- Department Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Shahbag, Dhaka, Bangladesh.
DOI:10.25259/SNI_212_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Md. Kamrul Ahsan, Om Prakash Pandit, Md. Shahidul Islam Khan. Percutaneous vertebroplasty for symptomatic osteoporotic compression fractures: A single–center prospective study. 19-Apr-2021;12:176
How to cite this URL: Md. Kamrul Ahsan, Om Prakash Pandit, Md. Shahidul Islam Khan. Percutaneous vertebroplasty for symptomatic osteoporotic compression fractures: A single–center prospective study. 19-Apr-2021;12:176. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10731
Abstract
Background: Osteoporotic vertebral compression fractures (OVCFs) increasingly occur with advancing age, and are associated with significant morbidity, mortality, and cost. We assessed the clinical efficacy, radiological, and functional outcomes for patients undergoing percutaneous vertebroplasty (PVP) due to OVCFs, with a special focus on the frequency of new vertebral compression fractures (VCFs).
Methods: This study, carried from 2018 to 2020, included 22 females and 4 males. They averaged 60.15 years of age (range, 50–70) were followed an average of 14.5 months (range 12–36 months), and had 30 VCFs between the T7–L2 levels. Multiple variables were studied, including; anterior vertebral height (AVH) and kyphotic angle (KA), new VCFs, and functional outcomes.
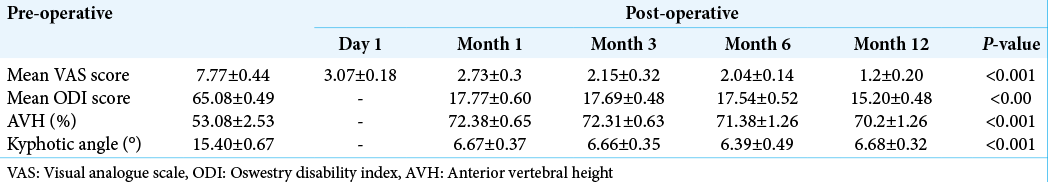
