- Department of Neurosurgery, Euromedica Geniki Kliniki of Thessaloniki, Thessaloniki, Greece
- Department of Neurosurgery, Aristotle University of Thessaloniki, Ippokration General Hospital, Thessaloniki, Greece
- Faculty of Medicine, University of Pristina, Temporarily Settled in Kosovska Mitrovica, Serbia
Correspondence Address:
Marios Theologou
Department of Neurosurgery, Aristotle University of Thessaloniki, Ippokration General Hospital, Thessaloniki, Greece
DOI:10.4103/sni.sni_85_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marios Theologou, Theologos Theologou, Dimitrios Zevgaridis, Nikolaos Skoulios, Slavisa Matejic, Christos Tsonidis. Pedicle screw placement accuracy impact and comparison between grading systems. 27-Jun-2017;8:131
How to cite this URL: Marios Theologou, Theologos Theologou, Dimitrios Zevgaridis, Nikolaos Skoulios, Slavisa Matejic, Christos Tsonidis. Pedicle screw placement accuracy impact and comparison between grading systems. 27-Jun-2017;8:131. Available from: http://surgicalneurologyint.com/surgicalint-articles/pedicle-screw-placement-accuracy-impact-and-comparison-between-grading-systems-2/
Abstract
Background:Pedicle screw instrumentation is widely used for spinal stabilization. However, the accuracy for free-hand screw placement ranges from 69% to 94%. This study assesses the value of the existing classification systems, and investigates their impact on the ability to assess the accuracy of free-hand screw placement.
Methods:Data were collected retrospectively from the medical records of 34 patients who received 224 pedicle screws placed utilizing a free-hand technique. Screw placement was evaluated employing the 2-mm increment and Zdichavsky et al. classification systems. Kappa coefficient and Landis and Koch interpretations were employed for statistical analysis.
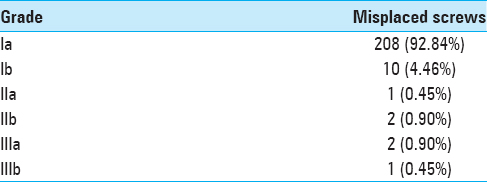
Results:The 2-mm increment classification system resulted in a total of 18 (8.03%) misplaced screws. Lateral screw misplacement was observed in 13 (5.8%) instances, with medial pedicle wall penetration being noted in 5 (2.23%). Of the 18 misplaced screws, 4 (22.22%) were classified as minor (≤2 mm), 12 (66.67%) as moderate (2–4 mm), and 2 (11.11%) as severe (>4 mm) (K = 0.882). The Zdichavsky et al. grading system categorized 208 (92.84%) pedicle screws as Ia, 10 (4.46%) as Ib, 1 (0.45%) as IIa, 2 (0.90%) as IIb, 2 (0.90%) as IIIa, and 1 (0.45%) as IIIb grade; this resulted in a total of 16 (7.14%) misplaced screws (K = 0.980). One patient exhibited a new postoperative radiculopathy attributed to poor screw placement. There were no additional early or late postsurgical complications attributed to screw misplacement.
Conclusion:The free-hand pedicle screw placement technique is both safe and effective. Postoperative computed tomography studies; however, are useful to confirm the accuracy of screw placement. Although, the available grading systems proved reliable, easy to use, and clearly reflected the individual surgeon's skills, they do not clearly document whether screws are safely placed.
Keywords: Accuracy, evaluation, grading, pedicle screw
INTRODUCTION
Pedicle screw instrumentation is widely used for the stabilization of the subaxial cervical, thoracic, and lumbar spine.[
MATERIALS AND METHODS
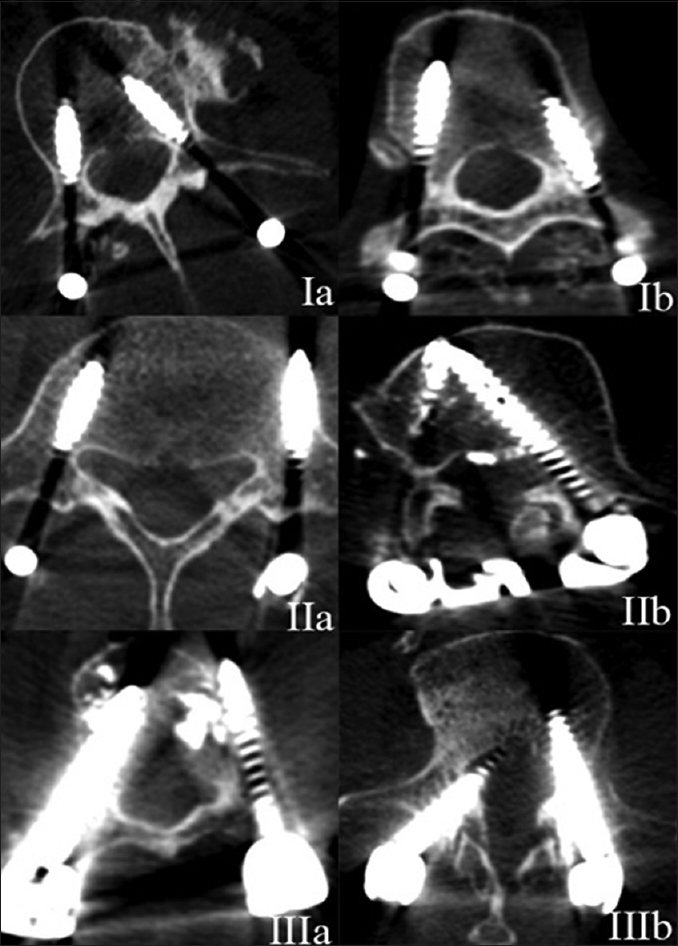
In this retrospective observational study, data were collected from the medical records of 34 patients operated on by a single-surgical team utilizing a free-hand technique for the placement of lumbar pedicle screws utilizing a posterior approach with conventional techniques (e.g., anatomical landmarks for guidance). Patients were followed up for a minimum of 12 months. A postoperative CT allowed for direct assessment of the accuracy with which 224 pedicle screws were placed. CT images were independently reviewed by both a neurosurgeon and a radiologist. They employed the two of the most popular grading systems: the 2-mm increment based grading system and the Zdichavsky et al. grading criteria. CT's were evaluated using the RadiAnt DICOM Viewer v. 2.2.9. statistical analysis was performed using the IBM SPSS v. 21. A literature review identified these two and other popular grading systems.
