- Department of Neurosurgery, Yokohama Rosai Hospital, Yokohama, Japan.
- Department of Neuroendovascular Therapy, Yokohama Rosai Hospital, Yokohama, Japan.
Correspondence Address:
Fukutaro Ohgaki, Department of Neurosurgery, Yokohama Rosai Hospital, Yokohama, Japan.
DOI:10.25259/SNI_746_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fukutaro Ohgaki1, Nagatsuki Tomura2, Takashi Shuto1. Percutaneous transluminal angioplasty for vertebral artery origin stenosis under the flow-reversal protection using Mo.MA™ Ultra: A technical case report. 24-Nov-2023;14:406
How to cite this URL: Fukutaro Ohgaki1, Nagatsuki Tomura2, Takashi Shuto1. Percutaneous transluminal angioplasty for vertebral artery origin stenosis under the flow-reversal protection using Mo.MA™ Ultra: A technical case report. 24-Nov-2023;14:406. Available from: https://surgicalneurologyint.com/surgicalint-articles/12645/
Abstract
Background: Vertebral artery origin stenosis (VAOS) is a major cause of ischemic stroke of the posterior circulation. Aggressive medical treatment using dual antiplatelet therapy is the most common treatment approach to symptomatic VAOS; however, the effectiveness of endovascular treatment (EVT) for VAOS has recently been reported. Here, we report a case of VAOS treated with percutaneous transluminal angioplasty (PTA) under flow reversal protection using Mo.MA™ Ultra.
Case Description: The patient was a 78-year-old man. He underwent mechanical thrombectomy for acute right posterior cerebral artery occlusion, and recanalization was achieved. Subsequently, artery-to-artery (A-to-A) embolism caused by the right VAOS was revealed as the etiology. PTA under the flow-reversal protection using Mo.MA™ Ultra was performed electively, and the VAOS and antegrade flow of the right vertebral artery (VA) improved.
Conclusion: In EVT for symptomatic VAOS, lesion cross for distal protection device placement is considered to create a high risk of distal embolism due to the anatomic and clinicopathological characteristics of VAOS lesions, especially in A-to-A embolism cases. The flow-reversal protection using Mo.MA™ Ultra can be performed with EVT to prevent distal embolism with lesion cross by retrograde flow of the VA. This method is feasible, especially for cases in which antegrade flow to the basilar artery through the developed contralateral VA is anticipated during the Mo.MA™ Ultra protection.
Keywords: Embolic protection device, Flow-reversal protection, Mo.MA™ Ultra, Percutaneous transluminal angioplasty, Vertebral artery origin stenosis
INTRODUCTION
Vertebral artery origin stenosis (VAOS) is one of the most common causes of posterior circulation ischemic stroke, with a rate of approximately 15−20%.[
Aggressive medical management using dual antiplatelet therapy (DAPT) and endovascular treatment (EVT) have been reported for VAOS treatment; however, no evidence has revealed their superiority.[
In addition to this, although an embolic protection device (EPD) (Spider FX™, Medtronic, Dublin, Ireland) was used in a study,[
We report a case of VAOS in a patient who underwent percutaneous transluminal angioplasty (PTA) under flow-reversal protection using Mo.MA™ Ultra.
