- Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA,
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA, 1122 Frankling Avenue Suite 106, Garden City, NY, USA.
Correspondence Address:
Nancy E. Epstein, M.D., F.A.C.S., Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief of Surgical Neurology International NY, USA, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA.
DOI:10.25259/SNI_1007_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Perspective: Efficacy and outcomes for different lumbar interspinous devices (ISD) vs. open surgery to treat lumbar spinal stenosis (LSS). 19-Jan-2024;15:17
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Perspective: Efficacy and outcomes for different lumbar interspinous devices (ISD) vs. open surgery to treat lumbar spinal stenosis (LSS). 19-Jan-2024;15:17. Available from: https://surgicalneurologyint.com/surgicalint-articles/12714/
Abstract
Background: Interspinous devices (ISD) constitute a minimally invasive (MI) alternative to open surgery (i.e., laminectomy/decompression with/without fusion (i.e., posterior lumbar interbody fusion (PLIF)/posterolateral instrumented fusion (PLF)) for treating lumbar spinal stenosis (LSS). Biomechanically, static and/or dynamic ISD “offload” pressure on the disc space, increase intervertebral foraminal/disc space heights, reverse/preserve lordosis, limit range of motion (ROM)/stabilize the surgical level, and reduce adjacent segment disease (ASD). Other benefits reported in the literature included; reduced operative time (OR Time), length of hospital stay (LOS), estimated blood loss (EBL), and improved outcomes (i.e., ODI (Oswestry Disability Index), VAS (Visual Analog Scale), and/or SF-36 (Short-Form 36)).
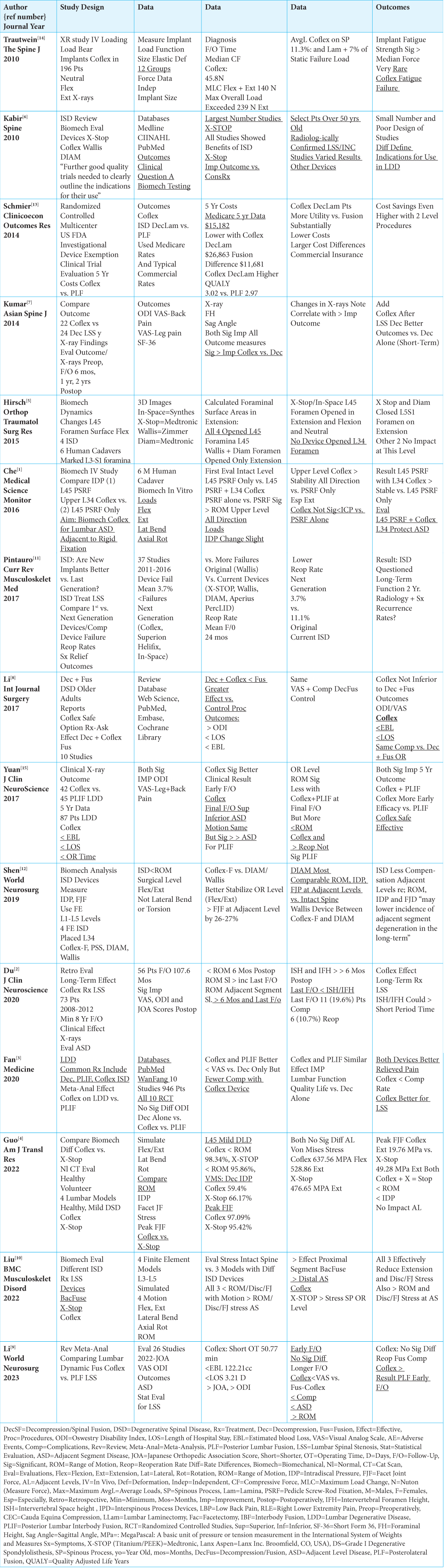
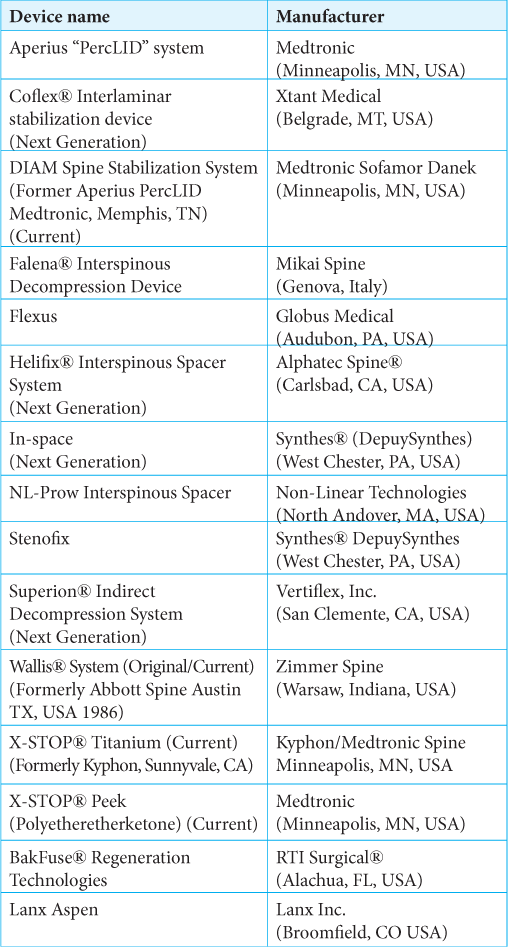
Methods: Various studies documented the relative efficacy and outcomes of original (i.e., Wallis), current (i.e., X-STOP, Wallis, DIAM, Aperius PercLID), and new generation (i.e., Coflex, Superion Helifix, In-Space) ISD used to treat LSS vs. open surgery.
Results: Although ISD overall resulted in comparable or improved outcomes vs. open surgery, the newer generation ISD provided the greatest reductions in critical cost-saving parameters (i.e., OR time, LOS, and lower reoperation rates of 3.7% for Coflex vs. 11.1% for original/current ISD) vs. original/current ISD and open surgery. Further, the 5-year postoperative study showed the average cost of new generation Coflex ISD/decompressions was $15,182, or $11,681 lower than the average $26,863 amount for PLF.
Conclusion: Patients undergoing new generation ISD for LSS exhibited comparable or better outcomes, but greater reductions in OR times, EBL, LOS, ROM, and ASD vs. those receiving original/current ISD or undergoing open surgery.
