- Department of Neurosurgery, Faculty of Medicine and Pharmacy of Oujda, Mohammed First University Morocco, Oujda, Morocco.
Correspondence Address:
Mohammed Alamine Elfarissi, Department of Neurosurgery, Faculty of Medicine and Pharmacy of Oujda, Mohammed First University Morocco, Oujda, Morocco.
DOI:10.25259/SNI_476_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammed Alamine Elfarissi, Mohamed Dahamou, Younes Dehneh, Mohammed Lhamlili, Mohamed Khoulali, Noureddine Oulali, Faycal Moufid. Pediatric sellar-suprasellar tuberculosis: A case report and review of the literature. 27-Oct-2023;14:379
How to cite this URL: Mohammed Alamine Elfarissi, Mohamed Dahamou, Younes Dehneh, Mohammed Lhamlili, Mohamed Khoulali, Noureddine Oulali, Faycal Moufid. Pediatric sellar-suprasellar tuberculosis: A case report and review of the literature. 27-Oct-2023;14:379. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12614
Abstract
Background: Pediatric sellar-suprasellar tuberculosis is a rare form of tuberculosis that affects the pituitary gland and surrounding areas in the brain. It can be difficult to diagnose based on clinical and radiological signs alone, as they can be similar to other pituitary masses. A combination of biological, hormonal, and imaging examinations can aid in making an accurate diagnosis. It is important to consider tuberculosis in the differential diagnosis of sellar-suprasellar masses in the pediatric population, especially in areas with a high prevalence of tuberculosis.
Case Description: A 17-year-old male with no history of illness showed up with a series of symptoms, including headaches and vision problems. A sellar-suprasellar lesion was seen on imaging, along with several minor lesions. The diagnosis of tuberculosis meningitis with cerebral and pituitary tuberculoma was made after cerebrospinal fluid analysis revealed the presence of tuberculosis. Treatment with anti-tuberculosis drugs led to clinical improvement and lesion resolution.
Conclusion: Children’s sellar tuberculomas can be difficult to diagnose since they resemble other pituitary tumors. It is essential to take them into account in the differential diagnosis, especially in regions with a high incidence of tuberculosis. Long-term chemotherapy is the recommended course of treatment, and monthly follow-up visits are necessary to check hormone levels and evaluate whether a permanent hormone replacement is necessary.
Keywords: Antitubercular chemotherapy, Granuloma, Meningitis, Pediatric infection, Pituitary tuberculosis
INTRODUCTION
Mycobacterium tuberculosis is a highly infectious disease that is responsible for the greatest number of deaths worldwide caused by a single organism. It primarily affects the lungs, but extra-pulmonary localization has also been reported. Despite advances in medical treatment, tuberculosis remains a major global health problem, with an estimated 1.3 million deaths in HIV-negative patients in 2020. Only 1% of tuberculosis cases worldwide involve the central nervous system, which can affect the brain, meninges, or adjacent bone depending on the host’s immune factors.[