CASE DESCRIPTION
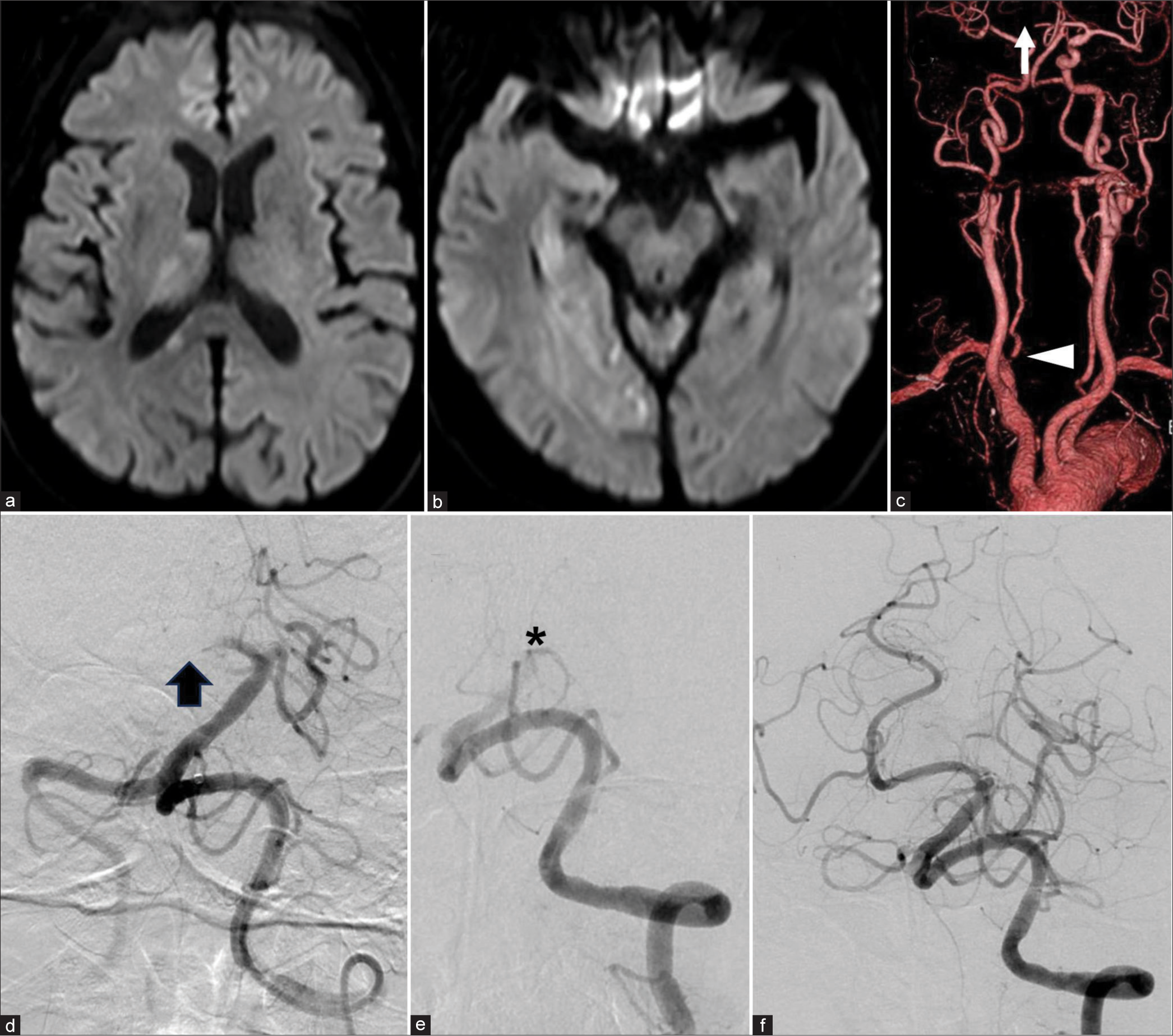
The patient was a 78-year-old man; he was well regarding activities of daily living (pretreatment modified Rankin Scale: 0). He had a medical history of high blood pressure. He presented with ambulation difficulty and consciousness disorder on waking and was transferred to our hospital. On admission, his Glasgow Coma Scale was 9 (E2V2M5), and he presented with left hemiparesis and hemispatial neglect with the National Institutes of Health Stroke Scale of 16. Magnetic resonance imaging (MRI) and computed tomographic angiography (CTA) revealed acute cerebral infarction caused by occlusion of the P1 segment of the right posterior cerebral artery (PCA) with a suspicious finding of the right VAOS [
Figure 1:
(a-c) Magnetic resonance imaging on admission revealed acute cerebral infarction in the PCA territory. A mismatch was detected between the high-intensity area of the diffusion-weighted image and the right P1 segment occlusion (c, arrow) with the right vertebral artery origin stenosis (c, arrowhead) shown by computed tomographic angiography. (d-f) MT was performed for the P1 segment of the right PCA occlusion (d, arrow). During MT, recanalization of PCA was accomplished once, but basilar artery occlusion occurred (e, asterisk). Recanalization of the thrombolysis index cerebral infarction score 2b was obtained (f).PCA: posterior cerebral artery, MT: Mechanical thrombectomy.
