- Department of Neurosurgery, Kurashiki Central Hospital, Kurashiki, Japan.
Correspondence Address:
Masanori Kinosada, Department of Neurosurgery, Kurashiki Central Hospital, Kurashiki, Japan.
DOI:10.25259/SNI_462_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masanori Kinosada, Hiroyuki Ikeda, Minami Uezato, Yasunori Yokochi, Ryosuke Kaneko, Yoshitaka Kurosaki, Masaki Chin. Parent artery occlusion for cerebral infarction after spontaneous recanalization in traumatic vertebral artery: A case report. 04-Aug-2023;14:278
How to cite this URL: Masanori Kinosada, Hiroyuki Ikeda, Minami Uezato, Yasunori Yokochi, Ryosuke Kaneko, Yoshitaka Kurosaki, Masaki Chin. Parent artery occlusion for cerebral infarction after spontaneous recanalization in traumatic vertebral artery: A case report. 04-Aug-2023;14:278. Available from: https://surgicalneurologyint.com/surgicalint-articles/12482/
Abstract
Background: There is no established treatment strategy for traumatic vertebral artery occlusion that does not require cervical spine repair surgery.
Case Description: A 49-year-old man was brought to our hospital with traffic trauma. Fractures were observed in the left lateral mass and transverse process of Atlas and the left vertebral artery was occluded at the level of the foramen transversum of Atlas. No acute cerebral infarction was observed. Because the cervical spinal cord was not compressed by the fracture, no repair surgery was performed. Continuous intravenous heparin and oral aspirin were started for traumatic vertebral artery occlusion. Thereafter, the left vertebral artery spontaneously recanalized, but no cerebral infarction was observed. The patient was discharged home on day 16 of injury. Four days later, however, he was brought to our hospital with nausea and lightheadedness. Acute cerebral infarction was observed in the left posterior inferior cerebellar artery territory and a thrombus in the left vertebral artery V4 segment. Parent artery occlusion was performed to prevent further cerebral infarction due to distal embolization of the thrombus. No further cerebral infarction occurred after the operation and the patient was discharged home with a modified Rankin scale score of 1.
