- Department of Neurosurgery, Neuroscience Research Center, Faculty of Medicine, Lebanese University, Beirut, Lebanon
- American University of Technology, Faculty of Business Administration, Byblos, Lebanon
- Department of Neurological Surgery, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
Correspondence Address:
Youssef Fares
American University of Technology, Faculty of Business Administration, Byblos, Lebanon
DOI:10.4103/sni.sni_94_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Youssef Fares, Jawad Fares, Moustafa M. Kurdi, Mohamad A. Bou Haidar. Physician leadership and hospital ranking: Expanding the role of neurosurgeons. 03-Oct-2018;9:199
How to cite this URL: Youssef Fares, Jawad Fares, Moustafa M. Kurdi, Mohamad A. Bou Haidar. Physician leadership and hospital ranking: Expanding the role of neurosurgeons. 03-Oct-2018;9:199. Available from: http://surgicalneurologyint.com/surgicalint-articles/9031/
Abstract
Background:Empirical studies that explore whether hospitals with physician leadership perform better than hospitals led by nonphysician managers are scarce. This study looks at the leaders currently being hired by hospitals in the Arab World and explores whether chief executive officers (CEOs) in hospitals ranked higher are typically physician leaders or nonphysician managers. Furthermore, we discuss whether physicians, especially neurosurgeons, are equipped to lead hospitals and healthcare institutions worldwide.
Methods:The “Ranking Web of World Hospitals” by Cybermetrics Lab, 2017, was used. A dataset on CEOs in the top 50 hospitals and the bottom 50 hospitals in the Arab World was constructed. Independent samples t-test and regression equations were conducted, and P values
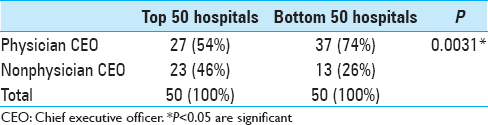
Results:A total of 283 hospitals were ranked. Among the top 50 hospitals, 54% of the CEOs were physicians, whereas the remaining were nonphysician managers. Among the bottom 50 hospitals, 74% of the CEOs were physicians, whereas 26% of the CEOs were nonphysicians. Interestingly, physician leadership was significantly associated with lower hospital ranking (bottom 50 hospitals) in the Arab World (P = 0.0031).
Conclusion:This article does not establish that nonphysician managers make more effective leaders when compared with physicians, but it starts an empirical course. For better evaluation of hospital leadership qualities, a new hospital ranking system must be created that focuses on patient satisfaction and perception of quality. Physician leaders, especially academic neurosurgeons, are an extraordinary leadership source, combining sound management with high medical standards. With the right academic training, neurosurgeons can play an increasingly significant role in addressing the challenges facing healthcare today.
Keywords: CEO, hospitals, leadership, managers, physicians, ranking
INTRODUCTION
The current healthcare environment in the Arab World has become extremely intricate, with increased demands to establish an equilibrium between quality and cost, and technology and humanity.[
For long, it has been hypothesized that hospitals perform better when they are led by physicians.[
The physician leaders’ clinical background gives them more credibility with the medical staff than nonphysician managers; physicians are more likely to respond well to physician leaders, especially on issues of medical management.[
In the Arab World, there are no empirical studies that assess the claim that hospitals with physician leadership perform better than when they are led by nonphysician managers. To establish a clear relationship between leadership and organizational outcomes is challenging because many of the conditions required for an unambiguously causal analysis cannot be met. Therefore, this study looks at the leaders currently being hired by hospitals in the Arab World and explores whether chief executive officers (CEOs) in hospitals ranked higher in the Arab World are typically physician leaders or nonphysician managers. Furthermore, the discussion expands with the aim of answering the following questions:
Are hospital ranking systems reliable? Who should run hospitals? Can physicians run hospitals? Can neurosurgeons lead hospitals? What makes neurosurgeons good hospital leaders?