RESULTS
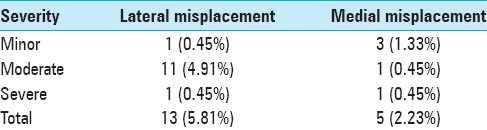
The use of the 2-mm increment classification, resulted in 18 (8.03%) misplaced screws; lateral screw misplacement was observed in 13 (5.8%) instances; medial pedicle wall penetration in 5 (2.23%). Of the 18 misplaced screws, 4 (22.22%) were classified as minor (≤2 mm), 12 (66.67%) as moderate (2–4mm), and 2 (11.11%) as severe (>4 mm) [
DISCUSSION
Innovative CT-guided techniques have greatly contributed to minimizing the incidence of pedicle screw misplacement, especially when utilized by experienced surgeons. The superiority of navigation systems is particularly obvious when applied to abnormal/anomalous spinal structures.[
Grading systems
This study compared the value of two systems regarding the free-hand (under fluoroscopy) misplacement of the lumbar pedicle screws. Aosude et al. determined the 2-mm incremental based system was the most accurate to define screw malplacement[
Figure 1
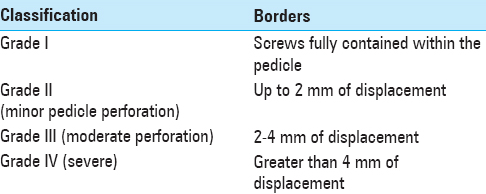
Zdichavsky grading system IA: ≥ 50% of pedicle screw diameter (PSD) within the pedicle & ≥ 50% of PSD within the vertebral body IB: > 50% of PSD lateral outside the pedicle & > 50% of PSD within the vertebral body IIA: ≥ 50% of PSD within the pedicle & > 50% of PSD lateral outside the vertebral body IIB: ≥ 50% of PSD within the pedicle & tip of PS crossing the middle line of the vertebral body IIIA: >50% of PSD lateral outside the pedicle & >50% of PSD lateral outside the vertebral body IIIB: >50% of PSD medial outside the pedicle & tip of PS crossing midline of the vertebral body
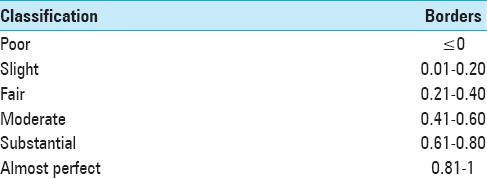
We employed the Landis and Koch Kappa interpretation system for statistical assessment[
Screw misplacement/complication rates
Our misplacement and early/late complications rates proved to be comparable to the lowest in the literature, showing that our free hand, fluoroscopically guided technique (without using CT guidance) remains safe and effective. Although, the overall misplacement percentage in the literature is low, this does not reflect the potential for neurological/other morbidity.
CONCLUSION
Free-hand pedicle screw placement techniques performed under fluoroscopic guidance remain safe and effective for spine stabilization in the lumbar region. For experienced surgeons, there was only a slight difference in results between conventional vs. computer-assisted techniques for accurate screws placement. We advocate the routine postoperative CT assessment of lumbar instrumented pedicle/screw fusions to allow for accurate confirmation of screw placement. The future introduction of a grading system to better facilitate decision making would be useful.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aoude AA, Fortin M, Figueiredo R, Jarzem P, Ouellet J, Weber MH. Methods to determine pedicle screw placement accuracy in spine surgery: A systematic review. Eur Spine J. 2015. 24: 990-1004
2. Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC. Accuracy of pedicle screw placement: A systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012. 21: 247-55
3. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. 33: 159-74
4. Tian N-F, Huang Q-S, Zhou P, Zhou Y, Wu R-K, Lou Y. Pedicle screw insertion accuracy with different assisted methods: A systematic review and meta-analysis of comparative studies. Eur Spine J. 2011. 20: 846-59
5. Zdichavsky M, Blauth M, Knop C, Graessner M, Herrmann H, Krettek C. Accuracy of Pedicle Screw Placement in Thoracic Spine Fractures: Part I: Inter- and Intraobserver Reliability of the Scoring System. Eur J Trauma. 2004. 30: 234-40
6. Zdichavsky M, Blauth M, Knop C, Lotz J, Krettek C, Bastian L. Accuracy of Pedicle Screw Placement in Thoracic Spine Fractures: Part II: A Retrospective Analysis of 278 Pedicle Screws Using Computed Tomographic Scans. Eur J Trauma. 2004. 30: 241-7