- Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook and Editor-in-Chief Surgical Neurology International NY, USA, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA,
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA, 1122 Frankling Avenue Suite 106, Garden City, NY, USA.
Correspondence Address:
Nancy E Epstein, Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook and Editor-in-Chief Surgical Neurology International, and c/o Dr. Marc Agulnick 1122 Franklin Avenue Suite 106, Garden City, NY, United States.
DOI:10.25259/SNI_691_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E Epstein1, Marc A Agulnick2. Perspective; high frequency of intraoperative errors due to extreme, oblique, and lateral lumbar interbody fusions (XLIF, OLIF, LLIF): Are they “safe”?. 22-Sep-2023;14:346
How to cite this URL: Nancy E Epstein1, Marc A Agulnick2. Perspective; high frequency of intraoperative errors due to extreme, oblique, and lateral lumbar interbody fusions (XLIF, OLIF, LLIF): Are they “safe”?. 22-Sep-2023;14:346. Available from: https://surgicalneurologyint.com/surgicalint-articles/12563/
Abstract
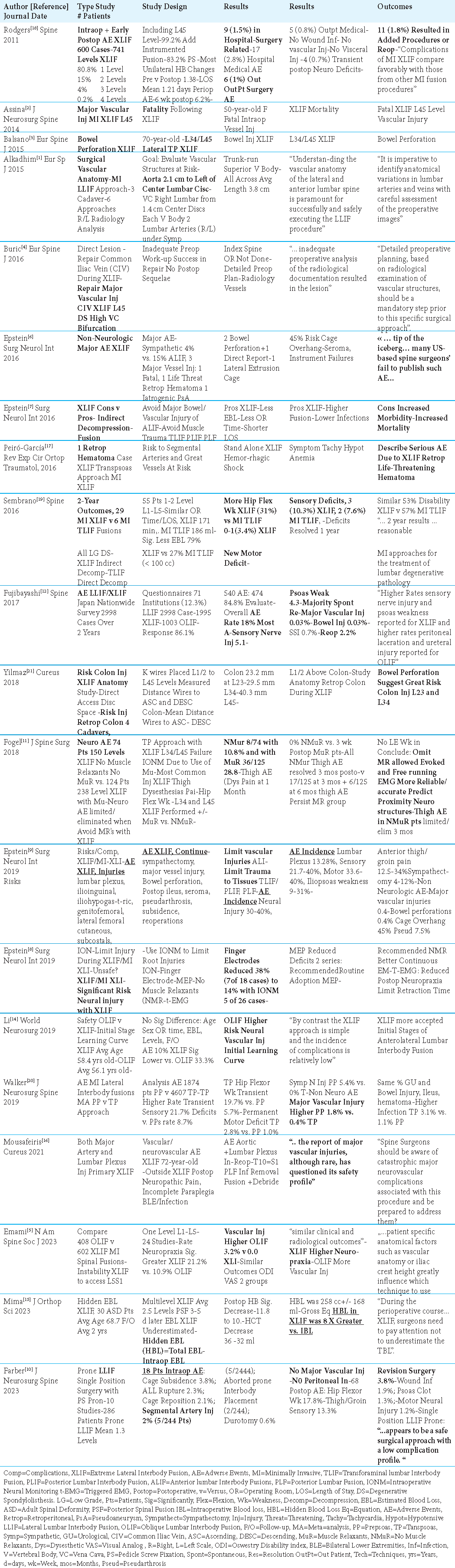
Background: Extreme Lateral Lumbar Interbody Fusions (XLIF), Oblique Lateral Interbody Fusion (OLIF,) and Lateral Lumbar Interbody Fusion (LLIF) were largely developed to provide indirect lumbar decompressions for spinal stenosis, deformity, and/or instability.
Methods: Here, we have reviewed and updated the incidence of intraoperative errors attributed to XLIF, OLIF, and LLIF. Specifically, we focused on how often these procedures caused new neurological deficits, major vessel, visceral, and other injuries, including those warranting secondary surgery.
