- Department of Neurosurgery, Ibn Rochd UHC, Hassan II University, Casablanca, Morocco
- Department of Anatomic Pathology, Ibn Rochd UHC, Hassan II University, Casablanca, Morocco
Correspondence Address:
Said Hilmani
Department of Neurosurgery, Ibn Rochd UHC, Hassan II University, Casablanca, Morocco
DOI:10.4103/2152-7806.177892
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hilmani S, Ngamasata T, Karkouri M, Elazahri A. Paraganglioma of the filum terminale mimicking neurinoma: Case report. Surg Neurol Int 02-Mar-2016;7:
How to cite this URL: Hilmani S, Ngamasata T, Karkouri M, Elazahri A. Paraganglioma of the filum terminale mimicking neurinoma: Case report. Surg Neurol Int 02-Mar-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/paraganglioma-of-the-filum-terminale-mimicking-neurinoma-case-report/
Abstract
Background:Paraganglioma of the filum terminale is an uncommon tumor of cauda equina region. Lumbar radiculopathies are revelations that can get complicated from cauda equina syndrome. Magnetic resonance imaging (MRI) allows the diagnosis without distinguishing it from a neurofibroma. Only histopathological study can bring certainty in the diagnosis. The treatment of choice is a complete removal.
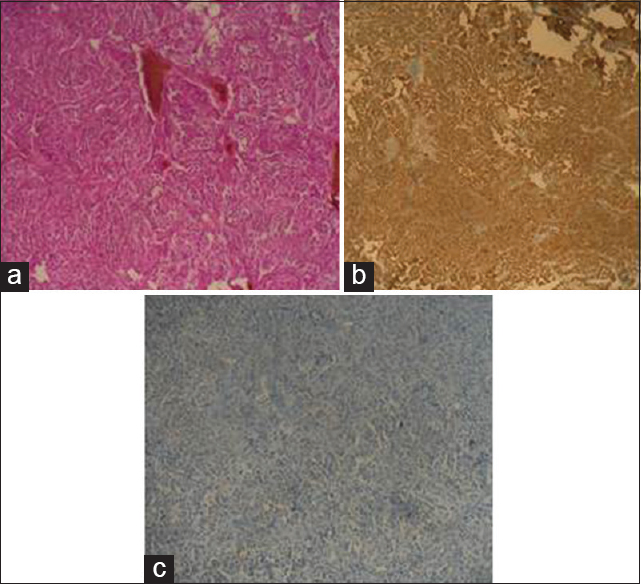
Case Description:We report a case of paraganglioma of the filum terminale in a 74-year-old female patient, admitted for cauda equina syndrome, which has been progressing for 2 years. MRI of medulla objectified an extramedullary lesion at L3–L4, diagnosed as neurinoma. A complete resection of the tumor was performed with a section of the filum terminale, which she was taking since birth. Histology confirmed the diagnosis of paraganglioma. The clinical course was characterized by a complete recovery of the deficit.
Conclusion:Through this case report, the authors discuss clinical and radiological aspects of this tumor, as well as the management in the light of published data.
Keywords: Cauda equina, neuroendocrine tumor, paraganglioma
INTRODUCTION
Paragangliomas are rare neuroendocrine tumors, usually benign. They grow in paraganglia and derive from the migration of neural crest cells that constitute the sympathetic and parasympathetic nervous system. Paraganglioma of the filum terminale is an exceptional tumor, compressing 2.5–3.8% of all cauda tumors.[
CASE REPORT
Our patient was a 74-year-old woman, without any particular pathological antecedents, presenting intermittent and badly systemized bilateral sciatica, along with weaknesses in both lower limbs, gradually progressing for 2 years. This symptomatology got complicated by sphincter disorders characterized by urinary incontinence and constipation. The clinical examination objectified incomplete paraplegia without sensory loss. Patellar and Achilles reflexes were reduced on both the lower limbs. MRI showed an intradural fusiform lesion at L3–L4, with an isosignal on T1 and T2, associated with a central nodular hypersignal on both sequences. The lesion took up the whole spinal canal, making a scallop shape on the vertebral body and laminating its posterior arch. The tumor homogenously enhanced following a gadolinium injection [
DISCUSSION
Paragangliomas are tumors that arise from neuroectodermal cells of the extra-adrenal sympathetic or parasympathetic nervous system. They are sporadic tumors; however, their origin has been discussed in many observations.[
CONCLUSION
