes, in 1872, was the first to identify OF as a rare benign osseous lesion.[
There are three histological variants with different biological behaviors, including COF, juvenile psammomatoid OF (JPOF), and JTOF.[
Clinical presentations of OF are variable, and they differ according to the location. OF may be asymptomatic for a long time. Patients may present with a painless facial swelling, which may reside for several years.[
These lesions are diagnosed with CT, and MRI is used for preoperative surgical planning. OF usually appears as a well-defined lesion. The density of fibrous and osseous tissues is the major determinant of the radiological appearance of these lesions. In the advanced stages of OF, the center is filled with mature bone tissues, while in the earlier stages, the center is usually soft and fibrous.[
There is no general consensus about the management strategy for OF, and it differs according to the location of the lesion and the rate of growth. The treatment of choice is complete surgical resection, while conservative management is tried in asymptomatic cases.[
CONCLUSION
OF is an uncommon benign tumor that should be considered in the differential diagnosis of sinonasal obstructive lesions. In the present study, we report a rare case of OF involving the sphenoid and ethmoid sinuses that were treated endoscopically with complete resolution of the symptoms. Endoscopic management is a safe, effective approach with a low rate of complications.
Ethical approval
The research/study was approved by the Institutional Review Board at Cairo University Hospital, number CU1245, dated January 10, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cansiz H, Tuskan K, Karaman E, Dervisoğlu S. Endoscope assisted removal of cementoossifying fibroma in the paranasal sinuses in a five-year-old girl. Int J Pediatr Otorhinolaryngol. 2004. 68: 489-93
2. Cheng C, Takahashi H, Yao K, Nakayama M, Makoshi T, Nagai H. Cemento-ossifying fibroma of maxillary and sphenoid sinuses: Case report and literature review. Acta Otolaryngol Suppl. 2002. 547: 118-22
3. Choi YC, Jeon EJ, Park YS. Ossifying fibroma arising in the right ethmoid sinus and nasal cavity. Int J Pediatr Otorhinolaryngol. 2000. 54: 159-62
4. Ciniglio Appiani M, Verillaud B, Bresson D, Sauvaget E, Blancal JP, Guichard JP. Ossifying fibromas of the paranasal sinuses: Diagnosis and management. Acta Otorhinolaryngol Ital. 2015. 35: 355-61
5. El-Mofty S. Psammomatoid and trabecular juvenile ossifying fibroma of the craniofacial skeleton: Two distinct clinicopathologic entities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 93: 296-304
6. El-Mofty SK, Nelson B, Toyosawa S, El-Naggar AK, Chan JK, Grandis JR, editors. Ossifying fibroma. World Health Organization classification head and neck tumours. Lyon: IARC; 2017. p.
7. Hakeem AH, Hakeem IH. Juvenile ossifying fibroma of paranasal sinuses-do we need to be radical in surgery?. J Craniofac Surg. 2013. 24: e257-8
8. Han MH, Chang KH, Lee CH, Seo JW, Han MC, Kim CW. Sinonasal psammomatoid ossifying fibromas: CT and MR manifestations. AJNR Am J Neuroradiol. 1991. 12: 25-30
9. Johnson LC, Yousefi M, Vinh TN, Heffner DK, Hyams VJ, Hartman KS. Juvenile active ossifying fibroma. Its nature, dynamics and origin. Acta Otolaryngol Suppl. 1991. 488: 1-40
10. Katti G, Khan MM, Chaubey SS, Amena M. Cemento-ossifying fibroma of the jaw. BMJ Case Rep. 2016. 2016: bcr2015214327