MATERIALS AND METHODS
Study design
This empirical study looks at the CEOs in the top and bottom ranked hospitals in the Arab World – determining whether those hospitals ranked higher or lower in the league table are more likely to be headed by physician leaders or nonphysician managers. To do this, one particular ranking is used, namely, the “Ranking Web of World Hospitals” by Cybermetrics Lab, 2017.[
Data collection
The “Ranking Web of World Hospitals” is an initiative of the Cybermetrics Lab, a research group belonging to the Consejo Superior de Investigaciones Científicas (CSIC), the largest public research body in Spain.[
The unit for analysis is the institutional domain, so only hospitals with an independent web domain are considered. If an institution has more than one main domain, two or more entries are used with different addresses. Names and addresses were collected from both national and international sources, including “Hospitals Worldwide,” among others.[
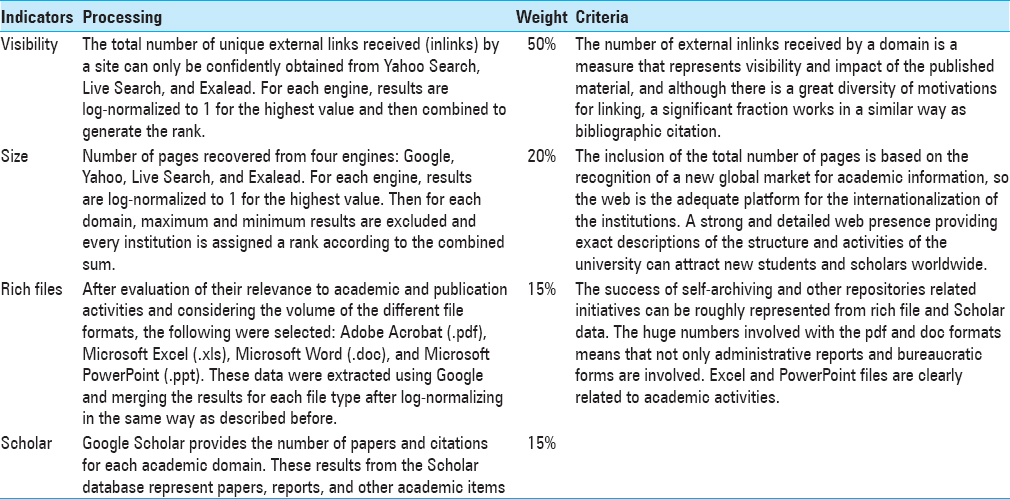
Hospital activity is multidimensional and this is reflected in its web presence. Therefore, the best way to build the ranking is by combining a group of indicators that measure these different aspects. Almind and Ingwersen proposed the first Web indicator, “Web Impact Factor” (WIF), based on link analysis that combines the number of external inlinks and the number of pages of the website, a ratio of 1:1 between visibility and size.[
Next, data were collected on each hospital CEO. To do this, we used hospitals’ websites and, on some occasions, personal contact with institutions (in the form of a request for the name of the CEO). Each CEO was classified into one of the two categories – physician leaders and leaders who are nonphysician managers. To qualify as a physician leader, by this study's criterion, a CEO must have been trained in medicine and obtained a Doctor of Medicine (MD) degree, or its equivalent (MBBS).
Data analysis
To establish whether the top 50 hospitals or bottom 50 hospitals in the rankings are more likely to be led by physicians or professional managers, we used an independent samples t-test and regression equations to compare percentages. P values <0.05 were considered statistically significant for all analyses. All statistical analyses were performed with GraphPad Prism.
RESULTS
A total of 283 hospitals were ranked in the Arab World. Hospitals ranking between 1 and 50 were considered the top 50 hospitals, and those ranking between 234 and 283 were considered the bottom 50 hospitals.