Paraganglioma of the filum terminale is a rare tumor, often disclosed by lumbago and sciatica that are sometimes complicated by cauda equina syndrome. MRI with gadolinium injection allows setting surgical strategies, but does not bring certainty in the diagnosis, which is obtained through an anatomopathology. The total resection of the lesion, sectioning the filum terminale, guarantees a total cure and prevents recurrences in most of the cases. Nevertheless, a long-term clinical and radiological follow-up is necessary.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Boncoeur-Martel MP, Lesort A, Moreau JJ, Labrousse F, Roche I, Bouillet P. MRI of paraganglioma of the filum terminale. J Comput Assist Tomogr. 1996. 20: 162-5
2. Bozkurt G, Ziyal IM, Akbay A, Dal D, Can B, Ozcan OE. Cauda-filar paraganglioma with ‘silk cocoon’ appearance on spinal angiography. Acta Neurochir (Wien). 2005. 147: 99-100
3. Demirçivi Ozer F, Aydin M, Bezircioglu H, Oran I. Paraganglioma of the cauda equina: A highly vascular tumour. J Clin Neurosci. 2010. 17: 1445-7
4. Dial P, Marks C, Bolton J. Current management of paragangliomas. Surg Gynecol Obstet. 1982. 155: 187-92
5. Falavigna A, Righesso O, Volquind D, Salgado KB, Teles AR. Intraosseous sacral paraganglioma with extradural extension: Case report. Acta Neurochir (Wien). 2010. 152: 475-80
6. Gutenberg A, Wegner C, Pilgram-Pastor SM, Gunawan B, Rohde V, Giese A. Paraganglioma of the filum terminale: Review and report of the first case analyzed by CGH. Clin Neuropathol. 2010. 29: 227-32
7. Kleihues P, Burger PC, Scheithauer BW. The new WHO classification of brain tumours. Brain Pathol. 1993. 3: 255-68
8. Landi A, Tarantino R, Marotta N, Rocco P, Antonelli M, Salvati M. Paraganglioma of the filum terminale: Case report. World J Surg Oncol. 2009. 7: 95-
9. Lapierre F, Bataille B, Vandermarcq P, Goujon JM, Wager M, Page P. Cauda equina tumors in adults. Neurochirurgie. 1999. 45: 29-38
10. Levy RA. Paraganglioma of the filum terminale: MR findings. AJR Am J Roentgenol. 1993. 160: 851-2
11. Liccardo G, Pastore FS, Sherkat S, Signoretti S, Cavazzana A, Fraioli B. Paraganglioma of the cauda equina. Case report with 33-month recurrence free follow-up and review of the literature. J Neurosurg Sci. 1999. 43: 169-73
12. Marcol W, Kiwic G, Malinowska-Kolodziej I, Kotulska K, Kotas A, Adamek D. Paraganglioma of the cauda equina presenting with erectile and sphincter dysfunction. J Chin Med Assoc. 2009. 72: 328-31
13. Masuoka J, Brandner S, Paulus W, Soffer D, Vital A, Chimelli L. Germline SDHD mutation in paraganglioma of the spinal cord. Oncogene. 2001. 20: 5084-6
14. Mathon B, Carpentier A, Clemenceau S, Boch AL, Bitar A, Mokhtari K. Paraganglioma of the cauda equina region: Report of six cases and review of the literature. Neurochirurgie. 2012. 58: 341-5
15. Midi A, Yener AN, Sav A, Cubuk R. Cauda equina paraganglioma with ependymoma-like histology: A case report. Turk Neurosurg. 2012. 22: 353-9
16. Miller CA, Torack RM. Secretory ependymoma of the filum terminale. Acta Neuropathol. 1970. 15: 240-50
17. Mishra T, Goel NA, Goel AH. Primary paraganglioma of the spine: A clinicopathological study of eight cases. J Craniovertebr Junction Spine. 2014. 5: 20-4
18. Moran CA, Rush W, Mena H. Primary spinal paragangliomas: A clinicopathological and immunohistochemical study of 30 cases. Histopathology. 1997. 31: 167-73
19. Oh HS, Kim TW, Park KH. Spinal paraganglioma adherent to the cauda equina. Korean J Spine. 2014. 11: 252-4
20. Solymosi L, Ferbert A. A case of spinal paraganglioma. Neuroradiology. 1985. 27: 217-9
21. Strommer KN, Brandner S, Sarioglu AC, Sure U, Yonekawa Y. Symptomatic cerebellar metastasis and late local recurrence of a cauda equina paraganglioma. Case report. J Neurosurg. 1995. 83: 166-9
22. Wager M, Lapierre F, Blanc JL, Listrat A, Bataille B. Cauda equina tumors: A French multicenter retrospective review of 231 adult cases and review of the literature. Neurosurg Rev. 2000. 23: 119-29