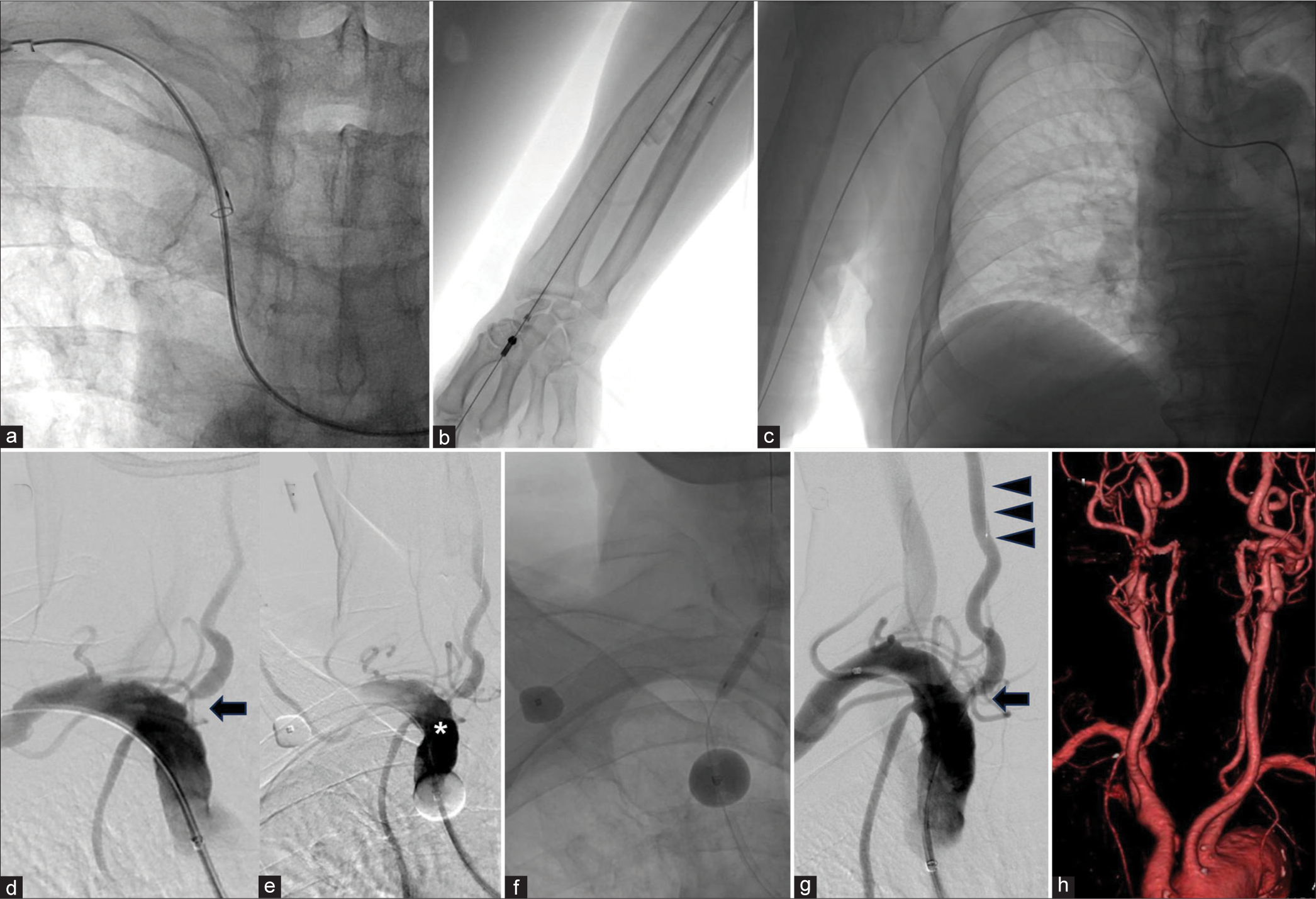
DAPT was used to prevent the recurrence of the A-to-A embolism, and PTA for VAOS was performed electively at 20 days after onset. Anterograde flow persisted, and distal embolism was a concern. In addition, this was a symptomatic lesion that had developed A-to-A embolism once, and recurrence of A-to-A embolism with the lesion cross was concerned. Therefore, we decided to perform flow-reversal protection using the Mo.MA™ Ultra (Medtronic, Dublin, Ireland). Pretreatment CTA showed type III aortic arch and prominent tortuosity of the right brachiocephalic artery (BRCA), which was selected as the approach route; therefore, we presumed that it would be difficult to place Mo.MA™ Ultra. Consequently, we used the snare traction technique [
Figure 2:
(a-c) For the Mo.MA™ Ultra placement, the traction route of Radifocus® stiff wire, was made using Amplatz Goose Neck™ Microsnare because its tortuosity was prominent. In digital subtraction angiography, (d) VAOS was evident (arrow) and considered the cause of the A-to-A embolism. (e) Under the flow-reversal protection, contrast agent pooled (asterisk) by retrograde flow from the right VA. (f and g) Percutaneous transluminal angioplasty was performed, leading to an improvement of VAOS (g, arrow) and antegrade flow of the right VA (g, arrowhead). (h) The patency of VAOS in the right VA was confirmed by follow-up computed tomographic angiography. A-to-A: Artery to artery, VA: Vertebral artery, VAOS: Vertebral artery origin stenosis.