Results: The postoperative Visual Analog Scale and Oswestry Disability Index were significantly reduced at 12 months after PVP. Improvements for AVH and KA were also statistically significant; 23 patients (88.46%) had a dramatic decrease in pain on post-operative day 1, while 3 patients (11.53%) had no decrease in pain after PVP on post-operative day 1–1 postoperative month. No major complications were observed except high incidence of cement leakage at 8 levels (26.67%) in 6 patients. Additionally, new VCFs occurred in 10 vertebrae in 8 patients (30.76%), involving 6 adjacent (60%), and 4 nonadjacent vertebrae (40%).
Conclusion: PVP is an effective procedure in the management of painful OVCFs refractory to medical treatment. These PVP procedures yield immediate vertebral stabilization, relieve pain, and restore function with minimal associated morbidity.
Keywords: Bone cement, Compression fracture, Osteoporosis, Vertebroplasty
INTRODUCTION
Approximately 3–16% of women and 1–8% of men aged >50 years are reported to have sustained a clinically symptomatic vertebral compression fracture (VCF).[
MATERIALS AND METHODS
Clinical variables
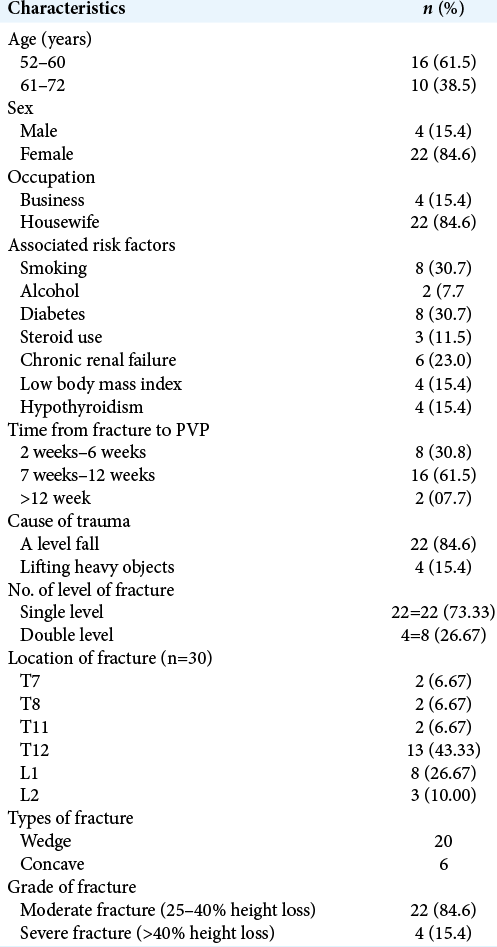
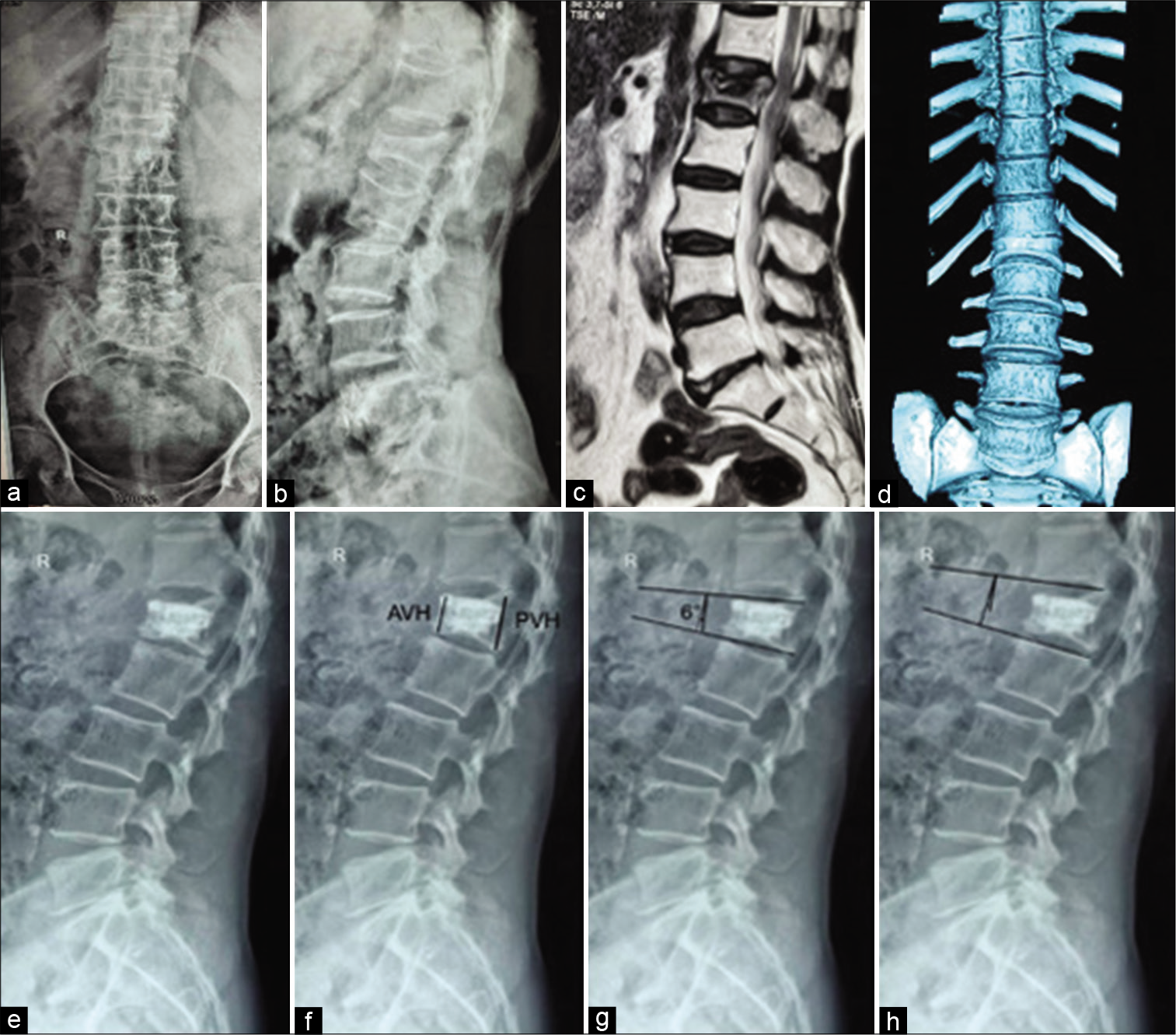
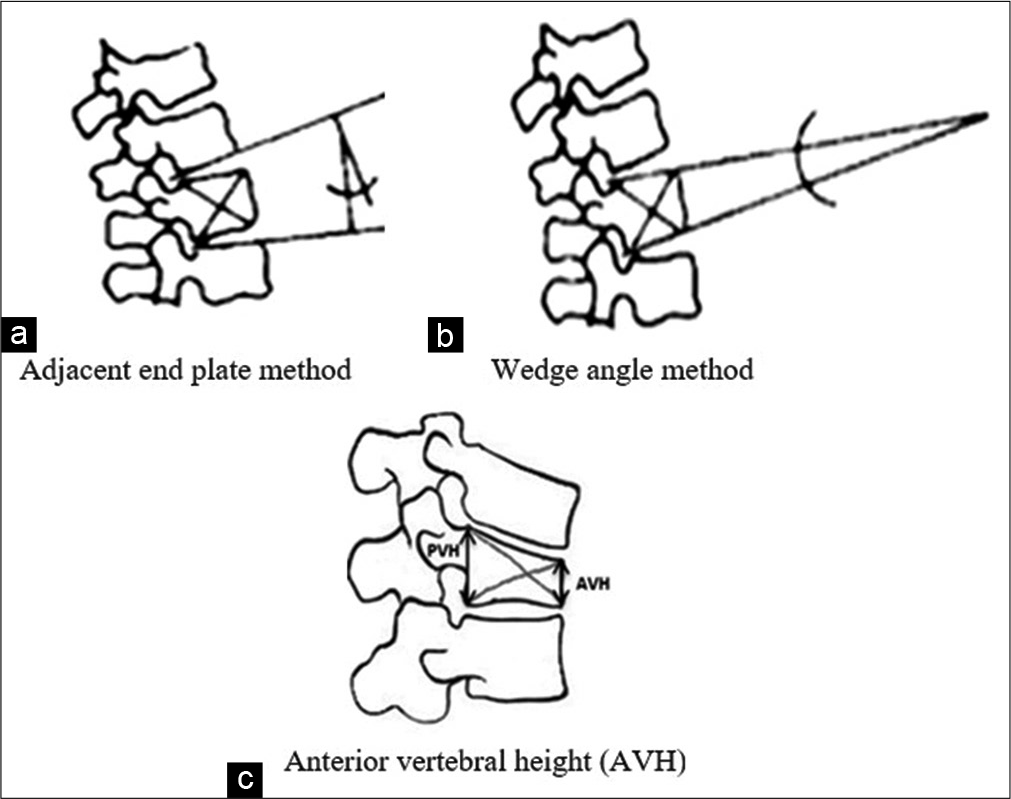
With Institutional Review Board approval, (2018–2020) we retrospectively reviewed the charts of 22 females and 4 males with OVCS. Patients averaged 60.15 years of age, the mean follow-up period was 14.5 months, and exhibited 30 VCFs (T7–L2) [
Radiological work up
All patients underwent radiological assessment (plain X-rays, computed tomography [CT], and Magnetic resonance imaging [MRI] scans) plus laboratory investigations [
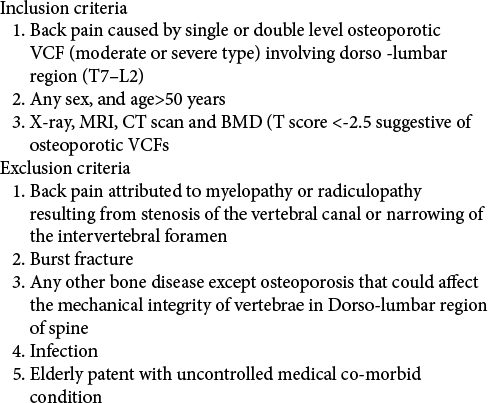
Figure 1:
72-year-old lady underwent percutaneous vertebroplasty following osteoporotic vertebral compression fracture (VCF) at L1 level on July 28, 2018 after 8 weeks of onset of symptoms. (a and b) plain X-ray lumbosacral spine shows compression fracture L1, (c-d) T2 weighted sagittal view magnetic resonance imaging and computed tomography scan showing VCF and (e-h) shows subsequent follow up at 1, 3, 6 and at 12 months, and measurement of anterior vertebral height (increased 70% at 12 month) and kyphotic angle decrease from 15 to 6 degree.
Outcome evaluation
Postoperatively, patients were evaluated utilizing Visual Analog Scale (VAS), Oswestry Disability Index (ODI) score, and radiological parameters (anterior vertebral height [AVH], kyphotic angle [KA]; plain standing X-rays on 1 day and 1, 4, 6, 12 months, and yearly thereafter) [
Figure 2:
Measurement technique for assessing fracture kyphosis (a and b) and anterior vertebral height (c). Segmental kyphosis (a) was assessed by measuring the angle between the inferior end plate of the upper vertebra and superior end plate of the lower vertebra and vertebral kyphosis (b) by measuring the angle between the two end plates of the fractured vertebra
PVP procedure
Routine PVP were performed under general anesthesia or local anesthesia using a C-arm. Bilateral cannulations were favored due to increase the likelihood of adequate/ safer cement injections. The routine procedures were then performed.
Statistical analysis
The quantitative data were analyzed statistically using Statistical Package for the Social Science, version 25, Armonk, NY, INM Corp. Statistical significance was set at P < 0.05 and confidence interval set at 95% level. Continuous variable was expressed as mean with standard deviation and categorical variables as frequency with percentage. Numerical data were assessed by paired t-test.