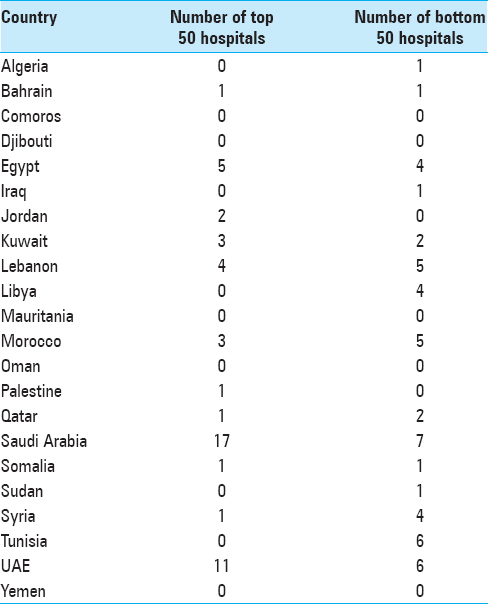
Saudi Arabia had the highest number of top 50 hospitals with 17 hospitals ranked, followed by the UAE with 11 top 50 hospitals. Saudi Arabia also had the highest number of bottom 50 hospitals with 7 hospitals ranked, followed by the UAE and Tunisia, with 6 hospitals each [
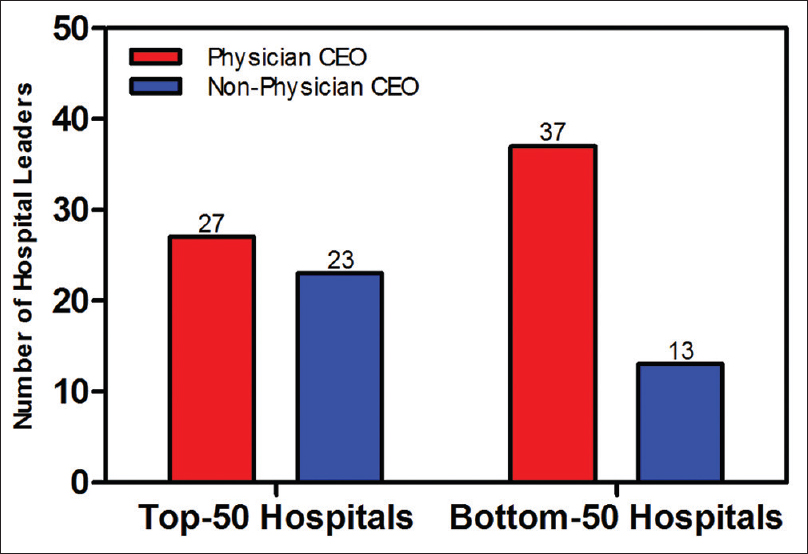
Among the top 50 hospitals in the Arab World, 54% of the CEOs were physicians, whereas 46% of the CEOs were nonphysician managers. Among the bottom 50 hospitals in the Arab World, 74% of the CEOs were physicians, whereas 26% of the CEOs were nonphysicians [
DISCUSSION
Our results are cross-sectional associations and use one particular hospital-quality ranking. This means that they have important limitations. Therefore, the findings do not prove that nonphysician managers make more effective leaders than physicians. Potentially, they may even reveal a form of the reverse – assortative matching – in that the bottom hospitals may be more likely to seek out physicians as leaders. Arguably, however, better hospitals will have a wider pool of CEO candidates to choose from, because of the extra status and wealth that they attract.[
Hospital ranking systems
The results of this study differ from what has been reported in the literature. Goodall found that US hospitals positioned higher in a widely used media ranking, “US News and World Report” (USNWR), are more likely to be led by medical doctors rather than managers.[
In our study, we use the “Ranking Web of World Hospitals” to assess hospital performance based on cybermetric indicators that are useful to evaluate science and technology metrics.[
The “Ranking Web of World Hospitals” used in our study includes all hospitals – regardless of size – in the Arab World that have a website domain. Many of the bottom 50 ranked hospitals were single-specialty centers, primary care centers, and polyclinics with few staff members and employees. However, the top 50 ranked hospitals were mostly academic medical centers that provide tertiary care in multiple disciplines and specialties. These centers often have hundreds of physicians, staff members, and employees. Therefore, it makes more sense that bigger hospitals will have a larger online presence, more web files, and more scholarly material associated with it. Consequently, academic medical centers will naturally rank higher when cybermetric and scientometric indicators are considered. However, with the variety of indicators used among different ranking systems, the question remains: what is the basis on which hospitals should be ranked?
If we advocate the “patientfirst” perspective that is the major driving force of physicians, then hospitals whose system satisfies the needs of patients more should be ranked higher. Academic medical centers and large teaching hospitals are not the benchmark by which other hospitals should be measured. A successful small hospital with good doctors and pleasant staff but no academic superstructure should be ranked adequately if its patients are satisfied with its services. The “patientfirst” ideal is a well-known principle in nearly every physician; however, in some places, administrations and politics come before the patient, as do other subjective factors. Moreover, the choice of the patient is often physician-related and not hospital-related. When a patient, a family member or a friend needs medical consultation, they look for the best physician available. If they go to the highly ranked hospitals, they do so with the hope that the best physicians are there as well; the hospital building or the administration per se are not the main concern of the patient. Nevertheless, it is unnecessary that the best ranked hospitals have the best physicians.