According to the literature, there were 28 cases of pediatric pituitary tuberculosis reported up to 2022 [
In this report, we present a case of pediatric pituitary tuberculosis and review the literature on children. It is important to consider tuberculosis in the differential diagnosis of sellar-suprasellar masses in the pediatric population, especially in areas with a high prevalence of tuberculosis.
CASE REPORT
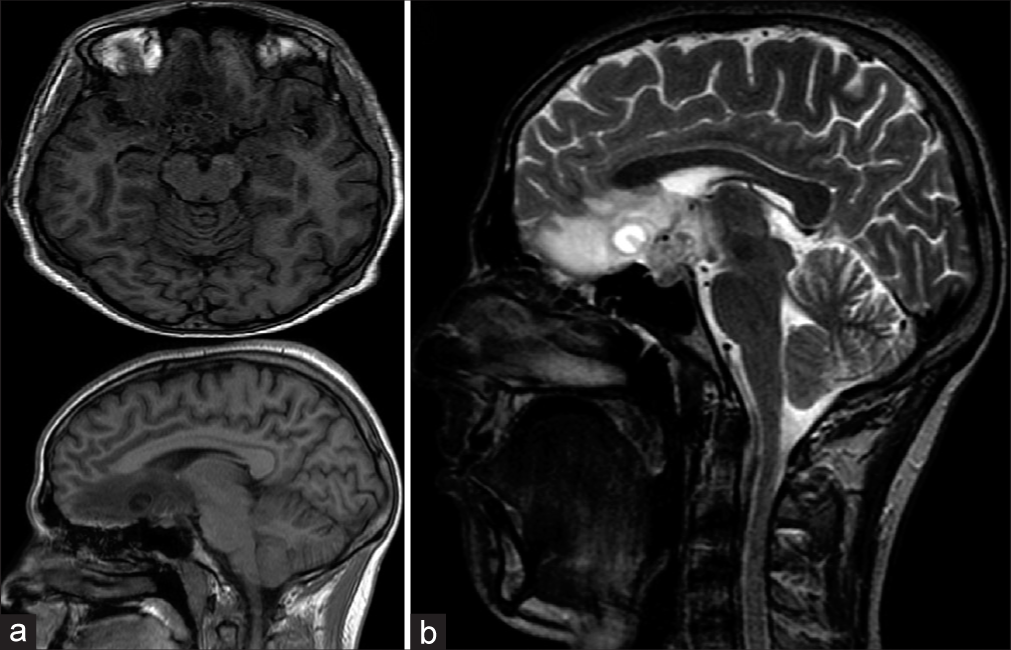
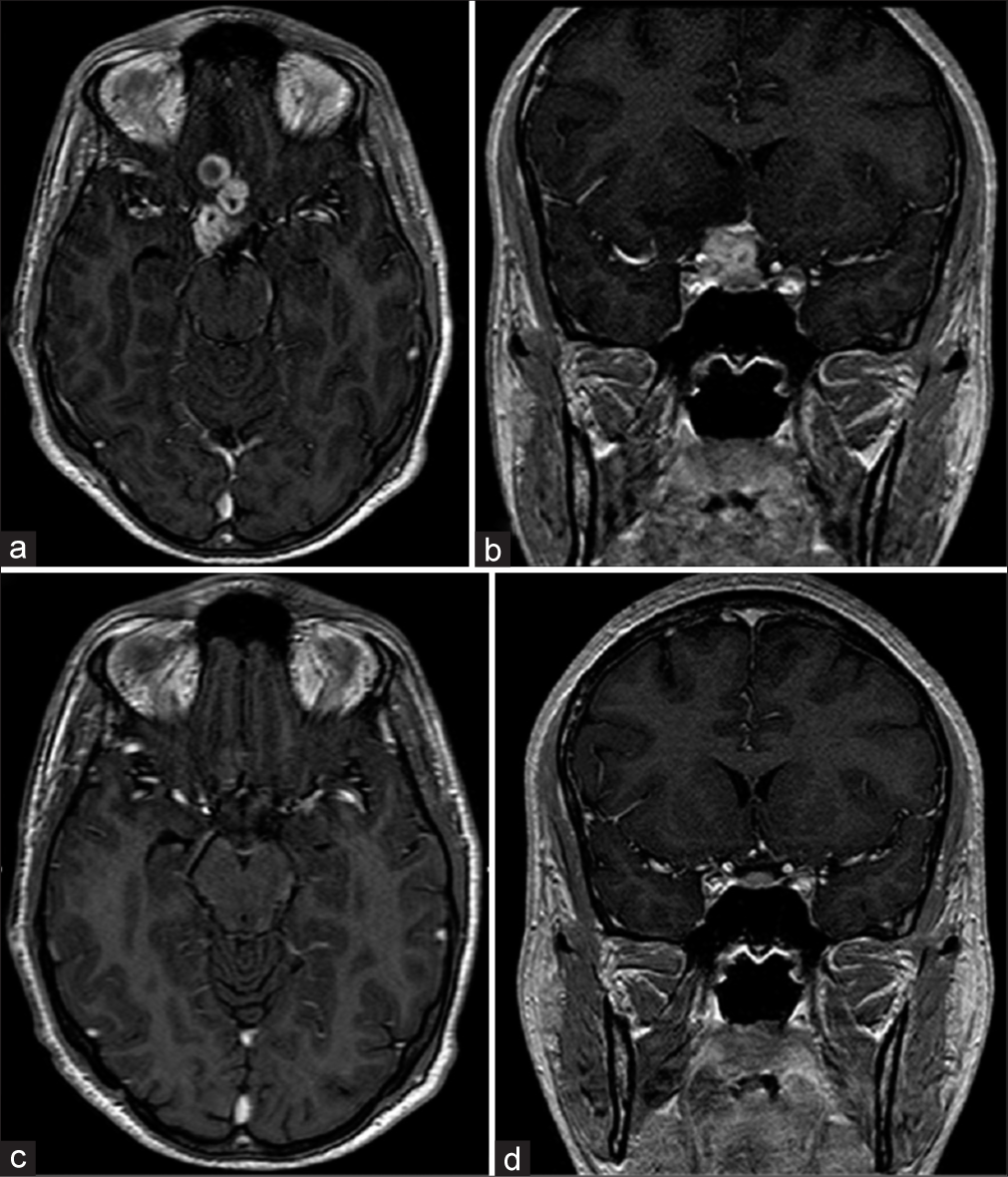
A 17-year-old male without a medical history presented progressive symptoms during the past month, consisting of headaches, decreased visual acuity, and visual field impairment with right temporal hemianopia. The clinical examination found a conscious patient, slightly feverish, pulse was 78/min, and his blood pressure was 120/76 mm Hg. The lung examination was clear on auscultation. The chest radiograph was normal. Magnetic resonance imaging (MRI) of the brain shows a sellar-suprasellar lesion, isointense to hypointense on T1, isointense to hyperintense on T2 [
Based on clinical features, neuroimaging, and investigations, a diagnosis of meningitis tuberculosis with cerebral and pituitary tuberculoma was made. Treatment for tuberculosis was initiated with a 2-month combination of isoniazid, rifampicin, pyrazinamide, and ethambutol, followed by 7 months of isoniazid and rifampicin, associated with corticosteroid therapy, and the evolution was marked by the clinical improvement of the patient, even on the radiological level, by the disappearance of the lesion [
DISCUSSION
Tuberculomas in intracranial space can occur at any age, affecting mostly young adults,[
CONCLUSION
The diagnosis of sellar tuberculomas in children can be challenging as the clinical and radiological presentations can be similar to other pituitary masses. It is crucial to consider pituitary tuberculomas in the differential diagnosis of suprasellar masses, particularly in developing countries where the incidence of tuberculosis is high. Avoiding surgery is the best route to prevent the development of new hormonal deficiencies but sometimes it is a necessary procedure to obtain tissue for diagnosis through biopsy or surgery before starting any specific treatment. The recommended treatment for pituitary tuberculomas is long-term chemotherapy with anti-tubercular drugs, which generally results in a good outcome. However, it is not entirely clear if patients require lifelong replacement of deficient hormones, so regular follow-up is necessary to monitor for any changes in hormone levels.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agrawal VM, Giri PJ. Tuberculosis: A common infection with rare presentation, isolated sellar tuberculoma with panhypopituitarism. J Neurosci Rural Pract. 2019. 10: 327-30