Results: Performing XLIF, OLIF, and LLIF can lead to significant intraoperative surgical errors that include varying rates of; new neurological injuries (i.e. iliopsoas motor deficits (4.3-19.7-33.6-40%), proximal hip/upper thigh sensory loss/dysesthesias (5.1% to 21.7% to 40%)), life-threatneing vascular injuries (i.e., XLIF (0% - 0.4%-1.8%), OLIF (3.2%), and LLIF (2%) involving the aorta, iliac artery, inferior vena cava, iliac vein, and segmental arteries), and bowel/viscarl injuries (0.03%-0.4%) leading to reoperations (i.e., XLIF (1.8%) vs. LLIF (3.8%) vs. XLIF/LLIF/OLIF 2.2%)).
Conclusion: Varying reports documented that XLIF, OLIF and LLIF caused up to a 40% incidence of new sensory/motor deficits, up to a 3.2% incidence of major vascular insults, a 0.4% frequency of visceral/bowel perforations, and a 3.8% need for reoperations. These high frequencies of intraoperative surgical errors attributed to XLIF, OLIF, and LLIF should prompt reconsideration of whether these procedures are “safe.”
Keywords: Extreme Lateral Interbody Fusions (XLIF), Oblique Lateral Interbody Fusion (OLIF), Lateral Lumbar Interbody Fusions (LLLIF), Surgical Errors, Mistakes, Vascular, Bowel, Neural, Injuries, Intraoperative Mistakes, Lack of Safety/Efficacy
INTRODUCTION
Extreme Lateral Lumbar Interbody Fusions (XLIF), Oblique Lateral Interbody Fusion (OLIF,) and Lateral Lumbar Interbody Fusions (LLIF) provide indirect lumbar decompressions largely addressing spinal stenosis, instability, and/or deformity. However, they have previously been reported to cause varying frequencies of neural injuries (i.e., iliopsoas sensory/motor deficits up to 40%, proximal hip/upper thigh sensory loss up to 40%), up to a 3.2% frequency of major vascular injuries (i.e., aortic, iliac artery, inferior vena cava, iliac vein, segmental arteries), a 0.4% incidence of bowel/visceral injuries, and a 3.8% requirement for reoperations [
VARYING FREQUENCIES OF BOWEL INJURIES CAUSED BY XLIF
Cadaveric Study Showing Higher Risk of Colon Perforation for L23 and L34 XLIF
When Yilmaz et al. (2018) evaluated 4 cadavers, they documented that XLIF performed at the L23 and L34 levels put the retroperitoneal colon at greater risk for perforation; “The mean distance from the intervertebral disc space to the ascending or descending colon was 23.2 mm at the L23 level, 29.5 mm at the L34 level, and 40.3 mm at the l45 level” [
Frequencies of Bowel Injuries Caused by XLIF
Multiple studies showed the risks of bowel injuries occurring for XLIF ranged from 0% -0.03%-0.4%, while LLIF resulted in a 0% incidence of bowel perforations [
VARYING FREQUENCIES OF MAJOR VASCULAR INJURIES CAUSED BY XLIF, OLIF, AND LLIF
Varying frequencies of major vascular injuries/surgical errors have been reported during XLIF (0% up to 1.8%), OLIF (up to 3.2%), and LLIF (up to 2%) [
Need to Document Anterior Lumbar Vascular Anatomy Prior to XLIF, OLIF, and LLIF Surgery
In an effort to limit major vascular injuries occurring during XLIF, OLIF, and LLIF procedures, multliple authors recommended obtaining preoperative radiological studies to document the anatomy of the lumbar great vessels [