Conclusion: In cases of traumatic vertebral artery occlusion without an occlusive mechanism, parent artery occlusion may be considered in terms of recanalization risk, regardless of the need for repair surgery.
Keywords: Blunt cervical injury, Endovascular surgery, Recanalization, Traumatic vertebral artery injury, Vertebral artery occlusion
INTRODUCTION
The frequency of vertebral artery injury in blunt cervical spine injury ranges from 19% to 39%,[
CASE PRESENTATION
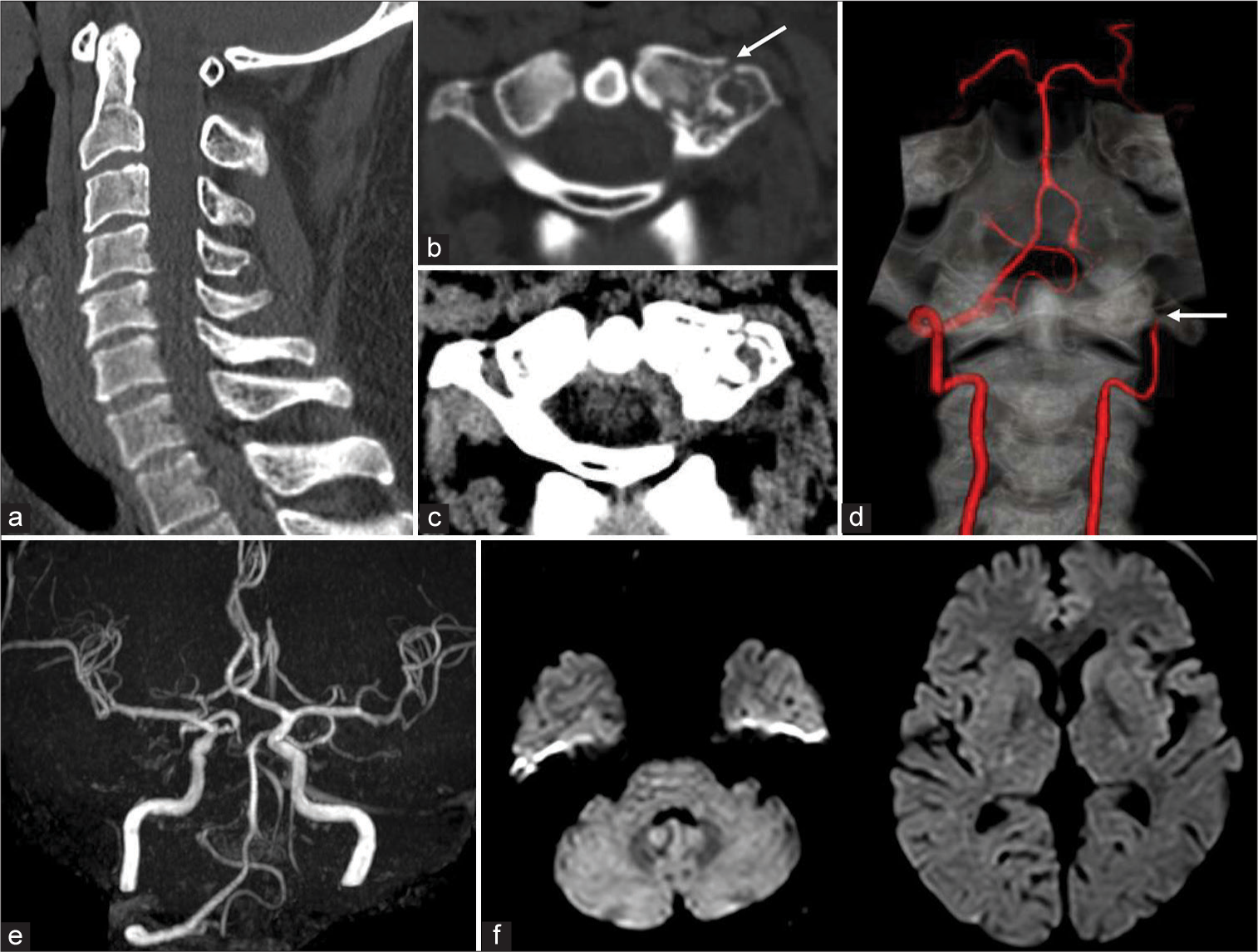
A 49-year-old man was brought to our hospital for emergency treatment after a collision with a car while riding a motorcycle. On arrival, his level of consciousness was 15 on the Glasgow Coma Scale, with no abnormal neurological findings. Medical history was significant for hypertension, dyslipidemia, Type 2 diabetes, and schizophrenia. Cervical spine computed tomography (CT) showed no cervical dislocation or spinal canal stenosis [
Figure 1:
Imaging findings on admission. Cervical spine computed tomography (CT) showing no cervical dislocation or spinal canal stenosis (a), but there were fractures in the left lateral mass and transverse process of Atlas, with no high density area suggestive of a thrombus in the foramen transversum. The white arrow indicates the fractures in the left lateral mass and transverse process of Atlas (b and c). CT angiography showing the left vertebral artery occluded at the level of the foramen transversum of Atlas. Both vertebral arteries are similar in diameter, and the left vertebral artery V4 segment and left posterior inferior cerebellar artery are depicted through the right vertebral artery. White arrow indicates occlusion (d). Magnetic resonance angiography showing no blood flow signal in the left vertebral artery (e). Diffusion-weighted magnetic resonance imaging showing no acute cerebral infarction (f).