11. Kendi AT, Kara S, Altinok D, Keskil S. Sinonasal ossifying fibroma with fluid-fluid levels on MR images. AJNR Am J Neuroradiol. 2003. 24: 1639-41
12. Ledderose GJ Stelter K, Becker S, Leunig A. Paranasal ossifying fibroma: Endoscopic resection or wait and scan?. Eur Arch Otorhinolaryngol. 2011. 268: 999-1004
13. Liu JJ, Thompson LD, Janisiewicz AM, Shibuya TY, Keschner DB, Garg R. Ossifying fibroma of the maxilla and sinonasal tract: Case series. Allergy Rhinol (Providence). 2017. 8: 32-6
14. Ma J, Zhou B, Cui S, Huang Q, Yang Z, Wang G. Resection of the ossifying fibroma of paranasal sinuses and anterior skull base with nasal endoscope under the guidance of image navigation. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2010. 24: 918-20 927
15. Malcomson KG. Ossifying fibroma of the sphenoid. J Laryngol Otol. 1967. 81: 87-92
16. Manes RP, Ryan MW, Batra PS, Mendelsohn D, Fang YV, Marple BF. Ossifying fibroma of the nose and paranasal sinuses. Int Forum Allergy Rhinol. 2013. 3: 161-8
17. Margo CE, Ragsdale BD, Perman KI, Zimmerman LE, Sweet DE. Psammomatoid (juvenile) ossifying fibroma of the orbit. Ophthalmology. 1985. 92: 150-9
18. Margo CE, Weiss A, Habal MB. Psammomatoid ossifying fibroma. Arch Ophthalmol. 1986. 104: 1347-51
19. Marvel JB, Marsh MA, Catlin FI. Ossifying fibroma of the mid-face and paranasal sinuses: Diagnostic and therapeutic considerations. Otolaryngol Head Neck Surg. 1991. 104: 803-8
20. McCollister KB, Hopper BD, Michel MA. Sinonasal neoplasms: Update on classification, imaging features, and management. Appl Radiol. 2015. 44: 7-15
21. Mohsenifar Z, Nouhi S, Abbas FM, Farhadi S, Abedin B. Ossifying fibroma of the ethmoid sinus: Report of a rare case and review of literature. J Res Med Sci. 2011. 16: 841-7
22. Nakajima R, Saito N, Uchino A, Kuji I, Suzuki T, Nishikawa R. Juvenile psammomatoid ossifying fibroma with visual disturbance: A case report with imaging features. J Neuroimaging. 2013. 23: 137-40
23. Salina AC, de Souza PM, da Costa Gadelha CM, Aguiar LB, de Castro JD, Barreto AR. Ossifying fibroma: An uncommon differential diagnosis for T2-hypointense sinonasal masses. Radiol Case Rep. 2017. 12: 313-7
24. Sterling KM, Stollman A, Sacher M, Som PM. Ossifying fibroma of sphenoid bone with coexistent mucocele: CT and MRI. J Comput Assist Tomogr. 1993. 17: 492-4
25. Suarez-Soto A, de la Hermosa MC, Minguez-Martinez I, Floría-García LM, Barea-Gámiz J, Delhom-Valero J. Management of fibro-osseous lesions of the craniofacial area. Presentation of 19 cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2013. 18: 479-85
26. Walter JM, Terry BC, Small EW, Matteson SR, Howell RM. Aggressive ossifying fibroma of the maxilla: Review of the literature and report of cases. J Oral Surg. 1979. 37: 276-86
27. Wang H, Sun X, Liu Q, Wang J, Wang D. Endoscopic resection of sinonasal ossifying fibroma: 31 cases report at an institution. Eur Arch Otorhinolaryngol. 2014. 271: 2975-82
28. Williams HK, Mangham C, Speight PM. Juvenile ossifying fibroma. An analysis of eight cases and a comparison with other fibro-osseous lesions. J Oral Pathol Med. 2000. 29: 13-8
29. Wilson M, Snyderman C. Fibro-osseous lesions of the skull base in the pediatric population. J Neurol Surg B Skull Base. 2018. 79: 31-6
30. Young FW, Putney FJ. Ossifying fibroma of the sinuses. Ann Otol Rhinol Laryngol. 1968. 77: 425-34