First, we punctured the left common femoral artery and placed a 9Fr super sheath (Terumo, Tokyo, Japan). Using a 4Fr SIM2 120 cm (Medikit, Tokyo, Japan)/Guidewire surf 0.035 180 cm (Piolax, Kanagawa, Japan), we selected the right BRCA. Then, we punctured the right radial artery (RA) and placed a 5Fr short sheath (Terumo, Tokyo, Japan). Using the right RA route, we placed a SIM 2 in the right brachial artery using an Amplatz Goose Neck™ Microsnare (Medtronic, Dublin, Ireland) [
No evidence of treatment-related infarction was detected on the follow-up MRI, and the improvement in the patency of the right VAOS was maintained [
DISCUSSION
Recently, several studies have reported the efficacy of EVT for VAOS.[
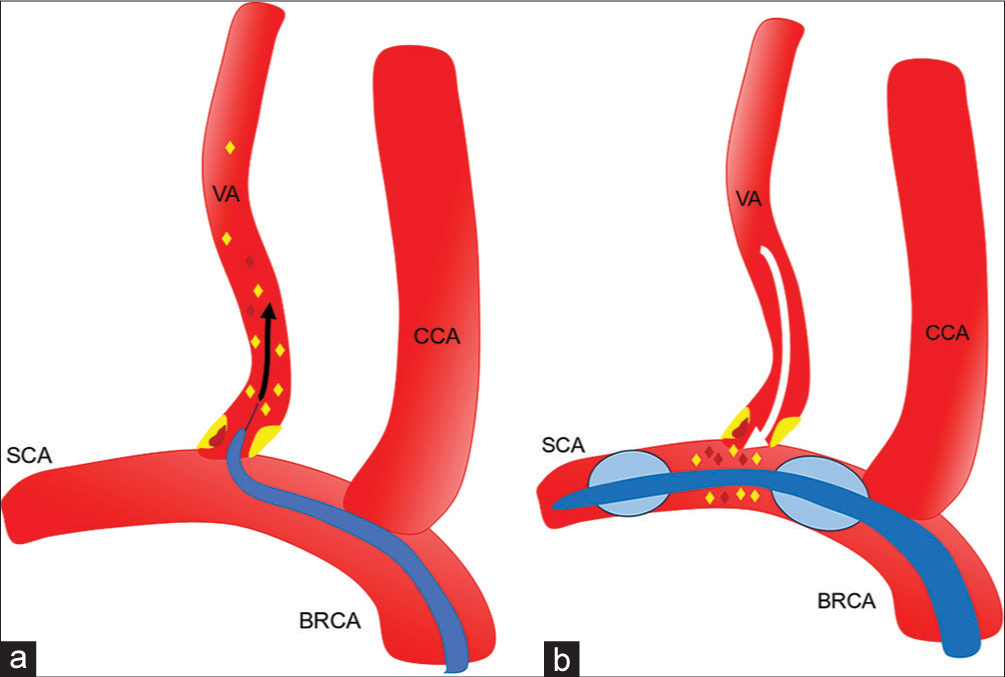
Figure 3:
(a) Schema of distal embolism (yellow rhombus: Plaque debris; wine-red rhombus: Thrombus; black arrow: scattering with antegrade flow) with the VAOS lesion cross by distal protection device. (b) Schema of flow-reversal protection using Mo.MA™ Ultra. Antegrade flow from the right BRCA and retrograde flow from the right SCA were obstructed by balloon inflation. Prevention of a distal embolism (yellow rhombus: Plaque debris, wine-red rhombus: Thrombus) in VA lesion cross is possible by retrograde flow from the right VA through the union (arrow). BRCA: Brachiocephalic artery, CCA: Common carotid artery, SCA: Subclavian artery, VA: Vertebral artery, VAOS: Vertebral artery origin stenosis.