Four Case Studies of Major Vascular Injuries Due to XLIF
Four cases of great vessel injuries occurred during XLIF (i.e. 3 of which were at L45); 1 injury resulted in a mortality, 1 resulted in shock due to a retroperitoneal hematoma, and there were 2 common iliac vein injuries (in one case also involving a lumbar plexus injury) [
Risks of Major Vessel Injuries for XLIF (0% - 0.4%-1.8%), OLIF (3.2%), and LLIF (2%)
Three series showed varying frequencies of intraoperative major vessel injuries occurring during XLIF (0-0.4%-1.8%), OLIF (3.2%), and LLIF (2%) [
VARYING FREQUENCIES OF NEURAL INJURIES/ERRORS CAUSED BY XLIF, OLIF, LLIF
Development of Intraoperative Neural Monitoring Protocols to Limit XLIF Neural Errors
In 2019, Epstein cited varying frequencies of neural injuries largely attributed to XLIF; lumbar plexus injuries (13.28%), new sensory deficits (21.7%- 40%), new motor loss (33.6%-40%), and iliopsoas weakness (9%-31%) [
Eliminating Intraoperative Muscle Relaxants to Limit XLIF-Related Neural Injuries
Fogel et al. (2018) found that eliminating muscle relaxants during XLIF (NMuR) reduced the incidence of new motor neurological deficits to 10.8% (i.e. in 8 of 74 cases for L34/ L45 XLIF) vs. a higher 28.8% (i.e. in 36 of 125 cases for L34/ L45 XLIF) seen when using muscle relaxants (MuR).[
Incidences of Neural Injuries with Prepsoas (PP) vs. Transpsoas (TP) Minimially Invasive (MI) XLIF
When Walker et al. (2019) evaluated the incidence of neurological deficits caused by Prepsoas (PP: 1874 patients) v Transpsoas (TP: 4607 patients) MI XLIF approaches, they found TP procedures caused more transient sensory deficits (21.7%) vs. PP (8.7%) procedures. Further, MI XLIF also resulted in more motor deficits using Transpsoas v. Prepsoas procedures; specifically, TP caused greater hip flexor weakness (19.7%) vs. PP (5.7%), and TP caused more other permanent motor deficits (2.8%) vs. PP (1.0%) procedures.[
High Rates of Intraopereative Neurological Injuries/ Surgical Errors Attributed to XLIF, OLIF, and LLIF
High rates of intraoperative neurological injuries/surgical errors were caused by XLIF, OLIF, and LLIF; frequencies of new proximal motor/sensory neural deficits due to XLIF approached 40%, with a reported 10.9% incidence of neuropraxia attributed to OLIF; also multiple new neurological deficits occurred secondary to LLIF (i.e., hip flexor weakness (17.8%), thigh/groin sensory loss (13.3%), and motor neural injuries (1.2%)) [
FREQUENCY OF HIDDEN/INACCURATE ESTIMATED BLOOD (EBL) AND TOTAL BLOOD LOSS (TBL) REPORTED FOR XLIF
Mima et al. (2023) looked at 30 patients undergoing average 2.5 level XLIF, followed by lumbar pedicle/screw fusions performed between 3-5 days later; the pathology being addressed was adjacent segment disease (ASD) [
REOPERATION RATES FOR PATIENTS UNDERGOING XLIF (1.8%) VS. LLIF (3.8%)
The frequencies of reoperations attributed to surgical errors in the larger series, but also including data from the 5 case studies, were variably reported for XLIF (up to 1.8%), LLIF (up to 3.8%), and XLIF/LLIF/OLIF combined (up to 2.2%) [
ARE XLIF, LLIF AND OLIF “SAFE” DESPITE HIGH INTRAOPERATIVE SURGICAL ERROR RATES?
