- Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook and Editor-in-Chief Surgical Neurology International NY, USA, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA,
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA, 1122 Frankling Avenue Suite 106, Garden City, NY, USA.
Correspondence Address:
Nancy E. Epstein, M.D., F.A.C.S., Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief of Surgical Neurology International NY, USA, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA.
DOI:10.25259/SNI_61_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Perspective: Cervical laminoforaminotomy (CLF) is safer than anterior cervical diskectomy/fusion (ACDF) for lateral cervical disease. 16-Feb-2024;15:50
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Perspective: Cervical laminoforaminotomy (CLF) is safer than anterior cervical diskectomy/fusion (ACDF) for lateral cervical disease. 16-Feb-2024;15:50. Available from: https://surgicalneurologyint.com/surgicalint-articles/12752/
Abstract
Background: The literature documents that laminoforaminotomy (CLF), whether performed open, minimally invasively, or microendoscopically, is safer than anterior cervical diskectomy/fusion (ACDF) for lateral cervical disease.
Methods: ACDF for lateral cervical disc disease and/or spondylosis exposes patients to multiple major surgical risk factors not encountered with CLF. These include; carotid artery or jugular vein injuries, esophageal tears, dysphagia, recurrent laryngeal nerve injuries, tracheal injuries, and dysphagia. CLF also exposes patients to lower rates of vertebral artery injury, dural tears (DT)/cerebrospinal fluid fistulas, instability warranting fusion, adjacent segment disease (ASD), plus cord and/or nerve root injuries.
Results: Further, CLF vs. ACDF for lateral cervical pathology offer reduced tissue damage, operative time, estimated blood loss (EBL), length of stay (LOS), and cost.
Conclusion: CLFs’, whether performed open, minimally invasively, or microendoscopically, offer greater safety, major pros with few cons, and decreased costs vs. ACDF for lateral cervical disease.
Keywords: Cervical Laminoforaminotomy (CLF), Safety, Reduced Cost, Disc Disease, Spondylosis, Lateral Recess Stenosis, Reduced Morbidity, Preservation Stability, Lack of Fusion, Anterior Cervical Diskectomy/Fusion (ACDF)
INTRODUCTION
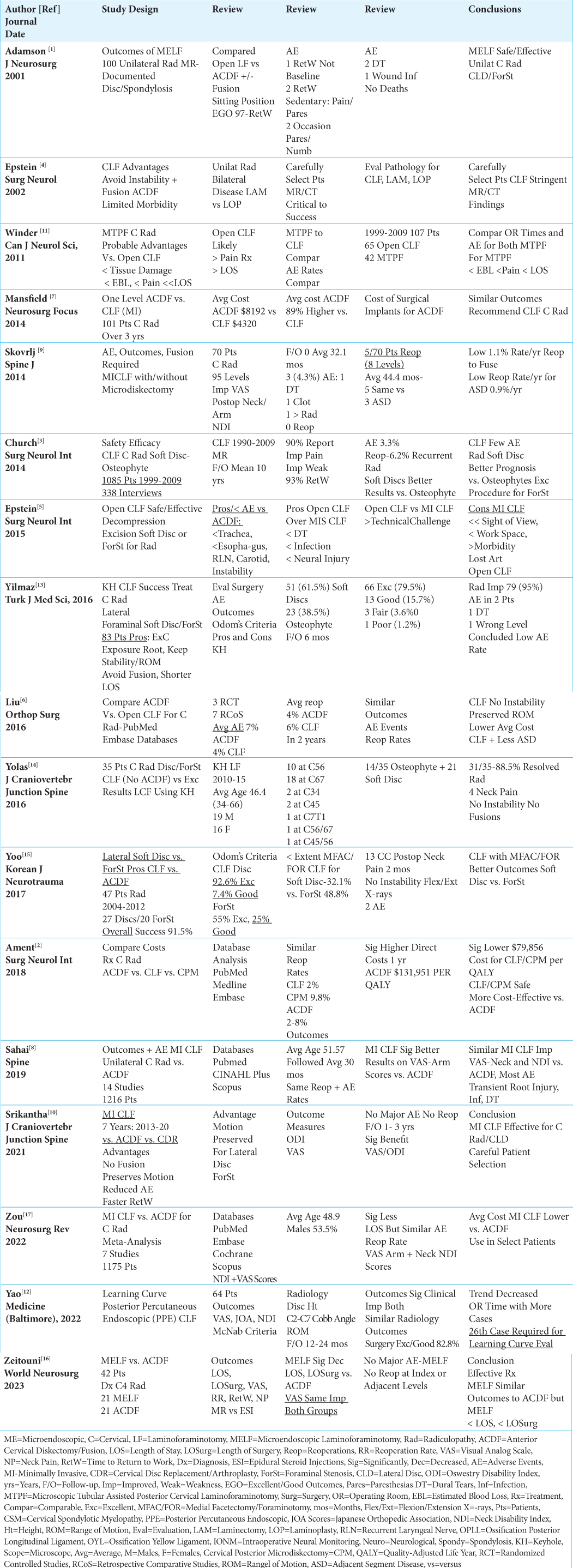
Cervical laminoforaminotomy (CLF), whether performed open, minimally invasively (MI), or microendoscopically (ME) for lateral/foraminal cervical disc disease, are safer than anterior cervical diskectomy/fusion (ACDF) [
Pros with Few Cons for Open Cervical Lamoinoforaminotomy (CLF) vs. ACDF for Lateral Cervical Disc/Spondylosis
Several studies emphasized the multiple pros without significant cons for performing open CLF vs. predominantly ACDF for addressing lateral cervical disc disease/spondylosis [
