- Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook and Editor-in-Chief Surgical Neurology International NY, USA, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA,
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA, 1122 Frankling Avenue Suite 106, Garden City, NY, USA.
Correspondence Address:
Nancy E. Epstein, M.D., F.A.C.S., Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief of Surgical Neurology International NY, USA, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA.
DOI:10.25259/SNI_95_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Perspective: Operate on lumbar synovial cysts and avoid ineffective percutaneous techniques. 01-Mar-2024;15:65
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Perspective: Operate on lumbar synovial cysts and avoid ineffective percutaneous techniques. 01-Mar-2024;15:65. Available from: https://surgicalneurologyint.com/surgicalint-articles/12779/
Abstract
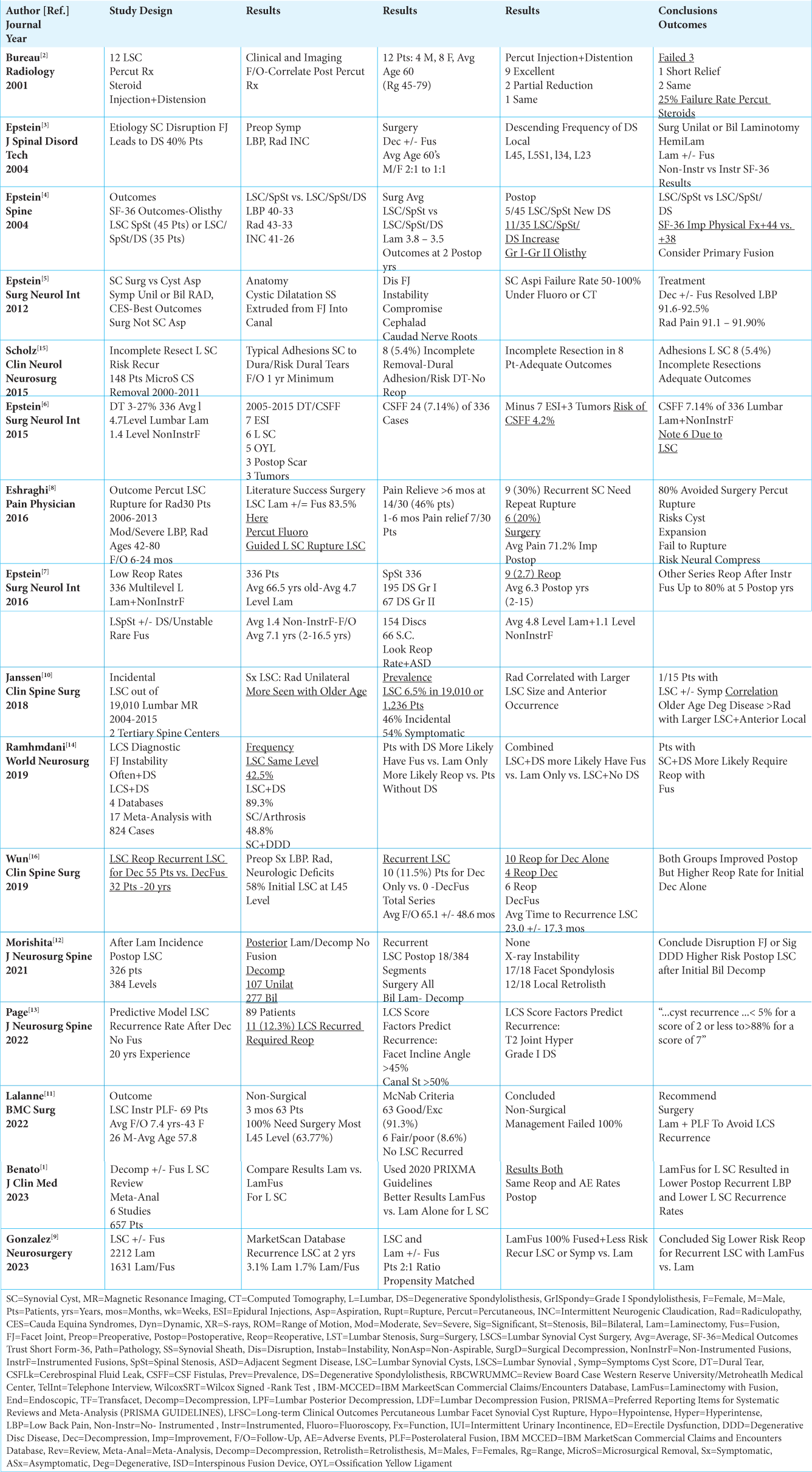
Background: Lumbar synovial cysts (LSC), best diagnosed on MR studies, may cause symptoms/signs ranging from unilateral radiculopathy to cauda equina compressive syndromes. Attempts at percutaneous treatment of LSC typically fail. Rather, greater safety/efficacy is associated with direct surgical resection with/without fusion.
