- Department of Surgery, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania
- Department of Neurosurgery, Muhimbili Orthopedic Institute, Dar es Salaam, Tanzania.
Correspondence Address:
Sylvery Mwesige, Department of Surgery, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
DOI:10.25259/SNI_1031_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sylvery Mwesige1, Maxigama Ndossi2, Nicephorus Rutabasibwa2, Laurent Lemeri2. Penetrating head trauma resulting from vigilante street justice. 15-Mar-2024;15:92
How to cite this URL: Sylvery Mwesige1, Maxigama Ndossi2, Nicephorus Rutabasibwa2, Laurent Lemeri2. Penetrating head trauma resulting from vigilante street justice. 15-Mar-2024;15:92. Available from: https://surgicalneurologyint.com/surgicalint-articles/12797/
Abstract
Background: Penetrating brain injury (PBI) can be caused by a variety of objects ranging from simple to complicated items. Nonetheless, it is strange and unusual to attack someone in the head with a long nail. Due to its rarity, care for them is still being developed and may include many steps.
Case Description: We are presenting a 35-year-old guy who was neurologically intact and hemodynamically stable but complained of headaches following a nail blow into the skull during a domestic altercation by a gang of individuals. A computed tomography scan revealed the metallic item inside the brain parenchyma. The patient recovered well from the procedure, which included the early removal of the foreign body, evacuation of the hematoma, and dura repair. Our objective is to demonstrate a few broad management concepts that help enhance patient outcomes. We covered the clinical manifestation and effective treatment of such a rare injury in this study.
Conclusion: Proper handling and rapid transport of patients to the advanced trauma center are crucial for victims of PBI. Timely and skilled interventions could prevent further nervous tissue damage and any related neurological dysfunction.
Keywords: Impacted foreign body, Penetrating brain injury, Vigilante justice
INTRODUCTION
Among trauma patients in Tanzania, traumatic brain damage is one of the main causes of morbidity and mortality. Due to the increase in motorcycle ridership, which has made motorcycles the primary form of public transportation in both urban and rural regions, it mostly impacts the young male age group. Assault is the third most prevalent cause of traumatic brain injury, behind collisions with vehicles and falls.[
Penetrating brain injury (PBI) constitutes a devastating and severe form of brain injury. Treatment for it might be difficult and have a bad consequence. Implementation, stabbing, explosions, and gunfire can all cause PBI. The severity of injury is determined by several factors including intracranial course, anatomical location, trajectory, energy, velocity, size, and kind of penetrating item.[
In situations when an object protrudes from the head, recommendations advise leaving it in place and stabilizing the patient throughout transport to avoid movement that might exacerbate cerebral vascular damage. It can only be taken out on receiving definitive treatment.
In radiological examination, a non-contrasted computed tomography (CT) is the preferred study to determine the degree of damage. Considering the likelihood of vascular injury, CT angiography (CTA) is also recommended.[
In PBI, the surgical procedure aims to safely remove the piled object while preserving function and avoiding any further damage.[
CASE PRESENTATION
From a local health institution, a 35-year-old male was referred to our facility (Tertiary Hospital). Six hours earlier, during a domestic incident, he had been struck in the skull with a nail, resulting in an unbearable headache.
Mechanism of injury
A gang of around twenty individuals is said to have arrested the young guy for stealing on the street. He was restrained on both his upper and lower limbs, and one of the attackers used a hammer to drive a nail into his brain.
Post incidence, there was no prior history of external bleeding, unconsciousness, vomiting, seizures, loss of hearing or vision, or weakness in the limbs. No comorbidities pre-existed.
Clinical evaluation
While lying supine on a stretcher, a focused examination revealed a nail was in situ in his skull near the midline, 2 cm posterior to the coronal suture, and 6 cm of the nail above the skin without external bleeding or clot. He had multiple shallow abrasions over the face, trunk, and upper and lower extremities.