Good/Excellent Postoperative Outcomes with Limited Adverse Events for Open CLF
Three studies documented good/excellent postoperative outcomes with limited reports of adverse events following open CLF [
Microscopic Tubular Assisted Posterior Cervical Laminoforaminotomy (MTPF) vs. Open CLF
Winder et al. (2011) compared the results for MTPF (42 patients) vs. open CLF (65 patients) for patients with lateral cervical disease; although both groups sustained comparable perioperative AE, and operating room times, MTPF reduced tissue damage, intraoperative blood loss, postoperative pain, and LOS [
Results for Minimally Invasive CLF (MICLF) vs. ACDF for Lateral Cervical Discs/Osteophytes
Three studies described better outcome scores and reduced length of stay (LOS) for MICLF over ACDF [
Success of Microendoscopic Laminoforaminotomy (MELF) for Lateral Cervical Disease
Two series showed that MELF were safe and effective, with MELF and ACDF yielding comparable results when addresssing lateral cervical disease [
Learning Curve for Percutaneous Endoscopic CLF (PPE CLF) Procedures Requires Performing the First 26 of the 64 Cases
Yao et al. (2022) determined that the learning curve for PPE CLF procedures occurred after the first 26 of 64 cases (i.e., before surgeons showed a “trend” for decreased operating room time and greater “proficiency”); this further correlated with an overall 82.8% incidence of good/excellent outcomes for the 65 patients at 12-24 postoperative months [
Lower Cost for Open CLF, Posterior Cervical Foraminotomy/Cervical Posterior Microdiskectomy (PCF/CPM) or MICLF vs. ACDF for Unilateral Cervical Radiculopathy
Three studies demonstrated reduced costs for variants of CLF (i.e..., open CLF, PCF/CPM, MICLF) vs. ACDF when addressing lateral cervical pathology [
Rare Postoperative Instability and Adjacent Segment Disease After Minimally Invasive Cervical Laminoforaminotomy (MICLF) With/Without Microdiskectomy
Over an average of 44.4 postoperative months, Skovrlj et al. showed that 5 of 70 total patients undergoing MICLF required additional surgery at eight levels (i.e., five at the index surgical level and 3 for new adjacent level disease); summarized, this meant that only 1.1% of patients undergoing MICLF required fusions per year, with another 0.9% warranting surgery for ASD/year [
CONCLUSION
CLF and its’ minimally invasive, microendoscopic, and microdiskectomy variants offer greater safety, major pros with few cons, and decreased costs vs. ACDF for patients with lateral/foraminal cervical disc disease and/or spondylosis [
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy: Results of a new technique in 100 cases. J Neurosurg. 2001. 95: 51-7
2. Ament JD, Kaarnati T, Kulabya E, Kim KD, Jackson JP. Treatment of cervical radiculopathy: A review of the evolution and economics. Surg Neurol Int. 2018. 9: 35