Methods: Treatment of LSC with percutaneous techniques, including cyst aspiration/perforation, injection (i.e., with/without steroids, saline/other), dilatation, and/or disruption/bursting, classically fail. This is because LSCs’ tough, thickened, and adherent fibrous capsules cause extensive thecal sac/nerve root compression, and contain minimal central “fluid” (i.e., “crank-case” and non-aspirable). Multiple percutaneous attempts at decompression, therefore, typically cause several needle puncture sites risking dural tears (DT)/cerebrospinal fluid (CSF) leaks, direct root injuries, failure to decompress the thecal sac/nerve roots, infections, hematomas, and over the longer-term, adhesive arachnoiditis.
Results: Alternatively, many studies document the success of direct or even partial resection of LSC (i.e., partial removal with marked cyst/dural adhesions with shrinking down the remnant of capsular tissue). Surgical decompressions of LSC, ranging from focal laminotomies to laminectomies, may or may not warrant additional fusions.
Conclusions: Symptomatic LSC are best managed with direct or even partial operative resection/decompression with/without fusion. The use of varying percutaneous techniques classically fails, and increases multiple perioperative risks.
Keywords: Lumbar, Synovial Cysts: Operative Management, Avoid Cyst Aspiration, Failure Percutaneous Treatment, Adverse Events, Cyst Perforation, Cyst Disruption, Bursting, Lumbar Decompression, Fusion
INTRODUCTION
Lumbar synovial cysts (LSC), best diagnosed on MR studies, may cause symptoms ranging from unilateral radiculopathy to cauda equina syndromes/compression [
6.5% Frequency of Symptomatic/Asymptomatic Lumbar Synovial Cysts
In 2018, Janssen et al. found that in 19,010 lumbar MR scans (2004-2015 obtained at 2 tertiary care spine centers), lumbar synovial cysts (LSC) occurred in 6.5% or 1236 patients; 54% were symptomatic, while 46% were asymptomatic [
Etiology and Level of Lumbar Synovial Cysts (LSC)
The etiology of lumbar synovial cysts (LSC) occurring in patients in their sixties who developed radicular deficits were ascribed by Epstein (2004) and others to disruption of the facet capsule [
Failure of Non-Surgical Management of LSC
Lalanne et al. (2022) observed that 100% of 69 patients with LSC failed to improve following 3 months of non-surgical management; all 69 underwent decompressions/instrumented posterolateral lumbar fusions that resulted in no LSC recurrence [
SF-36 Postoperative Outcomes for Patients with Lumbar Synovial Cysts, Stenosis with/without DS Treated with Decompressions Alone
Utilizing the Short-Form 36 (SF-36) patient-based outcome measure, Epstein (2004) compared postoperative results for patients undergoing decompressions for resection of LSC/Stenosis (45 patients) vs. 35 with LSC/Stenosis/DS [
High Lumbar Synovial Cyst Occurrence Rates Following Decompressions Alone
Two studies highlighted 6.7% to 12.3% rates of postoperative LSC occurrences in patients undergoing bilateral lumbar decompressions [
LSC/Lumbar Stenosis Treated with Primary Decompressions/Fusions Reduced LSC Recurrence Rates vs. Decompressions Alone
Five studies showed that patients with LSC/Stenosis undergoing primary decompressions/fusions resulted in lower LSC recurrence rates vs. for those having decompressions alone [
Low Failure Rates for Incomplete Surgical Resection of Lumbar Synovial Cysts
Scholz et al. (2015) documented that 8 (5.4%) of 148 patients with lumbar stenosis and LSC underwent incomplete microsurgical cyst resections [
Stenosis with/without DS Treated with Lumbar Decompressions/Non-Instrumented Fusions Result In Few Dural Fistulas Attributed to LSC
