- Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief Surgical Neurology International NY and c/o Dr. Marc Agulnick 1122 Franklin Avenue Suite 106, Garden City, NY 11530 ,United States.
Correspondence Address:
Nancy E Epstein, M.D., F.A.C.S., Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief Surgical Neurology International NY and c/o Dr. Marc Agulnick 1122 Franklin Avenue Suite 106, Garden City, NY 11530, United States.
DOI:10.25259/SNI_671_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E Epstein. Perspective: Can intraoperative neurophysiological monitoring (IONM) limit errors associated with lumbar pedicle screw fusions/transforaminal lumbar interbody fusions (TLIF)?. 08-Sep-2023;14:314
How to cite this URL: Nancy E Epstein. Perspective: Can intraoperative neurophysiological monitoring (IONM) limit errors associated with lumbar pedicle screw fusions/transforaminal lumbar interbody fusions (TLIF)?. 08-Sep-2023;14:314. Available from: https://surgicalneurologyint.com/surgicalint-articles/12543/
Abstract
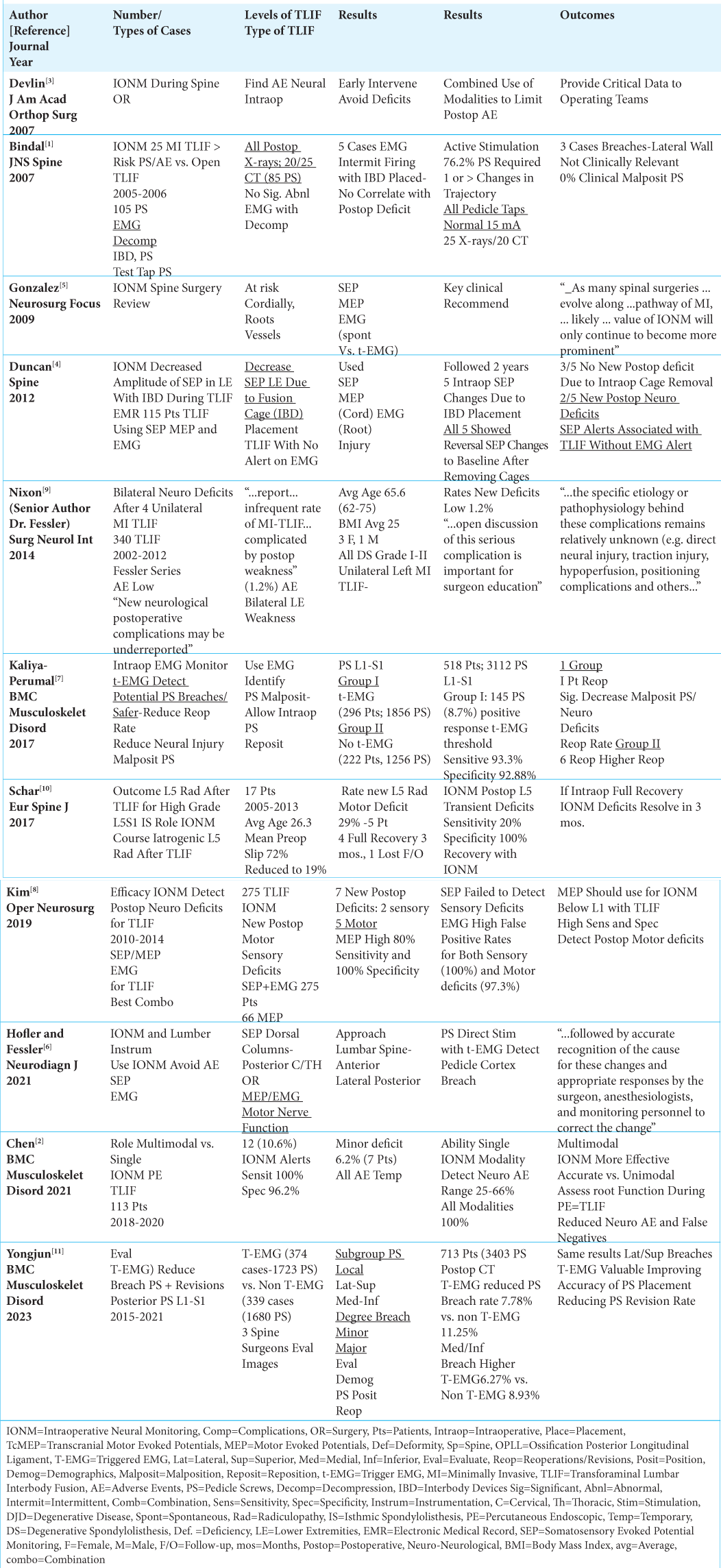
Background: We evaluated whether intraoperative neural monitoring (IONM), including somatosensory evoked potential monitoring (SEP), motor evoked potential monitoring (MEP), and electrophysiological monitoring (EMG), could reduce operative errors attributed to lumbar instrumented fusions, including minimally invasive (MI) transforaminal lumbar interbody fusion (TLIF)/open TLIF.
Methods: Operative errors included retraction/stretch or cauda equina neural/cauda equina injuries that typically occurred during misplacement of interbody devices (IBD) and/or malpositioning of pedicle screws (PS).
Results: IONM decreased the incidence of intraoperative errors occurring during instrumented lumbar fusions (MI-TLIF/TLIF). In one series, significant loss of intraoperative SEP in 5 (4.3%) of 115 patients occurred after placing IBD; immediate removal of all IBD left just 2 patients with new neural deficits. In other series, firing of trigger EMG’s (t-EMG) detected intraoperative PS malpositioning, prompted the immediate redirection of these screws, and reduced the need for reoperations. One t-EMG study required a reoperation in just 1 of 296 patients, while 6 reoperations were warranted out of 222 unmonitored patients. In another series, t-EMG reduced the pedicle screw breech rate to 7.78% (1723 PS) from a higher 11.25% for 1680 PS placed without t-EMG. A further study confirmed that MEP’s picked up new motor deficits in 5 of 275 TLIF.