Keywords: Interspinous Devices (ISD), Static, Dynamic, X-Stop, Coflex, Lumbar Spinal Stenosis (LSS), Decompression, Posterior Lumbar Interbody Fusion (PLIF), Posterolateral Fusion (PLF), Open Surgery, Laminectomy, Complications, Outcomes, Adverse Events
INTRODUCTION
For treating lumbar spinal stenosis, we compared the efficacy and outcomes of 3 different categories of interspinous devices (ISD) vs. open surgery (i.e., laminectomy/decompression, posterior lumbar interbody fusion (PLIF), posterolateral fusion (PLF/other) [
Biomechanically, ISD Enhance Stability at the Index Surgical Level with Reduction of ASD
Five biomechanical studies using surgical fusion models documented the efficacy of different ISD devices in reducing ROM at the index and adjacent surgical levels [
Treatment of LSS: Efficacy and Outcomes for Different ISD Devices vs. Open Surgery
For LSS, Efficacy and Outcomes of Different ISD Devices vs. No Surgery vs. Open Surgery
Multiple ISD devices used to treat LSS improved clinical outcomes [
For LSS, Improved Efficacy and Outcomes of Decompressions/ Coflex ISD Alone or vs. Decompressions Alone
Two series focused on the improved efficacy and outcomes for patients undergoing decompressions/Coflex ISD placement for LSS alone or vs. decompressions only [
For LSS, Improved Efficacy and Outcomes of Decompressions/ Coflex ISD Alone or vs. Decompressions Alone
For LSS, four studies documented better or similar outcomes for decompressions/Coflex ISD procedures but greater reductions in perioperative factors vs. PLIF and vs. decompressions alone [
Greater Cost Savings for Decompression/Coflex ISD vs. Instrumented Posterolateral Lumbar Fusions (PLF) for Treating LSS
The study by Schmier et al. focused on the cost savings for decompression/Coflex ISD vs. instrumented posterolateral lumbar fusions (PLF) for treating LSS [
CONCLUSION
For treating LSS, different ISD devices (i.e., original, current, and new generation) resulted in comparable or better outcomes vs. open surgery (i.e., laminectomy/ decompressions, PLIF, instrumented PLF) or no surgery, but newer generation devices often demonstrated greater reductions in EBL, LOS, OR time, index-level ROM, ASD, reoperation rates, and increased cost savings.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Che W, Chen Q, Ma YQ, Jiang YQ, Yuan W, Zhou XG. Single-level rigid fixation combined with coflex: A biomechanical study. Med Sci Monit. 2016. 22: 1022-7
2. Du MR, Wei FL, Zhu KL, Song RM, Huan Y, Jia B. Coflex interspinous process dynamic stabilization for lumbar spinal stenosis: Long-term follow-up. J Clin Neurosci. 2020. 81: 462-8