In 2015, Epstein found an overall 7.14% frequency (i.e. 24 patients) of dural tears occurring in 336 patients undergoing average 4.7 level lumbar laminectomies/1.4 level non-instrumented fusions for stenosis with/without DS [
High Failure Rates for Multiple Percutaneous Procedures Addressing LSC
Three studies summarized the multiple failures for various attempts at percutaneous treatment of LSC [
CONCLUSION
Symptomatic LSC are best managed with operative decompression/fusion. Notably, the various percutaneous cyst aspiration, distension, dilatation/other techniques typically fail, unnecessarily exposing patients to added perioperative/postoperative adverse events.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Benato A, Menna G, Rapisarda A, Polli FM, D’Ercole M, Izzo A. Decompression with or without fusion for lumbar synovial cysts-a systematic review and meta-analysis. J Clin Med. 2023. 12: 2664
2. Bureau NJ, Kaplan PA, Dussault RG. Lumbar facet joint synovial cyst: Percutaneous treatment with steroid injections and distention--clinical and imaging follow-up in 12 patients. Radiology. 2001. 221: 179-85
3. Epstein NE. Lumbar synovial cysts: A review of diagnosis, surgical management, and outcome assessment. J Spinal Disord Tech. 2004. 17: 321-5
4. Epstein NE. Lumbar laminectomy for the resection of synovial cysts and coexisting lumbar spinal stenosis or degenerative spondylolisthesis: An outcome study. Spine (Phila Pa 1976). 2004. 29: 1049-55
5. Epstein NE. The diagnosis and management of synovial cysts: Efficacy of surgery versus cyst aspiration. Surg Neurol Int. 2012. 3: S157-66
6. Epstein NE. Incidence and management of cerebrospinal fluid fistulas in 336 multilevel laminectomies with non-instrumented fusions. Surg Neurol Int. 2015. 8: S463-8
7. Epstein NE. Low reoperation rate following 336 multilevel lumbar laminectomies with non-instrumented fusions. Surg Neurol Int. 2016. 7: S331-6
8. Eshraghi Y, Desai V, Cajigal CC, Tabbaa K. Outcome of percutaneous lumbar synovial cyst rupture in patients with lumbar radiculopathy. Pain Physician. 2016. 19: E1019-25
9. Gonzalez GA, Corso K, Kothari P, Franco D, Porto G, Miao J. Lumbar synovial cysts-should you fuse or not?. Neurosurgery. 2023. 92: 1013-20
10. Janssen SJ, Ogink PT, Schwab JH. The prevalence of incidental and symptomatic lumbar synovial facet cysts. Clin Spine Surg. 2018. 31: E296-301
11. Lalanne LB, Carmona RL, Totera JI, Lemos A, Wilson JT, Montoya AM. Surgically managed symptomatic intraspinal lumbar facet synovial cyst outcome of surgical treatment with resection and instrumented posterolateral fusion, a case series. BMC Surg. 2022. 22: 277
12. Morishita Y, Taniguchi R, Kawano O, Maeda T. Synovial facet joint cysts after lumbar posterior decompression surgery. J Neurosurg Spine. 2021. 35: 704-9
13. Page PS, Greeneway GP, Ammanuel SG, Resnick DK. Creation and validation of a predictive model for lumbar synovial cyst recurrence following decompression without fusion. J Neurosurg Spine. 2022. 37: 851-4
14. Ramhmdani S, Ishida W, Perdomo-Pantoja A, Witham TF, Lo SF, Bydon A. Synovial cyst as a marker for lumbar instability: A systematic review and meta-analysis. World Neurosurg. 2019. 122: e1059-68
15. Scholz C, Hubbe U, Kogias E, Klinger JH. Incomplete resection of lumbar synovial cysts-evaluating the risk of recurrence. Clin Neurol Neurosurg. 2015. 136: 29-32
16. Wun K, Hashmi SZ, Maslak J, Schneider AD, Katchko KM, Singh G. The variability of lumbar facet joint synovial cyst recurrence requiring revision surgery after decompression-only and decompression/fusion. Clin Spine Surg. 2019. 32: E457-61