- Department of Neurosurgery, Kanazawa University, Kanazawa, Japan
- Department of Neurosurgery, Kouseiren Takoka Hospital, Takaoka, Japan
- Department of Neurosurgery, Kanazawa Medical University, Uchinada, Japan.
Correspondence Address:
Tomoya Kamide, Department of Neurosurgery, Kanazawa Unversity, Kanazawa, Japan.
DOI:10.25259/SNI_1109_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kosuke Nambu1, Tomoya Kamide1, Taishi Tsutsui1, Tomohiro Kitabayashi2, Akifumi Yoshikawa3, Kouichi Misaki1, Mitsutoshi Nakada1. Partially thrombosed distal posterior cerebral artery aneurysm treated with surgical trapping through occipital transtentorial approach assisted by endovascular coil embolization. 20-Jan-2023;14:20
How to cite this URL: Kosuke Nambu1, Tomoya Kamide1, Taishi Tsutsui1, Tomohiro Kitabayashi2, Akifumi Yoshikawa3, Kouichi Misaki1, Mitsutoshi Nakada1. Partially thrombosed distal posterior cerebral artery aneurysm treated with surgical trapping through occipital transtentorial approach assisted by endovascular coil embolization. 20-Jan-2023;14:20. Available from: https://surgicalneurologyint.com/surgicalint-articles/12111/
Abstract
Background: Posterior cerebral artery (PCA) aneurysms are relatively rare. PCA aneurysms tend to be large, giant, fusiform, and partially thrombosed. Surgical treatments, such as neck clipping and trapping with or without bypass surgery, are curative treatments for thrombosed intracranial aneurysms. Few cases of surgical treatment of distal PCA aneurysms have been reported. We treated a partially thrombosed distal PCA aneurysm by trapping through the occipital transtentorial approach (OTA) assisted by endovascular coil embolization.
Case Description: A 21-year-old woman presented with a sudden headache. Brain computed tomography, magnetic resonance imaging, and a cerebral angiogram revealed a partially thrombosed aneurysm in the left PCA P3 segment. Her headaches had improved once within several days, but reoccurred due to an enlarged thrombosed aneurysm. Endovascular coil embolization was performed to assist the surgery. The aneurysm and the distal artery of the aneurysm were embolized to interrupt the blood flow into the aneurysm. The following day, trapping of the aneurysm was performed through the OTA. Eventually, we performed aneurysm excision because trapping alone was considered to have the potential for regrowth of the aneurysm. The patient’s postoperative course was uneventful. No recurrence of the aneurysm was observed at the 2-year follow-up.