Conclusion: SEP/MEP/EMG intraoperative monitoring appears to reduce the risk of surgical errors when placing interbody devices and PS during the performance of lumbar instrumented fusions (MI-TLIF/TLIF).However, IONM is only effective if spine surgeons use it, and immediately address significant intraoperative changes.
Keywords: Transforaminal Lumbar Interbody Fusions, Surgical errors, Malpositioning Pedicle Screws, Interbody Devices, Retraction Neural Injuries, Intraoperative Monitoring, Somatosensory Evoked Potentials (SEP), Electromyography (EMG), Motor Evoked Potentials (MEP), Minimally Invasive (MI) TLIF
INTRODUCTION
Can intraoperative neurophysiological monitoring (IONM) limit surgical errors (i.e. particularly attributed to placing interbody devices (IBD), or pedicle screws (PS)) during instrumented pedicle/screw fusions, including open/minimally invasive (MI) transforaminal lumbar interbody fusions (MI-TLIF/TLIF)?[
Multimodal IONM Limits Postoperative Deficits and Reoperation Rates
Multiple rather than single IONM modalities utilized during instrumented lumbar pedicle screw fusions (PS) utilized during MI-TLIF/TLIF, better identify impending intraoperative neural injury/surgical errors; however they must prompt surgeons to perform immediate intraoperative resuscitative maneuvers to limit/avoid new postoperative neurological deficits [
Passive and Active t-EMG Limits Errors of Lumbar PS Fusions (MI-TLIF/Open TLIF)
Passive and active EMG (i.e., trigger EMG (t-EMG)) alerts increased the accuracy for detecting intraoperative PS misplacement, often prompting immediate screw redirection, and reducing the incidence of postoperative reoperations required to address malpositioned screws [
Significant SEP Decreases/Alerts During IBD Placement in 5 of 115 TLIF Patients Prompted Immediate IBD Removal and Averted Deficits in 3 Patients
When Duncan et al. (2012) performed 115 TLIF, 5 patients developed significant decreases (alerts) in SEP amplitude without EMG changes following the placement of IBD [
IONM Reduces Errors Occurring in MI-TLIF/Open TLIF Surgery
MI-TLIF/Open TLIF studies documented the reduction of intraoperative errors utilizing IONM [
CONCLUSION
Significant intraoperative IONM alerts prompted immediate intraoperative resuscitative maneuvers (i.e. reduction of retraction, stretching, IBD removal and/or PS redictection/ repositioning) to limit operative errors attributed to instrumented lumbar PS fusions (MI-TLIF/Open TLIF) [
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-Assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bindal RK, Ghosh S. Intraoperative electromyography monitoring in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine. 2007. 6: 126-32
2. Chen Y, Luo C, Wang J, Liu L, Huang B, Li CQ. Roles of multimodal intra-operative neurophysiological monitoring (IONM) in percutaneous endoscopic transforaminal lumbar interbody fusion: A case series of 113 patients. BMC Musculoskelet Disord. 2021. 22: 989
3. Devlin VJ, Schwartz DM. Intraoperative neurophysiologic monitoring during spinal surgery. J Am Acad Orthop Surg. 2007. 15: 549-60
4. Duncan JW, Bailey RA, Baena R. Intraoperative decrease in amplitude of somatosensory-evoked potentials of the lower extremities with interbody fusion cage placement during lumbar fusion surgery. Spine (Phila Pa 1976). 2012. 37: E1290-5
5. Gonzalez AA, Jeyanandarajan D, Hansen C, Zada G, Hsieh PC. Intraoperative neurophysiological monitoring during spine surgery: A review. Neurosurg Focus. 2009. 27: E6
6. Hofler RC, Fessler RG. Intraoperative neuromonitoring and lumbar spinal instrumentation: Indications and utility. Neurodiagn J. 2021. 61: 2-10
7. Kaliya-Perumal AK, Charng JR, Niu CC, Tsai TT, Lai PL, Chen LH. Intraoperative electromyographic monitoring to optimize safe lumbar pedicle screw placement-a retrospective analysis. BMC Musculoskelet Disord. 2017. 18: 229
8. Kim JH, Lenina S, Mosley G, Meaike J, Tran B, Kim JS. The efficacy of intraoperative neurophysiological monitoring to detect postoperative neurological deficits in transforaminal lumbar interbody fusion surgery. Oper Neurosurg (Hagerstown). 2019. 16: 71-8
9. Nixon AT, Smith ZA, Lawton CD, Wong AP, Dahdaleh NS, Koht A. Bilateral neurological deficits following unilateral minimally invasive TLIF: A review of four patients. Surg Neurol Int. 2014. 5: S317-24
10. Schär RT, Sutter M, Mannion AF, Eggspühler A, Jeszenszky D, Fekete TF. Outcome of L5 radiculopathy after reduction and instrumented transforaminal lumbar interbody fusion of high-grade L5-S1 isthmic spondylolisthesis and the role of intraoperative neurophysiological monitoring. Eur Spine J. 2017. 26: 679-90
11. Yongjun T, Yuntian Z, Biao C, Zenghui J. Intraoperative triggered electromyographic monitoring of pedicle screw efficiently reduces the lumbar pedicle breach and re-operative rate-a retrospective analysis based on postoperative computed tomography scan. BMC Musculoskelet Disord. 2023. 24: 535