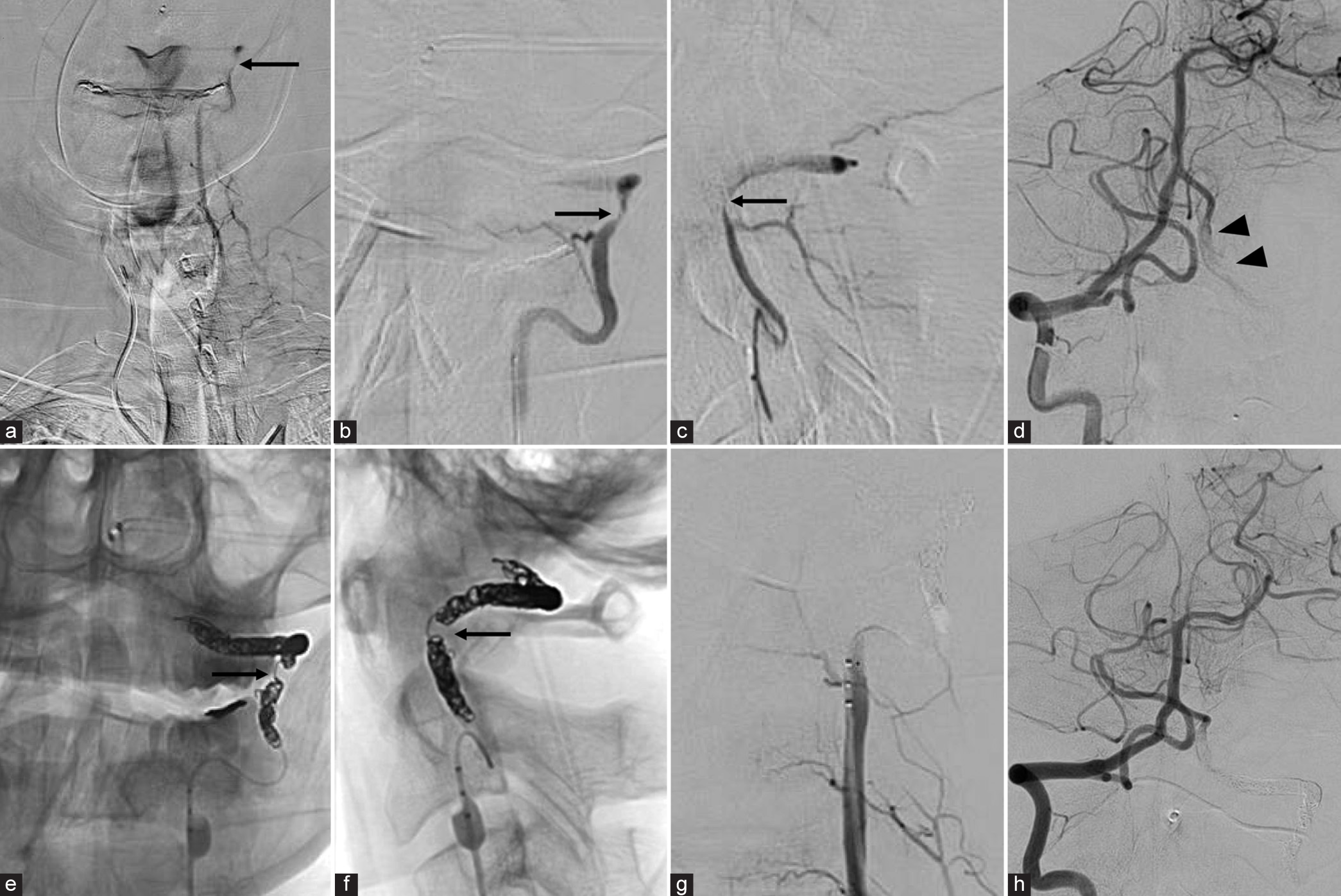
A diagnosis of a traumatic left vertebral artery injury with a transverse process fracture of Atlas was made. The left vertebral artery was occluded and was determined to be Grade IV on the Denver Grading Scale. Since there was no compression of the cervical spinal cord due to the Atlas fracture, conservative treatment with cervical collar immobilization was chosen. Because the patient did not require cervical spine repair surgery and had not suffered cerebral infarction, continuous intravenous heparin (10,000 units/day) and oral aspirin (100 mg/day) were started. Magnetic resonance angiography on day 2 showed spontaneous recanalization of the left vertebral artery, but diffusion-weighted magnetic resonance imaging showed no acute cerebral infarction [
Figure 2:
Imaging findings at first and second hospitalizations. Magnetic resonance angiography on day 2 showing spontaneous recanalization of the left vertebral artery (a). Magnetic resonance angiography on day 6 showing further increased blood flow signal in the left vertebral artery and vessel wall irregularity of the left vertebral artery at the level of the left foramen transversum of Atlas. White arrow indicates vessel wall irregularity (b). Magnetic resonance angiography on day 20 showing occlusion of the left vertebral artery (c). Diffusion-weighted magnetic resonance imaging on day 20 showing acute cerebral infarction in the left posterior inferior cerebellar artery territory (d). Computed tomography (CT) of the head on day 20 showing a high density area in the left vertebral artery V4 segment (e). CT angiography on day 20 showing severe stenosis of the left vertebral artery at the level of the foramen transversum of Atlas, with no visualization of the left posterior inferior cerebellar artery. White arrow indicates severe stenosis of the left vertebral artery (f).