Furthermore, this patient’s aortic arch was type III, Mo.Ma™ Ultra was considered suitable for a stable catheter placement [
However, as a limitation of this method, the flow-reversal protection is confined in cases of well-developed contralateral VA because complete obstruction of antegrade flow is required with Mo.MA™ Ultra. Therefore, cases with poor contralateral VA development or both sides of lesions are inappropriate for this method. In addition to this, when the distance between the origin of the VA and the common carotid artery is insufficient, flow-reversal protection using the Mo.MA™ Ultra is difficult [
CONCLUSION
PTA effectively prevents stroke recurrence with symptomatic VAOS. In addition to this, the flow-reversal protection using Mo.MA™ Ultra can be performed with EVT to prevent distal embolism with lesion cross by retrograde flow of the VA. This method is feasible, especially for cases where antegrade flow through the developed contralateral VA is anticipated during the Mo.MA™ Ultra protection.
Ethical approval
Not applicable.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chaturvedi S. Vertebral artery stenting: Lifting the therapeutic fog. Lancet Neurol. 2019. 18: 620-1
2. Compter A, van der Worp HB, Schonewille WJ, Vos JA, Boiten J, Nederkoorn PJ. Stenting versus medical treatment in patients with symptomatic vertebral artery stenosis: A randomised open-label phase 2 trial. Lancet Neurol. 2015. 14: 606-14
3. Gruber P, Berberat J, Kahles T, Anon J, Diepers M, Nedeltchev K. Angioplasty using drug-coated balloons in ostial vertebral artery stenosis. Ann Vasc Surg. 2020. 64: 157-62
4. Gulli G, Marquardt L, Rothwell PM, Markus HS. Stroke risk after posterior circulation stroke/transient ischemic attack and its relationship to site of vertebrobasilar stenosis: Pooled data analysis from prospective studies. Stroke. 2013. 44: 598-604
5. Haghighi AB, Edgell RC, Cruz-Flores S, Zaidat OO. Vertebral artery origin stenosis and its treatment. J Stroke Cerebrovasc Dis. 2011. 20: 369-76
6. Kim YJ, Lee JH, Choi JW, Roh HG, Chun YI, Lee JS. Long-term outcome of vertebral artery origin stenosis in patients with acute ischemic stroke. BMC Neurol. 2013. 13: 171
7. Li L, Wang X, Yang B, Wang Y, Gao P, Chen Y. Validation and comparison of drug eluting stent to bare metal stent for restenosis rates following vertebral artery ostium stenting: A single-center real-world study. Interv Neuroradiol. 2020. 26: 629-36
8. Shao JX, Ling YA, Du HP, Zhai GJ, Xu Y, Cao YJ. Comparison of hemodynamic changes and prognosis between stenting and standardized medical treatment in patients with symptomatic moderate to severe vertebral artery origin stenosis. Medicine (Baltimore). 2019. 98: e14899
9. Thompson MC, Issa MA, Lazzaro MA, Zaidat OO. The natural history of vertebral artery origin stenosis. J Stroke Cerebrovasc Dis. 2014. 23: e1-4
10. Wang MY, Wang F, Liu YS, Yu LJ. Comparison of drug-coated balloons to bare metal stents in the treatment of symptomatic vertebral artery-origin stenosis: A prospective randomized trial. World Neurosurg. 2021. 154: e689-97
11. Wang Z, Ling Y, Zhao H, Mao Y, Dong Q, Cao W. A comparison of different endovascular treatment for vertebral artery origin stenosis. World Neurosurg. 2022. 164: e1290-7
12. Wityk RJ, Chang HM, Rosengart A, Han WC, DeWitt LD, Pessin MS. Proximal extracranial vertebral artery disease in the New England medical center posterior circulation registry. Arch Neurol. 1998. 55: 470-8
13. Wu S, Yin Y, Li Z, Li N, Ma W, Zhang L. Using drug-coated balloons for symptomatic vertebral artery origin stenosis: A systematic review and meta-analysis. J Clin Neurosci. 2023. 107: 98-105
14. Zhou Z, Yin Q, Xu G, Yue X, Zhang R, Zhu W. Influence of vessel size and tortuosity on in-stent restenosis after stent implantation in the vertebral artery ostium. Cardiovasc Intervent Radiol. 2011. 34: 481-7