3. Church EW, Halpern CH, Faught RW, Balmuri U, Attiah MA, Hayden S. Cervical laminoforaminotomy for radiculopathy: Symptomatic and functional outcomes in a large cohort with long-term follow-up. Surg Neurol Int. 2014. 5: S536-43
4. Epstein NE. A review of laminoforaminotomy for the management of lateral and foraminal cervical disc herniations or spurs. Surg Neurol. 2002. 57: 226-33 discussion 233-4
5. Epstein NE. Open laminoforaminotomy: A lost art?. Surg Neurol Int. 2015. 6: S600-7
6. Liu WJ, Hu L, Chou PH, Wang JW, Kan WS. Comparison of anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of cervical radiculopathy: A systematic review. Orthop Surg. 2016. 8: 425-31
7. Mansfield HE, Canar WJ, Gerard CS, O’Toole JE. Single-level anterior cervical discectomy and fusion versus minimally invasive posterior cervical foraminotomy for patients with cervical radiculopathy: a cost analysis. Neurosurg Focus. 2014. 37: E9
8. Sahai N, Changoor S, Dunn CJ, Sinha K, Hwang KS, Faloon M. Minimally invasive posterior cervical foraminotomy as an alternative to anterior cervical discectomy and fusion for unilateral cervical radiculopathy: A systematic review and meta-analysis. Spine (Phila Pa 1976). 2019. 44: 1731-9
9. Skovrlj B, Gologorsky Y, Haque R, Fessler RB, Qureshi SA. Complications, outcomes, and need for fusion after minimally invasive posterior cervical foraminotomy and microdiscectomy. Spine J. 2014. 14: 2405-11
10. Srikantha U, Hari A, Lokanath YK. Minimally invasive cervical laminoforaminotomy-Technique and outcomes. J Craniovertebr Junction Spine. 2021. 12: 361-7
11. Winder MJ, Thomas KC. Minimally invasive versus open approach for cervical laminoforaminotomy. Can J Neurol Sci. 2011. 38: 262-7
12. Yao R, Yan M, Liang Q, Wang H, Liu Z, Li F. Clinical efficacy and learning curve of posterior percutaneous endoscopic cervical laminoforaminotomy for patients with cervical spondylotic radiculopathy. Medicine (Baltimore). 2022. 101: e30401
13. Yilmaz H, Erturk AR, Karatus A, Atci IB, Yurt A. Posterior laminoforaminotomy in the treatment of lateral cervical herniated disc and foraminal stenosis. Turk J Med Sci. 2016. 46: 424-9
14. Yolas C, Ozdemir NG, Okay HO, Kanat A, Senol M, Atci IB. Cervical disc hernia operations through posterior laminoforaminotomy. J Craniovertebr Junction Spine. 2016. 7: 91-5
15. Yoo HJ, Park HJ, Seong YH, Roh SW. Comparison of surgical results between soft ruptured disc and foraminal stenosis patients in posterior cervical laminoforaminotomy. Korean J Neurotrauma. 2017. 13: 124-9
16. Zeitouni D, Pfortmiller D, Monk SH, Franklin D, Cowan D, Tenorio I. Microendoscopic posterior cervical laminoforaminotomy for C4 radiculopathy. World Neurosurg. 2023. 180: e729-32
17. Zou T, Wang PC, Chen H, Feng XM, Sun HH. Minimally invasive posterior cervical foraminotomy. Neurosurg Rev. 2022. 45: 3609-18