Conclusion: OTA could be useful for the treatment of distal PCA aneurysms, whereas coil embolization may support the surgical treatment of partially thrombosed intracranial aneurysms.
Keywords: Endovascular treatment, Microsurgery, Posterior cerebral artery aneurysm, Stroke, Thrombectomy, Vasa vasorum
INTRODUCTION
Posterior cerebral artery (PCA) aneurysms are rare, accounting for <1–2% of all intracranial aneurysms.[
CASE REPORT
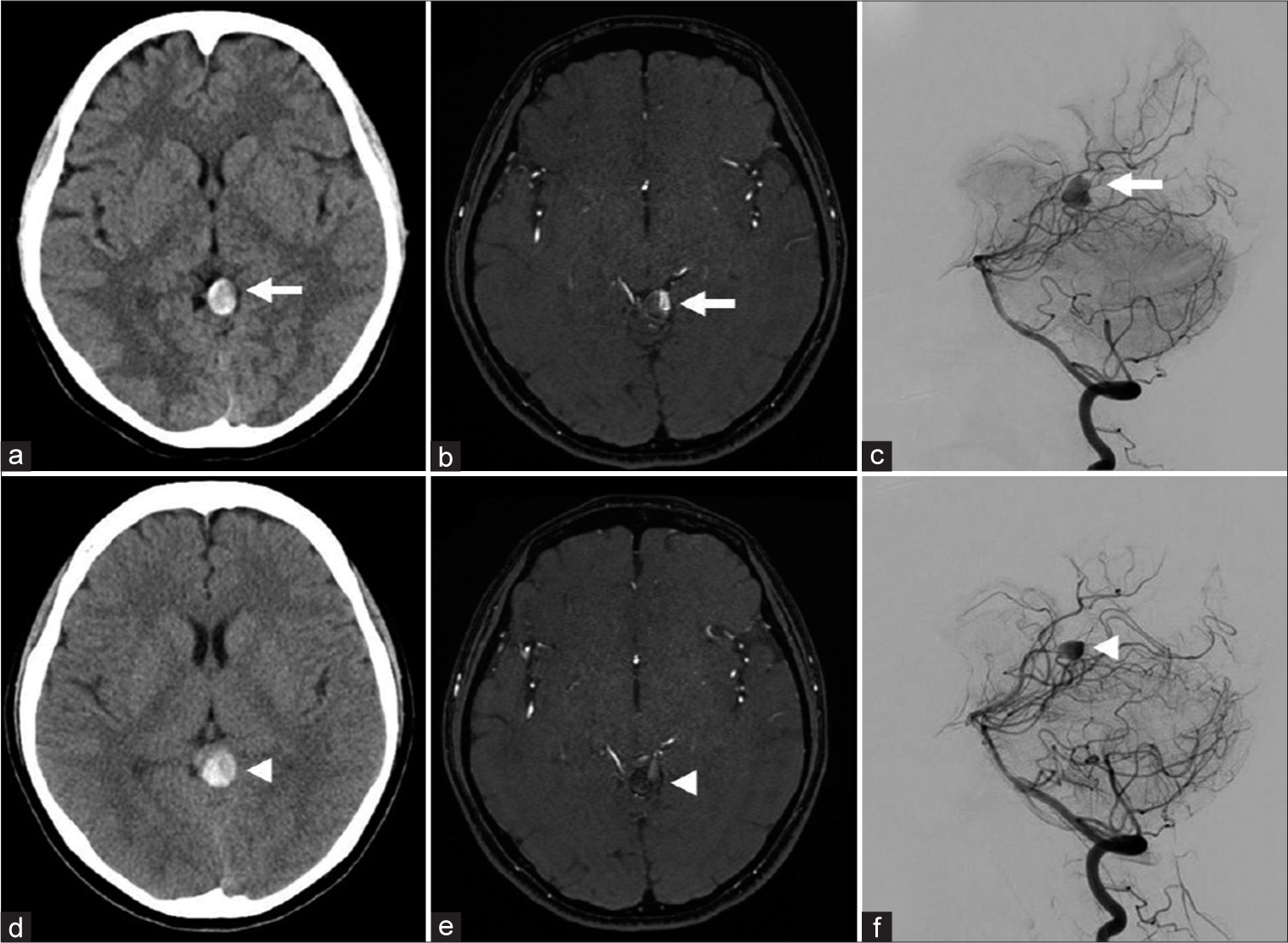
A 21-year-old woman presented with a sudden headache. Brain computed tomography (CT) and magnetic resonance imaging (MRI) revealed a thrombosed aneurysm on the quadrigeminal cistern [
Figure 1:
(a) Computed tomography (CT) showing a hyperdense lesion suspected to be a thrombosed aneurysm on the quadrigeminal cistern (arrow). (b) Magnetic resonance angiography (MRA) demonstrating partial blood flow in the aneurysm (arrow). (c) Left vertebral angiography image showing an aneurysm located in the P3 segment of the left posterior cerebral artery (arrow). (d) Enlargement of the aneurysm on CT (arrowhead). (e and f) MRA and left vertebral angiography showing decreased blood flow into the aneurysm compared to 1 month before (arrowheads).
Figure 2:
(a) Three-dimensional rotational angiography showing the proximal (arrow) and distal arteries (arrowheads). (b) The schematic drawing of the case during the coil embolization (orange line: microcatheter, blue mass: embolized coil, arrow: proximal artery, arrowheads: distal artery). (c) Left vertebral angiography at the end of coil embolization showing the disappearance of blood flow into the aneurysm.
Figure 3:
Intraoperative views. (a) Embolized coils the day before in the distal artery (arrow). (b) Clips are applied to the proximal (white arrow) and distal (black arrow) arteries of the aneurysm. (c) Embolized coils the day before in the aneurysm not interrupting the thrombectomy (arrowheads). (d) Vessels feeding the wall of the aneurysm (arrowheads). (e) The aneurysm removed in one lump. (f) Postoperative magnetic resonance imaging showing no residual lesion and no ischemic change.
DISCUSSION
In this case, a hybrid strategy including endovascular coil embolization and microsurgical trapping through the OTA was effective for a partially thrombosed distal PCA aneurysm.