On the night of 19, nausea and lightheadedness occurred. Because the symptoms did not improve, he was rushed to our hospital on day 20. Magnetic resonance angiography showed occlusion of the left vertebral artery [
Endovascular treatment
Heparin was administered intravenously under local anesthesia to maintain an activated coagulation time of >200 s. A 4-Fr diagnostic catheter was guided into the right vertebral artery. Left subclavian arteriography showed antegrade blood flow in the left vertebral artery above the level of the transverse foramen of Atlas [
Figure 3:
Intraoperative imaging findings. Left subclavian arteriography showing antegrade blood flow in the left vertebral artery above the level of the foramen transversum of Atlas. Black arrow indicates severe stenosis of the left vertebral artery (a). Microcatheter angiography showing severe stenosis of the left vertebral artery at the level of the foramen transversum of Atlas, a muscular branch proximal to the stenosis, and a branch of the posterior meningeal artery distal to the stenosis. Black arrow indicates severe stenosis of the left vertebral artery (b: frontal view/c: lateral view). Right vertebral artery angiography with the left vertebral artery blocked showing a thrombus in the left vertebral artery V4 segment and occlusion of the left posterior inferior cerebellar artery. Black arrowheads indicate a thrombus in the left vertebral artery V4 segment (d). Images after coil embolization. The black arrow indicates the severe stenosis of the left vertebral artery (e: frontal view/f: lateral view). Left vertebral artery angiography showing good embolization (g). Right vertebral artery angiography showing good visualization of the main intracranial artery (h).
Postoperative course
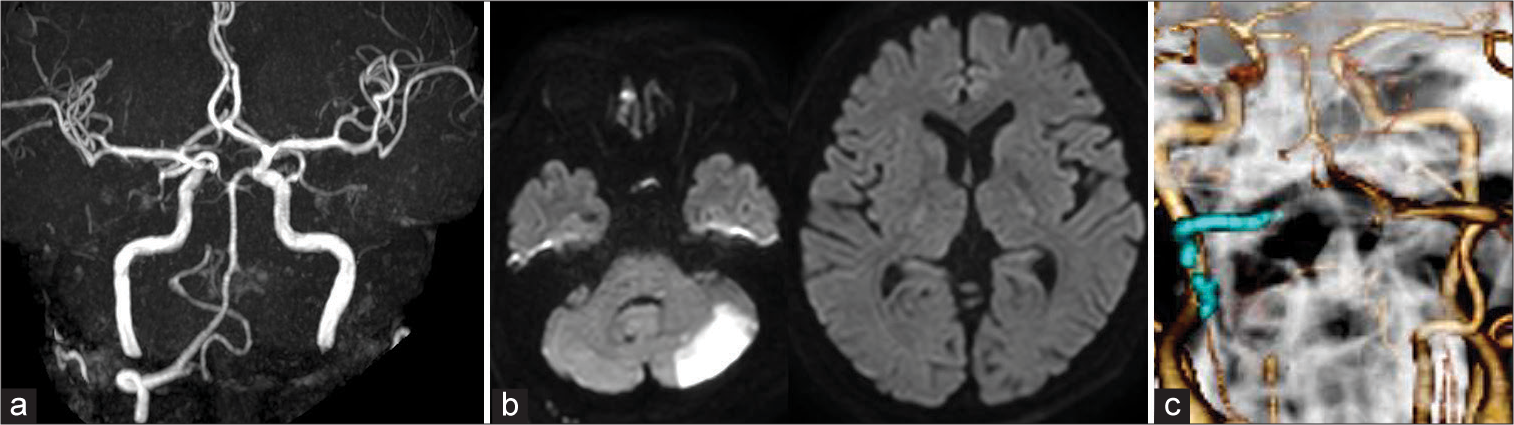
No new neurological abnormalities were found. Magnetic resonance angiography on day 21 showed occlusion of the left vertebral artery [
DISCUSSION
The left vertebral artery at the initial examination of this patient was thought to be occluded by intimal damage due to dissection, without any physical occlusion mechanism. In the acute phase, the left vertebral artery recanalized without thrombus formation; however, in the subacute phase, thrombus formation due to stenosis of the dissected lesion and intimal damage caused cerebral infarction. Parent artery occlusion was performed to prevent further cerebral infarction due to distal embolization of the thrombus.