Current ranking metrics fail to address the patients’ needs or reflect measures of their satisfaction. Objectively determining the best hospital is hard and is almost impossible to quantitate.[
Who should run hospitals?
In the Arab World, politics, religion, and familial descent often play a role in dictating to whom the hospital leadership position is assigned. As the “provider of healthcare services” is an important and powerful position within the governance system, politics often overthrow academia and expertise.[
Hence, back to the question: “who should run hospitals?” We believe that physicians are the most equipped to run healthcare institutions as they can stir the hospital policies toward their longstanding principle: “patientsfirst.” Goodall's theory of “expert leadership” proposes that just as highly cited scholars make better presidents of research universities,[
Can physicians run hospitals?
Many would argue that the absence of managerial leadership competencies among the physicians who hold key positions in bottom-ranked hospitals is the reason why these hospitals ranked low. Indeed, physicians may be competent in the arenas of education, clinical care, and research; nonetheless, they may have little or no training in areas such as organizational behavior, management, finance, and marketing – a set of competencies increasingly more germane to their daily responsibilities.[
It is interesting that 7 of the top 10 hospitals ranked in 2018-2019 (USNWR) for neurology and neurosurgery are led by physicians.[
The issue is not with the physician's knowledge or capabilities but with the physician's goals. Some physicians might regard running a hospital as an administrative task, not a serious scholarly or intellectual endeavor. Physicians may also fear that assuming greater leadership responsibility would threaten their clinical commitment.[
It is important to note that the patient is the customer in the healthcare business. Bloom et al.[
Many believe that with the current health challenges facing the Arab World, professional managers and physicians are forced to collaborate; however, it has been documented in similar settings that the willingness and ability for managers and physicians to work together is actually eroding.[
Neurosurgeons as hospital leaders
Neurosurgery is an elite tertiary specialty that necessitates advanced technology and can only be practiced in hospitals. Furthermore, comprehensive care centers need neurosurgeons to treat the most critically ill patients, like those with acute cerebrovascular disease, brain tumors, or traumatic brain injury. Thus, both neurosurgeons and hospitals need each other. However, the question remains: have neurosurgeons, specifically, proven themselves to excel as hospital leaders?
Neurosurgeons are culturally known to be highly self-motivated, dedicated to excellence, and autonomous in their way of work. They are often the first to advance quality initiatives and can be leaders in helping organizations adapt to the changing healthcare environment.[
Neurosurgeons have a long history of excellence in healthcare leadership positions. In 1946, upon his return to Madrid, Spain, Dr. Sexto Obrador, pioneering Spanish neurosurgeon, started and developed several neurosurgical departments across the country. Most notably, Obrador was responsible for developing the emblematic Hospital de La Paz, which was famous for having one of the best neurosurgical services in the world. Dr. Alfonso Asenjo, pioneering Chilean neurosurgeon, founded the Institute of Neurosurgery and Brain Research of the University of Chile, serving as its Director. His institute was famous in the 1950s for being way ahead from the rest of the world. Another example is Dr. Manuel Velasco-Suarez, pioneering Mexican neurosurgeon, who constructed and organized the National Institute of Neurology and Neurosurgery of Mexico in 1964. The Institute has trained, in the past 50 years, hundreds of doctors from Mexico, Central and South America, Asia, and Europe. The center is among the largest and most comprehensive centers in the world. Other neurosurgeons have also proven their credentials in leadership positions at large and prominent hospitals worldwide.[
What makes neurosurgeons good hospital leaders?
We established that the leader should understand medicine well and must be aware of what physicians do on a daily basis. We also established that physicians, particularly neurosurgeons, can be good hospital leaders. Two questions follow: what makes a good hospital leader? And where can we find good hospital leaders?
A good hospital leader is decisive, fair, truthful, and a seeker of excellence. He or she does not compromise on the “patientfirst” principle or tolerate anything that stands in the way of what is best for the patients.
Where do we find those leaders? Successful leaders are found mostly as heads of highly stressful and demanding specialties. These personnel have proven themselves by building successful practices and leading teams of people to achieve great outcomes. Moreover, they are generally highly regarded by their peers and the society they live in. Physicians of less-demanding specialties may not be used to dealing with high-stress situations or taking decisive verdicts. This can lead to compromise in matters related to the “patientfirst” principle.