3. Fan Y, Zhu L. Decompression alone versus fusion and Coflex in the treatment of lumbar degenerative disease: A network meta-analysis. Medicine (Baltimore). 2020. 99: e19457
4. Guo Z, Liu G, Wang L, Zhao Y, Zhao Y, Lu S. Biomechanical effect of Coflex and X-STOP spacers on the lumbar spine: A finite element analysis. Am J Transl Res. 2022. 14: 5155-63
5. Hirsch C, Breque C, Ragot S, Pascal-Mousselard H, Richer JP, Scepi M. Biomechanical study of dynamic changes in L4-L5 foramen surface area in flexion and extension after implantation of four interspinous process devices. Orthop Traumatol Surg Res. 2015. 101: 215-9
6. Kabir SM, Gupta SR, Casey AT. Lumbar interspinous spacers: A systematic review of clinical and biomechanical evidence. Spine (Phila Pa 1976). 2010. 35: E1499-506
7. Kumar N, Shah SM, Ng YH, Pannierselvam VK, Dasde S, Shen L. Role of coflex as an adjunct to decompression for symptomatic lumbar spinal stenosis. Asian Spine J. 2014. 8: 161-9
8. Li AM, Li X, Yang Z. Decompression and coflex interlaminar stabilisation compared with conventional surgical procedures for lumbar spinal stenosis: A systematic review and meta-analysis. Int J Surg. 2017. 40: 60-7
9. Li T, Yan J, Ren Q, Hu J, Wang F, Liu X. Efficacy and safety of lumbar dynamic stabilization device coflex for lumbar spinal stenosis: A systematic review and meta-analysis. World Neurosurg. 2023. 170: 7-20
10. Liu Z, Zhang S, Li J, Tang H. Biomechanical comparison of different interspinous process devices in the treatment of lumbar spinal stenosis: A finite element analysis. BMC Musculoskelet Disord. 2022. 23: 585
11. Pintauro M, Duffy A, Vahedi P, Rymarczuk G, Heller J. Interspinous implants: Are the new implants better than the last generation? A review. Curr Rev Musculoskelet Med. 2017. 10: 189-98
12. Shen H, Fogel GR, Zhu J, Liao Z, Liu W. Biomechanical analysis of different lumbar interspinous process devices: A finite element study. World Neurosurg. 2019. 127: e1112-9
13. Schmier JK, Halevi M, Maislin G, Ong K. Comparative cost effectiveness of Coflex® interlaminar stabilization versus instrumented posterolateral lumbar fusion for the treatment of lumbar spinal stenosis and spondylolisthesis. Clinicoecon Outcomes Res. 2014. 6: 125-31
14. Trautwein FT, Lowery GL, Wharton ND, Hipp JA, Chomiak RJ. Determination of the in vivo posterior loading environment of the Coflex interlaminar-interspinous implant. Spine J. 2010. 10: 244-51
15. Yuan W, Su QJ, Liu T, Yang JC, Kang N, Guan L. Evaluation of Coflex interspinous stabilization following decompression compared with decompression and posterior lumbar interbody fusion for the treatment of lumbar degenerative disease: A minimum 5-year follow-up study. J Clin Neurosci. 2017. 35: 24-9