Despite high frequencies of surgery-related intraoperative errors, authors in several series concluded that XLIF/LLIF/ OLIF were “safe” [
MULTIPLE AUTHORS CONSIDER XLIF/OLIF NOT TO BE “SAFE” DUE TO HIGH ERROR RATES
Multipel authors were concerned about the “safety” of XLIF/ MI XLIF/OLIF procedures due to their high intraoperative surgical error rates.[
CONCLUSION
XLIF, OLIF, and LLIF collectively cause up to a 40% incidence of new sensory and motor deficits, up to a 3.2% incidence of major vascular insults, a 0.4% incidence of reported visceral/ bowel perforations, and a 3.8% need for repeat surgery. With such high frequencies of intraoperative surgical errors the spine surgical community should be now concluding that these XLIF, OLIF, and LLIF approaches are not “safe”.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alkadhim M, Zoccali C, Abbasifard S, Avila MJ, Patel AS, Sattarov K. The surgical vascular anatomy of the minimally invasive lateral lumbar interbody approach: A cadaveric and radiographic analysis. Eur Spine J. 2015. 24: 906-11
2. Assina R, Majmundar NJ, Herschman Y, Heary RF. First report of major vascular injury due to lateral transpsoas approach leading to fatality. J Neurosurg Spine. 2014. 21: 794-8
3. Balsano M, Carlucci S, Ose M, Boriani L. A case report of a rare complication of bowel perforation in extreme lateral interbody fusion. Eur Spine J. 2015. 24: 405-8
4. Buric J, Bombardieri D. Direct lesion and repair of a common iliac vein during XLIF approach. Eur Spine J. 2016. 25: 89-93
5. Emami A, Patel N, Coban D, Saela S, Sinha K, Faloon M. Comparing clinical and radiological outcomes between single-level OLIF and XLIF: A systematic review and meta-analysis. N Am Spine Soc J. 2023. 14: 100216
6. Epstein NE. Non-neurological major complications of extreme lateral and related lumbar interbody fusion techniques. Surg Neurol Int. 2016. 7: S656-9
7. Epstein NE. Extreme lateral lumbar interbody fusion: Do the cons outweigh the pros?. Surg Neurol Int. 2016. 7: S692-700
8. Epstein NE. Many intraoperative monitoring modalities have been developed to limit injury during extreme lateral interbody fusion (XLIF/MIS XLIF): Does that mean XLIF/MIS XLIF are unsafe?. Surg Neurol Int. 2019. 10: 233
9. Epstein NE. Review of risks and complications of extreme lateral interbody fusion (XLIF). Surg Neurol Int. 2019. 10: 237
10. Farber SH, Valenzuela Cecchi B, O’Neill LK, Chapple KM, Zhou JJ, Alan N. Complications associated with single-position prone lateral lumbar interbody fusion: A systematic review and pooled analysis. J Neurosurg Spine 2023;. 39: 380-6
11. Fogel GR, Rosen L, Koltsov JC, Cheng I. Neurologic adverse event avoidance in lateral lumbar interbody fusion: Technical considerations using muscle relaxants. J Spine Surg. 2018. 4: 247-53
12. Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, Nagashima H. Complications associated with lateral interbody fusion: Nationwide survey of 2998 Cases during the first 2 years of its use in Japan. Spine (Phila Pa 1976). 2017. 42: 1478-84
13. Kang YN, Ho YW, Chu W, Chou WS, Cheng SH. Effects and safety of lumbar fusion techniques in lumbar spondylolisthesis: A network meta-analysis of randomized controlled trials. Global Spine J. 2022. 12: 493-502
14. Li J, Wang X, Sun Y, Zhang F, Gao Y, Li Z. Safety analysis of two anterior lateral lumbar interbody fusions at the initial stage of learning curve. World Neurosurg. 2019. 127: e901-9
15. Mima Y, Yagi M, Suzuki S, Tsuji O, Nagoshi N, Okada E. Hidden blood loss in extreme lateral interbody fusion for adult spinal deformity. J Orthop Sci 2023;. 28: 509-14
16. Mousafeiris VK, Tsekouras V, Korovessis P. Simultaneous combined major arterial and lumbar plexus injury during primary extra lateral interbody fusion: Case report and review of the literature. Cureus. 2021. 13: e13701
17. Peiró-García A, Domínguez-Esteban I, Alía-Benítez J. Retroperitoneal hematoma after using the extreme lateral interbody fusion (XLIF) approach: Presentation of a case and a review of the literature. Rev Esp Cir Ortop Traumatol. 2016. 60: 330-4
18. Rodgers WB, Gerber EJ, Patterson J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: An analysis of 600 cases. Spine (Phila Pa 1976). 2011. 36: 26-32
19. Sembrano JN, Tohmeh A, Isaacs R. Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: Part I: Clinical findings. Spine (Phila Pa 1976). 2016. 41: S123-32
20. Walker CT, Farber SH, Cole TS, Xu DS, Godzik J, Whiting AC. Complications for minimally invasive lateral interbody arthrodesis: A systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J Neurosurg Spine. 2019. 30: 1-15
21. Yilmaz E, Iwanaga J, Moisi M, Blecher R, Abdul-Jabbar A, Tawfik T. Risks of colon injuries in extreme lateral approaches to the lumbar spine: An anatomical study. Cureus. 2018. 10: e2122