Much of this is personality-driven. Like the craft of neurosurgery, certain character traits and technical skills are symbiotic and essential for excellent leadership to face the rigors of uncertainty and change governing healthcare today. Successful neurosurgeons are strong decision-makers and fine executers by virtue of their training and practice. The systematic training involved in becoming a neurosurgeon develops inherent qualities and permits the acquisition of technical competencies that include strategic and tactical planning, persuasive communication, negotiation, financial decision-making, team-building, conflict resolution, and interviewing. These skills require training, akin to that of academic neurosurgery, and are necessary for the success and development of a 21st-century healthcare institution. In addition, neurosurgeon leaders, with their boastful skillset, are likely to set high standards for hiring. Subsequently, this leads to better outcomes and increased patient satisfaction and perception of quality.
CONCLUSION
It has been shown that hospitals positioned lower in a media ranking in the Arab World are more likely to be led by physicians rather than professional managers. However, given the difficulty of creating objective hospital performance measures, it is necessary to be cautious in analyzing empirical work.
A new hospital ranking system must be developed to focus on the “patient” in the healthcare environment. The metrics will typically answer the basic question of “what is the best place to go to when the patient is sick?” This system will also evaluate the leadership qualities of the persons who are leading such institutions and determine whether the leaders’ backgrounds are usually medical or nonmedical in nature.
Neurosurgeons are advised to obtain the academic training necessary for excellence in leadership so that the physician community may once again lead and direct the healthcare enterprise. Hospitals and academic medical centers need to be pulled out of the political and religious power struggles and debates that govern many countries in the Arab World, and patient satisfaction and quality of care must be prioritized.
Management education must become an integral part of all medical education, and medical schools and residency programs must designate leadership as a field of scholarly concentration so that interested and capable learners have opportunities to pursue further studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aguillo IF, Granadino B, Ortega JL, Prieto JA. Scientific research activity and communication measured with cybermetrics indicators. J Assoc Inf Sci Technol. 2006. 57: 1296-302
2. Aguillo IF, Granadino B, Ortega JL, Prieto JA. What the Internet says about Science: Universities can be ranked based on web indicators. Scientist. 2005. 19: 10-1
3. Almind TC, Ingwersen P. Informetric analyses on the world wide web: Methodological approaches to “webometrics.”. J Doc. 1997. 53: 404-26
4. Austin JM, D’Andrea G, Birkmeyer JD, Leape LL, Milstein A, Pronovost PJ. Safety in numbers: the development of Leapfrog's composite patient safety score for US hospitals. J Patient Saf. 2014. 10: 64-71
5. Ayoub F, Fares Y, Fares J. The psychological attitude of patients toward health practitioners in Lebanon. N Am J Med Sci. 2015. 7: 452-
6. Berenson RA, Ginsburg PB, May JH. Hospital-physicians relations: cooperation, competition, or separation?. Health Aff. 2007. 26: w31-43
7. Bloom N, Sadun R, Van Reenen J. Does management really work? How three essential practices can address even the most complex global problems. HBR. 2012. 90: 76-82
8. Castro PJ, Dorgan SJ, Richardson B. A healthier health care system for the United Kingdom. McKinsey Q. 2008. p. 1-5
9. Cochran J, Kaplan GS, Nesse RE. Physician leadership in changing times. Healthc (Amst). 2014. 2: 19-21
10. Comarow ALast accessed on 2018 Aug 19. Available from: https://health.usnews.com/health-care/best-hospitals/articles/faq-how-and-why-we-rank-and-rate-hospitals.
11. Cothey V, Aguillo I, Arroyo N. Operationalising “Websites”: Lexically, semantically or topologically. Cybermetrics. 2006. 10: 3-
12. Darzi A. A time for revolutions—The role of clinicians in health care reform. N Engl J Med. 2009. 361: e8-
13. Dwyer AJ. Medical managers in contemporary healthcare organisations: A consideration of the literature. Aust Health Rev. 2010. 34: 514-22
14. Dyrda LLast accessed on 2018 Jun 5. Available from: https://www.beckersspine.com/orthopedic-spine-industry-leaders/item/2809-8-spine-and-neurosurgeon-leaders-at-large-hospitals.