RESULTS
The mean post-operative VASs and ODI scores were significantly reduced at 12 months after PVP [
DISCUSSION
The efficacy of PVP in decreasing pain has been reported to be 60–90%.[
The amount of cement used during the PVP procedure is critical for its success. Recently it has been mentioned that 16% of the vertebral corpus volume should be augmented in order to balance the distribution of stress over the vertebra.[
A major problem that occurs after PVP is a new fracture in adjacent vertebra. A meta-analysis demonstrated that incidence of new fractures after PVP was 8–52%[
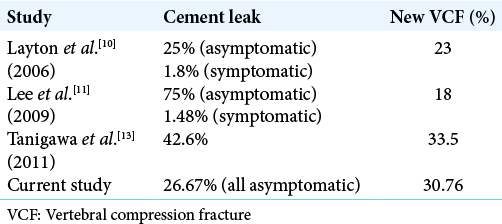
Vertebroplasty has a complication rate of 1–3%. The most frequently reported complications are cement extravasation. There were no major complications in the present study despite a relatively high incidence of cement leakage at 8 levels (26.67%). New VCFs occurred 10 vertebrae in 8 patients (30.76%), and one patient exhibited progressive kyphotic deformity (3.84%). In Lee et al.[
PVP is a procedure that improve stability and pain relief, and but have been associated with new fractures of adjacent vertebra versus conservative pain management.[
CONCLUSION
PVP is a safe and effective procedure in the management of painful OVCFs refractory to medical treatment. This procedure can be performed rapidly and is alternative to open surgeries in patients with comorbidities.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Blasco J, Martinez-Ferrer A, Macho J, San Roman L, Pomés J, Carrasco J. Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: A 12-month randomized follow-up, controlled trial. J Bone Miner Res. 2012. 27: 1159-66
2. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009. 361: 557-68
3. Esses SI, McGuire R, Jenkins J, Finkelstein J, Woodard E, Watters WC. The treatment of symptomatic osteoporotic spinal compression fractures. J Am Acad Orthop Surg. 2011. 19: 176-82
4. Heini PF, Wälchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: Operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 2000. 9: 445-50
5. Hu MM, Eskey CJ, Tong SC, Nogueira RG, Pomerantz SR, Rabinov JD. Kyphoplasty for vertebral compression fracture via a uni-pedicular approach. Pain Physician. 2005. 8: 363-7
6. Hulme PA, Krebs J, Ferguson SJ, Berlemann U. Vertebroplasty and kyphoplasty: A systematic review of 69 clinical studies. Spine (Phila Pa 1976). 2006. 31: 1983-2001
7. Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: Technical aspects. AJNR Am J Neuroradiol. 1997. 18: 1897-904
8. Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporosis Int. 2005. 16: S3-7
9. Kamano H, Hiwatashi A, Kobayashi N, Fuwa S, Takahashi O, Saida Y. New vertebral compression fractures after prophylactic vertebroplasty in osteoporotic patients. AJR Am J Roentgenol. 2011. 197: 451-6
10. Layton KF, Thielen KR, Koch CA, Luetmer PH, Lane JI, Wald JT. Vertebroplasty, first 1000 levels of a single center: Evaluation of the outcomes and complications. AJNR Am J Neuroradiol. 2007. 28: 683-9
11. Lee MJ, Dumonski M, Cahill P, Stanley T, Park D, Singh K. Percutaneous treatment of vertebral compression fractures: A meta-analysis of complications. Spine (Phila Pa 1976). 2009. 34: 1228-32
12. Luo J, Daines L, Charalambous A, Adams MA, Annesley-Williams DJ, Dolan P. Vertebroplasty: Only small cement volumes are required to normalize stress distributions on the vertebral bodies. Spine (Phila Pa 1976). 2009. 34: 2865-73
13. Tanigawa N, Kariya S, Komemushi A, Nakatani M, Yagi R, Kohzai M. Percutaneous vertebroplasty for osteoporotic compression fractures: Long-term evaluation of the technical and clinical outcomes. AJR Am J Roentgenol. 2011. 196: 1415-8
14. Trout AT, Kallmes DF, Kaufmann TJ. New fractures after vertebroplasty: Adjacent fractures occur significantly sooner. AJNR Am J Neuroradiol. 2006. 27: 217-23
15. Zhang Z, Fan J, Ding Q, Wu M, Yin G. Risk factors for new osteoporotic vertebral compression fractures after vertebroplasty: A systematic review and meta-analysis. J Spinal Disord Tech. 2013. 26: E150-7