2. Altunbasak S, Baytok V, Alhan E, Yuksel B, Aksaray N. Suprasellar tuberculoma causing endocrinologic disorders and imitating craniopharyngioma. Pediatr Neurosurg. 1995. 23: 328-31
3. Ben Abid F, Abukhattab M, Karim H, Agab M, Al-Bozom I, Ibrahim WH. Primary pituitary tuberculosis revisited. Am J Case Rep. 2017. 18: 391-4
4. Bonifacio-Delgadillo D, Aburto-Murrieta Y, Salinas-Lara C, Sotelo J, Montes-Mojarro I, Garcia-Marquez A. Clinical presentation and magnetic resonance findings in sellar tuberculomas. Case Rep Med. 2014. 2014: 961913
5. Brooks MH, Dumlao JS, Bronsky D, Waldstein SS. Hypophysial tuberculoma with hypopituitarism. Am J Med. 1973. 54: 777-81
6. Chellen S, Whittaker E, Eisenhut M, Grandjean L. Cerebral tuberculomas in a 6-year-old girl causing central diabetes insipidus. BMJ Case Rep. 2018. 2018: 1-5
7. Daoud E, Mezghani S, Fourati H, Ketata H, Guermazi Y, Ayadi K. MR imaging features of tuberculosis of the sellar region. J Radiol. 2011. 92: 714-21
8. Dayal D, Muthuvel B, Singh Sodhi K. Obesity as the Presenting Feature of Sellar Suprasellar Tuberculoma. Indian J Endocrinol Metab. 2018. 22: 176-7
9. Dhiman R, Lakra S, Panda PK, Hemachandran N, Sharma S, Saxena R. Neuro-ophthalmic manifestations of tuberculosis. Eye (Lond). 2022. 36: 15-28
10. Dutta P, Bhansali A, Singh P, Bhat MH. Suprasellar tubercular abscess presenting as panhypopituitarism: A common lesion in an uncommon site with a brief review of literature. Pituitary. 2006. 9: 73-7
11. Gucuyener K, Baykaner MK, Keskil IS, Hasanoğlu A, Ilgit E, Beyazova U. Tuberculoma in the suprasellar cistern: Possible CT--misinterpretation as aneurysm. Pediatr Radiol. 1993. 23: 153-4
12. Higuchi M, Arita N, Mori S, Satoh B, Mori H, Hayakawa T. Pituitary granuloma and chronic inflammation of hypophysis: Clinical and immunohistochemical studies. Acta Neurochir (Wien). 1993. 121: 152-8
13. Iyer D, Lissauer S, Jones G, Karandikar S, Shaw N, Walsh R. Panhypopituitarism after tuberculous meningitis with suprasellar abscess. Arch Dis Child. 2011. 96: A53
14. Jain R, Kumar R. Suprasellar tuberculoma presenting with diabetes insipidus and hypothyroidism--a case report. Nov Drug Targets with Tradit Herb Med Sci Clin Evid Published online. 2001. p. 314-316
15. Ketan D, Nadkarni T, Goel A. Tuberculomas of the hypophysis cerebri: Report of five cases. J Clin Neurosci. 2003. 10: 562-6
16. Khursheed N, Sarbjit S, Rumana M, Altaf R, Abrar . Sellarsuprasellar tuberculomas in children: 2 Cases and literature review. Pediatr Neurol. 2011. 44: 463-6
17. Kirshbaum JD, Levy HA. Tuberculoma of hypophysis with insufficiency of anterior lobe. Arch Intern Med. 1941. 2: 1095-104
18. Letchworth T. Tuberculoma of the pituitary body. Br Med J. 1924. 28: 1127