PCA is often divided into P1-P4 segments.[
It had been reported that parent artery occlusion (PAO) is needed to treat complicated PCA aneurysms, such as large or giant, fusiform, and thrombosed cases.[
As treatment for partially thrombosed aneurysms, endovascular treatment is considered inferior to surgical treatment due to a higher recanalization rate.[
We performed endovascular coil embolization to assist the surgery, considering the possibility that a thrombectomy of the aneurysm would be necessary when reaching the artery proximal to the aneurysm. We observed that the coils of the distal vessel embolized the day before, which were good markers during surgery. The coils in the aneurysm did not interfere with thrombectomy because they were packed near the proximal neck. Even if we had not been able to secure the proximal vessels beforehand, we would have been able to perform a thrombectomy before trapping. In our case, endovascular coil embolization was safe and helpful for assisting surgery through the OTA. Endovascular coil embolization might be useful in supporting the surgical treatment of partially thrombosed intracranial aneurysms.
CONCLUSION
OTA is a useful approach for distal PCA aneurysms and endovascular coil embolization might be useful in supporting surgical treatment of partially thrombosed intracranial aneurysms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chang SW, Abla AA, Kakarla UK, Sauvageau E, Dashti SR, Nakaji P. Treatment of distal posterior cerebral artery aneurysms: A critical appraisal of the occipital artery-to-posterior cerebral artery bypass. Neurosurgery. 2010. 67: 16-26 discussion 25-6
2. Ciceri EF, Klucznik RP, Grossman RG, Rose JE, Mawad ME. Aneurysms of the posterior cerebral artery: Classification and endovascular treatment. AJNR Am J Neuroradiol. 2001. 22: 27-34
3. Enomoto Y, Egashira Y, Matsubara H, Yoshimura S, Iwama T. Long-term outcome of endovascular therapy for large or giant thrombosed intracranial aneurysms. World Neurosurg. 2020. 144: e507-12
4. Ferrante L, Acqui M, Trillò G, Lunardi P, Fortuna A. Aneurysms of the posterior cerebral artery: Do they present specific characteristics?. Acta Neurochir (Wien). 1996. 138: 840-52
5. Guresir E, Wispel C, Borger V, Hadjiathanasiou A, Vatter H, Schuss P. Treatment of partially thrombosed intracranial aneurysms: Single-center series and systematic review. World Neurosurg. 2018. 118: e834-41
6. Hamada J, Morioka M, Yano S, Todaka T, Kai Y, Kuratsu J. Clinical features of aneurysms of the posterior cerebral artery: A 15-year experience with 21 cases. Neurosurgery. 2005. 56: 662-70 discussion 662-70
7. Iihara K, Murao K, Sakai N, Soeda A, Ishibashi-Ueda H, Yutani C. Continued growth of and increased symptoms from a thrombosed giant aneurysm of the vertebral artery after complete endovascular occlusion and trapping: The role of vasa vasorum. Case report. J Neurosurg. 2003. 98: 407-13
8. Kim YB, Lee JW, Huh SK, Kim BM, Kim DJ. Outcomes of multidisciplinary treatment for posterior cerebral artery aneurysms. Clin Neurol Neurosurg. 2013. 115: 2062-8
9. Krings T, Alvarez H, Reinacher P, Ozanne A, Baccin CE, Gandolfo C. Growth and rupture mechanism of partially thrombosed aneurysms. Interv Neuroradiol. 2007. 13: 117-26
10. Locksley HB. Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the cooperative study. J Neurosurg. 1966. 25: 219-9
11. Park W, Kwon DH, Ahn JS, Lee SH, Park JC, Kwun BD. Treatment strategies for dissecting aneurysms of the posterior cerebral artery. Acta Neurochir (Wien). 2015. 157: 1633-43
12. Pia HW, Fontana H. Aneurysms of the posterior cerebral artery. Locations and clinical pictures. Acta Neurochir (Wien). 1977. 38: 13-35
13. Portanova A, Hakakian N, Mikulis DJ, Virmani R, Abdalla WM, Wasserman BA. Intracranial vasa vasorum: Insights and implications for imaging. Radiology. 2013. 267: 667-79
14. Sakata S, Fujii K, Matsushima T, Fujiwara S, Fukui M, Matsubara T. Aneurysm of the posterior cerebral artery: Report of eleven cases--surgical approaches and procedures. Neurosurgery. 1993. 32: 163-7 discussion 167-8
15. Tanahashi K, Araki Y, Uda K, Muraoka S, Motomura K, Lushun C. Posterior cerebral artery reconstruction by in-situ bypass with superior cerebellar artery via occipital transtentorial approach. World Neurosurg. 2019. 126: 24-9
16. Yang K, Park JC, Ahn JS, Kwon DH, Kwun BD, Kim CJ. Characteristics and outcomes of varied treatment modalities for partially thrombosed intracranial aneurysms: A review of 35 cases. Acta Neurochir (Wien). 2014. 156: 1669-75
17. Zeal AA, Rhoton AL. Microsurgical anatomy of the posterior cerebral artery. J Neurosurg. 1978. 48: 534-59