Early diagnosis and prophylactic treatment are important for traumatic vertebral artery injury, but it is difficult to establish evidence-based treatment guidelines because the pathophysiology varies from case to case. Recently, endovascular treatment for traumatic vertebral artery occlusion by parent artery embolization proximal to the occlusion has been reported, but in cases that do not require cervical vertebral artery repair surgery, conservative treatment is chosen.[
One of the causes of cerebral infarction in this case is spontaneous recanalization of the left vertebral artery. In many cases of cervical spine injury that require repair, the vertebral artery is mechanically occluded, and when the occlusion is released by repair, recanalization occurs, resulting in cerebral infarction.[
Spontaneous recanalization of a traumatic vertebral artery occlusion without an occlusive mechanism may have the same risk of cerebral infarction as a mechanically occluded vertebral artery recanalized after repair surgery. Although it is reasonable to judge the need for parent artery occlusion on the basis of the presence or absence of repair, it is limited to cases of traumatic vertebral artery occlusion with an occlusive mechanism. In the case of traumatic vertebral artery occlusion with no occlusive mechanism, as in this case, it may be necessary to judge the need for parent artery occlusion not from the standpoint of repair, but from that of recanalization risk.
Lauerman et al. reported that all patients who had cerebral infarction after being diagnosed with traumatic vertebral artery occlusion recanalized and that the incidence of cerebral infarction when recanalization occurred was 22.2%.[
CONCLUSION
In cases of traumatic vertebral artery occlusion without an occlusive mechanism, parent artery occlusion may be considered in terms of recanalization risk, regardless of the need for repair surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Biffl WL, Moore EE, Elliott JP, Ray C, Offner PJ, Franciose RJ. The devastating potential of blunt vertebral arterial injuries. Ann Surg. 2000. 231: 672-81
2. Brommeland T, Helseth E, Aarhus M, Aarhus M, Moen KG, Dryskog S. Best practice guidelines for blunt cerebrovascular injury (BCVI). Scand J Trauma Resusc Emerg Med. 2018. 26: 90
3. Desouza RM, Crocker MJ, Haliasos N, Rennie A, Saxena A. Blunt traumatic vertebral artery injury: A clinical review. Eur Spine J. 2011. 20: 1405-16
4. Even J, McCullough K, Braly B, Hohl J, Song Y, Lee J. Clinical indications for arterial imaging in cervical trauma. Spine (Phila Pa 1976). 2012. 37: 286-91
5. Fujita Y, Aihara H, Nagashima H, Morishita A, Aoki K, Takayama H. Clinical features and treatment strategy of vertebral artery injury associated with cervical spine trauma. No Shinkei Geka. 2018. 46: 663-71
6. Herrera DA, Vargas SA, Dublin AB. Endovascular treatment of traumatic injuries of the vertebral artery. AJNR Am J Neuroradiol. 2008. 29: 1585-9
7. Kansagra AP, Cooke DL, English JD, Sincic RM, Amans MR, Dowd CF. Current trends in endovascular management of traumatic cerebrovascular injury. J Neurointerv Surg. 2014. 6: 47-50
8. Kwon JY, Kim NY, Suh DC, Kang DW, Kwon SU, Kim JS. Intracranial and extracranial arterial dissection presenting with ischemic stroke: Lesion location and stroke mechanism. J Neurol Sci. 2015. 358: 371-6
9. Lauerman MH, Feeney T, Sliker CW, Saksobhavivat N, Bruns BR, Laser A. Lethal now or lethal later: The natural history of grade 4 blunt cerebrovascular injury. J Trauma Acute Care Surg. 2015. 78: 1071-5 discussion 1074-5
10. Lebl DR, Bono CM, Velmahos G, Metkar U, Nguyen J, Harris MB. Vertebral artery injury associated with blunt cervical spine trauma: A multivariate regression analysis. Spine (Phila Pa 1976). 2013. 38: 1352-61
11. Miller PR, Fabian TC, Croce MA, Cagiannos C, Williams JS, Vang M. Prospective screening for blunt cerebrovascular injuries: Analysis of diagnostic modalities and outcomes. Ann Surg. 2002. 236: 386-95 discussion 393-5
12. Morton RP, Hanak BW, Levitt MR, Fink KR, Peterson EC, Vilela MD. Blunt traumatic occlusion of the internal carotid and vertebral arteries. J Neurosurg. 2014. 120: 1446-50
13. Panjabi MM, Dvorak J, Duranceau J, Yamamoto I, Gerber M, Rauschning W. Three-dimensional movements of the upper cervical spine. Spine (Phila Pa 1976). 1988. 13: 726-30
14. Tumialán LM, Theodore N. Basilar artery thrombosis after reduction of cervical spondyloptosis: A cautionary report. J Neurosurg Spine. 2012. 16: 492-6