His Glasgow coma score was 15, his pupils were normal in size and response to light, his cranial nerves were intact, had maximum strength in all limbs. Every vital sign was within normal range [
Radiological evaluation
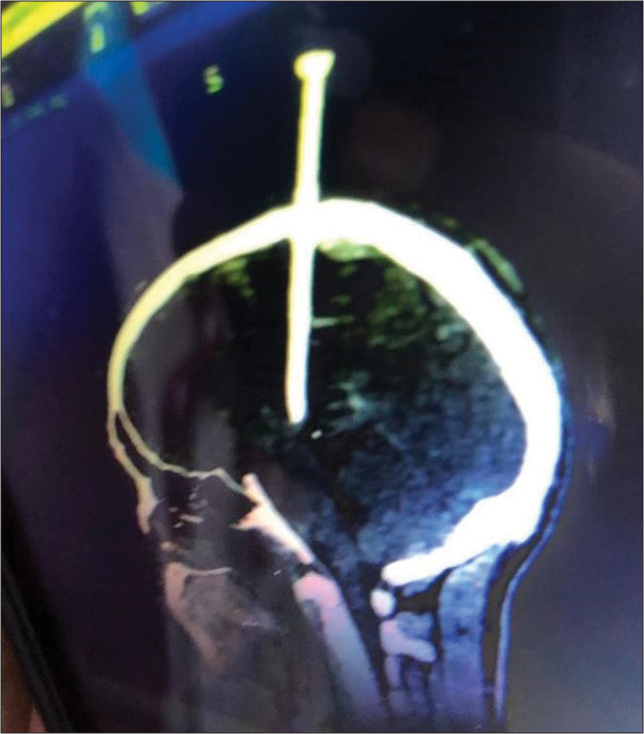
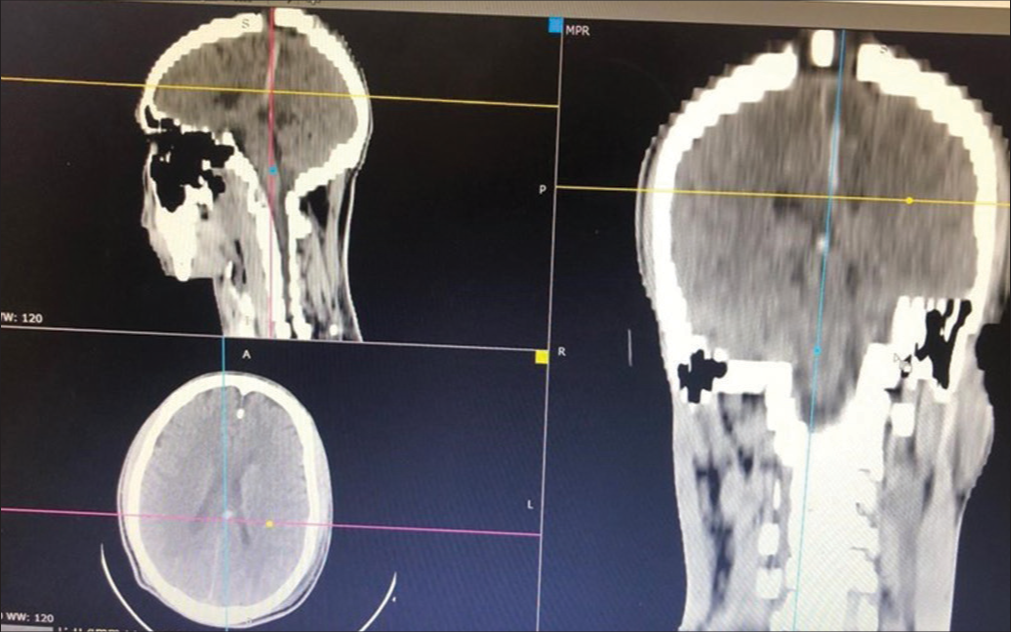
A metallic foreign body traveling through the parietal bone with an intracranial section of 9 cm and its tip immediately above the brain stem was discovered on a non-contrast sagittal CT scan. There was also edema along the tract and a sparse epidural hematoma. The ventricles and basal ganglia were unaffected. Preoperative CTA/computed tomography venography (CTV) was not done due to the patient’s financial status. Injury to the major vessel, such as the superior sagittal sinus, was unexpected because a plain CT scan already done at a peripheral hospital did not reveal a significant amount of intracranial bleeding [
Initial treatment
Prophylactic wide-spectrum antibiotics, IV fluids, tetanus vaccination, and analgesics were administered.
Surgical intervention
Under general anesthesia in the emergency operating room, a lineal incision and minor craniotomy were performed. The impacted nail was gently pulled off together with a bone flap. A little extradural hematoma was evacuated, washout with normal saline was done, and then the dura was repaired watertight. There was no evidence of damage to the larger intracranial blood vessels [
Postoperative care and outcome
Extubated on a table, the patient was admitted to the surgical intensive care unit and monitored closely. Antibiotics, strong painkillers, and prophylactic anticonvulsants were prescribed.
On the 1st postoperative day, the patient was fully conscious, ambulant, and had no focal neurological deficit.