15. Falcone RE, Satiani B. Physician as hospital chief executive officer. Vasc Endovascular Surg. 2008. 42: 88-94
16. Fares MY, Fares J, Baydoun H, Fares Y. Sport and exercise medicine research activity in the Arab world: A 15-year bibliometric analysis. BMJ Open Sport Exerc Med. 2017. 3: e000292-
17. Fares Y, Fares J. Neurosurgery in Lebanon: History, development, and future challenges. World Neurosurg. 2017. 99: 524-32
18. Goodall AH, Kahn LM, Oswald AJ. Why do leaders matter? A study of expert knowledge in a superstar setting. J Econ Behav Organ. 2011. 77: 265-84
19. Goodall AH. A theory of expert leadership (TEL) in psychiatry. Australas Psychiatry. 2016. 24: 231-4
20. Goodall AH. Highly cited leaders and the performance of research universities. Res Policy. 2009. 38: 1079-92
21. Goodall AH. Physician-leaders and hospital performance: Is there an association?. Soc Sci Med. 2011. 73: 535-9
22. Goodall AH. Should top universities be led by top researchers and are they. A citations analysis?. J Doc. 2006. 62: 388-411
23. Goodall AH.editors. Socrates in the boardroom: Why research universities should be led by top scholars. Princeton University Press; 2009. p.
24. Gunderman R, Kanter SL. Perspective: Educating physicians to lead hospitals. Acad Med. 2009. 84: 1348-51
25. Halligan A. Aidan Halligan on why Darzi needs clinical leadership. HSJ. 2008. 7:
26. Horton R. The Darzi vision: Quality, engagement, and professionalism. Lancet. 2008. 372: 3-4
27. Imison C, Giordano RW. Doctors as leaders. BMJ. 2009. p. 338-
28. Kim DH, Duco B, Wolterman D, Stokes C, Brace R, Solomon RA. A Review and survey of neurosurgeon–hospital relationships: Evolution and options. Neurosurgery. 2017. 80: S10-8
29. Kretschmer H, Aguillo IF. New indicators for gender studies in Web networks. IPM. 2005. 41: 1481-94
30. Kretschmer H, Aguillo IF. Visibility of collaboration on the Web. Scientometrics. 2004. 61: 405-26
31. Last accessed on 2018 Jun 5. Available from: https://en.mehrnews.com/news/115715/World-s-largest-neurosurgical-hospital-to-be-launched-in-Tehran.
32. Ortega JL, Aguillo I, Prieto JA. Longitudinal study of content and elements in the scientific web environment. J Inf Sci. 2006. 32: 344-51
33. Pope DG. Reacting to rankings: Evidence from “America's Best Hospitals”. J Health Econ. 2009. 28: 1154-65
34. Last accessed on 2018 Mar 21. Available from: http://hospitals.webometrics.info/en/aw.
35. Schneider EC, Epstein AM. Use of public performance reports: A survey of patients undergoing cardiac surgery. JAMA. 1998. 279: 1638-42
36. Schwartz RW, Pogge C. Physician leadership: Essential skills in a changing environment. Am J Surg. 2000. 180: 187-92
37. Sehgal AR. The role of reputation in US News & World Report's rankings of the top 50 American hospitals. Ann Intern Med. 2010. 152: 521-5
38. Stoller JK, Goodall A, Baker A. Why the best hospitals are managed by doctors. HBR. 2016. p. 12-27
39. Stoller JK. Developing physician-leaders: A call to action. J Gen Intern Med. 2009. 24: 876-8
40. Last accessed on 2018 Jun 5. Available from: https://www.beckershospitalreview.com/hospital-management-administration/the-case-for-physician-ceos.html.
41. Last accessed on 2018 Aug 19. Available from: https://health.usnews.com/best-hospitals/rankings/neurology-and-neurosurgery.
42. Last accessed on 2018 Aug 19. Available from: https://www.usnews.com/info/blogs/press-room/articles/2018-08-14/us-news-announces-2018-19-best-hospitals.
43. Wouters P, Reddy C, Aguillo I. On the visibility of information on the Web: An exploratory experimental approach. Res Eval. 2006. 15: 107-15
44. Xu G, Paddock LE, O’Connor JP, Nash DB, Buehler ML, Bard M. Physician executives report high job satisfaction. Summary of findings from a survey of senior physician executives. Physician Exec. 2001. 27: 46-7






Abed Alkarim Mubarak
Posted November 22, 2018, 8:48 pm
Very good study and very interested,and the leader physician more effective than no physician ..