19. Mittal P, Dua S, Saggar K, Gupta K. Magnetic resonance findings in sellar and suprasellar tuberculoma with hemorrhage. Surg Neurol Int. 2010. 1: 73
20. Muniz BC, Ribeiro BN de F, Ventura N, Gasparetto EL, Marchiori E. Isolated suprasellar involvement in tuberculosis: Findings on magnetic resonance imaging. Radiol Bras. 2019. 13: 109-11
21. Pagad HS, Hariyani R, Jain A, Shanbhag N. Case report blue sclera and osteogenesis imperfecta–A rare association. Kerala J Ophthalmol. 2018. 34: 240-3
22. Pereira J, Vaz R, Carvalho D, Cruz C. Thickening of the pituitary stalk: A finding suggestive of intrasellar tuberculoma? Case report. Neurosurgery. 1995. 2: 1013-6
23. Pruthi N, Shrithi K, Pandey P. Suprasellar tuberculoma associated with unilateral moyamoya phenomenon: Case report. Neurol India. 2014. 62: 447-9
24. Ranjan A, Chandy MJ. Intrasellar tuberculoma. Br J Neurosurg. 1994. 8: 179-85
25. Rock RB, Olin M, Baker CA, Molitor TW, Peterson PK. Central nervous system tuberculosis: Pathogenesis and clinical aspects. Clin Microbiol Rev. 2008. 21: 243-61
26. Saini KS, Patel AL, Shaikh WA, Magar LN, Pungaonkar SA. Magnetic resonance spectroscopy in pituitary tuberculoma. Singapore Med J. 2011. 15: 1-615
27. Sanjay B, Shinghal U, Jain M, Jaiswal A, Wadwekar V, Das K. Clinicoradiological presentation, management options and a review of sellar and suprasellar tuberculomas. J Clin Neurosci. 2009. 16: 1560-6
28. Sarkar S, Dey A, Morshed M, Sarkar S. Racemose pattern of intracranial tuberculoma at the basal, suprasellar and perimesencephalic cisterns-A case report. Surg Case Rep. 2020. 3: 1-4
29. Seeburg DP, Dremmen MH, Huisman TA. Imaging of the sella and parasellar region in the pediatric population. Neuroimaging Clin N Am. 2017. 27: 99-121
30. Sharma MC, Arora R, Mahapatra AK, Sarat-Chandra P, Gaikwad SB, Sarkar C. Intrasellar tuberculoma--an enigmatic pituitary infection: A series of 18 cases. Clin Neurol Neurosurg. 2000. 102: 72-7
31. Singh S. Pituitary tuberculoma: Magnetic resonance imaging. Neurol India. 2003. 51: 548-50
32. Srisukh S, Tanpaibule T, Kiertiburanakul S, Boongird A, Wattanatranon D, Panyaping T. Pituitary tuberculoma: A consideration in the differential diagnosis in a patient manifesting with pituitary apoplexy-like syndrome. IDCases. 2016. 5: 63-6
33. Stalldecker G, Diez S, Carabelli A, Reynoso R, Rey R, Hofmann N. Pituitary stalk tuberculoma. Pituitary. 2002. 5: 155-62
34. Verma R, Patil TB, Lalla R. Pituitary apoplexy syndrome as the manifestation of intracranial tuberculoma. BMJ Case Rep. 2014. 4: 12-72
35. Zhao BB, Tian C, Fu LJ, Zhang XB. Suprasellar cistern tuberculoma presenting as unilateral ocular motility disorder and ptosis: A case report. World J Clin Cases. 2022. 10: 4691-7
36. Ziani I, Bouichrat N, Bentebbaa FZ, Rouf S, Latrech H. Polyuropolydipsic syndrome: A descriptive study of 11 cases. Ann Endocrinol (Paris). 2021. 82: 371-2