From a control brain CT scan, there was no hematoma or edema along the foreign body tract, and he was discharged from the hospital two days later [
Clinical course and follow-up
There were no headaches, cerebrospinal fluid (CSF) leaks, seizures, or intracranial infections throughout the follow-up. On day 14 following the incident, a CTA was performed, and no aneurysms were found. Three months later, he was released from follow-up care.
DISCUSSION
Transcranial PBIs are less frequent but more recognizable. The Holy Bible describes the process of murdering someone by putting a nail into their head, particularly in the Book of Judges 4:21-22.[
The attacker, in this instance, was somewhat polite, unwittingly gave up, and refrained from driving a point home. More intracranial nail advancement would injure the brain stem and aggravate the situation since brain stem injuries impair important activities, including breathing, heart rate, and blood pressure.[
Penetrating head injuries may be associated with vascular injuries ranging from small cortical blood vessels to major ones. In our case, if there was a major vessel involvement. It would be the superior sagittal sinus. Many guidelines advocate performing neurovascular imaging such as CTA/ CTV preoperatively based on clinical judgment. In our case, neurovascular imaging was not employed due to the financial constraints of the uninsured patient; however, the pattern of injury from a plain CT scan done before arrival did not prompt the suspicion of major vessel injury.[
Surgical therapy generally aims to remove the impacted item and any associated necrotic material from the injury site, evacuate the hematoma, and reconstruct the dura watertight to prevent CSF leaking.
As in our illustration, it is advised that the object be removed along its route. Removing foreign objects roughly on the spot might end up in more serious consequences, such as uncontrollable bleeding and greater neurological damage.[
Surgical intervention may be necessary for low-velocity injuries due to the possibility of hematoma accumulation or protruding objects from the skull. In this instance, a nail that was embedded in the brain parenchyma and projecting externally required surgical therapy.[
In most cases, removing foreign objects from the brain helps avoid either acute or persistent intracranial infections. Neurological, mechanical, and functional impairments are further indicators.
The risk of collateral harm should be taken into account when considering surgical removal of a foreign body.
Under local anesthesia, it is sometimes possible to remove tiny, subdermal items. However, due to the possibility of severe bleeding on removal, cerebral edema, and further harm from the patient’s movements, general anesthesia is advisable for circumstances involving huge, deeply ingrained items.
For the preservation and repair of the surrounding anatomical components, effective planning of the foreign body removal procedure is essential. The greatest potential outcome in terms of neurological function and assuring appropriate rehabilitation can be attained with precise restoration of soft-tissue damage.[
CONCLUSION
Neurosurgeons are usually confronted with foreign bodies within the neurocranium. This case report highlights that PBI can occur with no neurological deficit. A minimally invasive approach can be employed to remove impacted objects after potentially associated injury to the major vessels has been ruled out.
Ethical approval
The Ethical approval was waived by our Institutional Review Board.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alao T, Waseem M, editors. Penetrating head trauma. StatPearls. Treasure Island, FL: StatPearls Publishing; 2017. p.
2. Kataria R, Singh D, Chopra S, Sinha VD. Low velocity penetrating head injury with impacted foreign bodies in situ. Asian J Neurosurg. 2011. 6: 39-44
3. Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011. 4: 395-402
4. Kee-Sampson JW, Gopireddy DR, Vulasala SS, Stein R, Kumar S, Virarkar M. Role of imaging in penetrating vascular injuries of the craniocervical region. J Clin Imaging Sci. 2022. 12: 63
5. Kiwango G, Msilanga D, Hocker M, Gerardo C, Lester R, Mvungi M. Epidemiology of traumatic brain injury patients at Kilimanjaro Christian Medical Centre, Moshi, Tanzania. Afr J Emerg Med. 2013. 3: S6
6. Salam AA, Eyres KS, Magides AD, Cleary J. Penetrating brain stem injury from crossbow bolt: A case report and review of the literature. Arch Emerg Med. 1990. 7: 224-7
7. Shi J, Mao Y, Cao J, Dong B. Management of screwdriver-induced penetrating brain injury: A case report. BMC Surg. 2017. 17: 3
8. Van Wolde E, editors. Deborah and Ya ‘El in judges 4. On reading prophetic texts. Netherlands: Brill; 1996. p. 283-95
9. Voss JO, Thieme N, Doll C, Hartwig S, Adolphs N, Heiland M. Penetrating foreign bodies in head and neck trauma: A surgical challenge. Craniomaxillofac Trauma Reconstr. 2018. 11: 172-82









Dr. Miguel A. Faria
Posted March 15, 2024, 10:16 am
This case seems to be more about anarchic street gangs and street thuggery than”vigilante justice.”