- Department of Neurosurgery, Saga University, Saga, Japan.
Correspondence Address:
Jun Masuoka, Department of Neurosurgery, Saga University, Saga, Japan.
DOI:10.25259/SNI_421_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jun Masuoka, Fumitaka Yoshioka, Kohei Inoue, Takashi Furukawa, Hiroshi Ito, Atsushi Ogata, Yukiko Nakahara, Tatsuya Abe. Pituitary adenoma presenting as isolated oculomotor nerve palsy. 01-Sep-2023;14:305
How to cite this URL: Jun Masuoka, Fumitaka Yoshioka, Kohei Inoue, Takashi Furukawa, Hiroshi Ito, Atsushi Ogata, Yukiko Nakahara, Tatsuya Abe. Pituitary adenoma presenting as isolated oculomotor nerve palsy. 01-Sep-2023;14:305. Available from: https://surgicalneurologyint.com/surgicalint-articles/12526/
Abstract
Background: Isolated oculomotor nerve palsy is a relatively uncommon symptom of pituitary adenoma that usually occurs in association with pituitary apoplexy or cavernous sinus (CS) invasion.
Case Description: We report two cases of relatively small pituitary adenomas with neither apoplexy nor CS invasion presenting as isolated oculomotor nerve palsy. Both patients presented with gradually worsening diplopia, without headache or visual field defects. Magnetic resonance imaging (MRI) showed a pituitary tumor with no evidence of intratumoral hemorrhage. Computed tomography revealed a lateroposterior extension of the tumor with the erosion of the posterior clinoid process. Constructive interference in steady-state MRI revealed compression of the oculomotor nerve by the tumor at the oculomotor triangle. The patients underwent endoscopic transsphenoidal surgery, and the intraoperative findings showed that the tumors did not invade the CS. The tumors were completely resected, and the oculomotor palsies resolved fully.
Conclusion: These cases illustrate the need to consider isolated oculomotor nerve palsy as an initial manifestation of a relatively small pituitary adenoma with neither apoplexy nor CS invasion. Based on the characteristic radiological findings, early surgical treatment is recommended to preserve oculomotor function.
Keywords: Constructive interference in steady-state (CISS), Oculomotor nerve palsy, Pituitary adenoma
INTRODUCTION
Visual field defects and endocrine dysfunction are the most common manifestations of pituitary adenoma. Oculomotor nerve palsy is less frequent and usually occurs in association with pituitary apoplexy or cavernous sinus (CS) invasion.[
CASE PRESENTATION
Case 1
A 65-year-old man presented with diplopia in the left gaze for the past 2 months. He did not experience headaches or vomiting. Ophthalmic testing revealed restricted supraduction and adduction of the right eye. Anisocoria, abnormal pupillary light reflex, or ptosis were not observed. Visual acuity and field measurements were within the normal range. A neurological diagnosis of an isolated right oculomotor nerve palsy was established. Magnetic resonance imaging (MRI) revealed a 19 mm homogeneously enhanced pituitary tumor that extended latero-posteriorly on the right side [
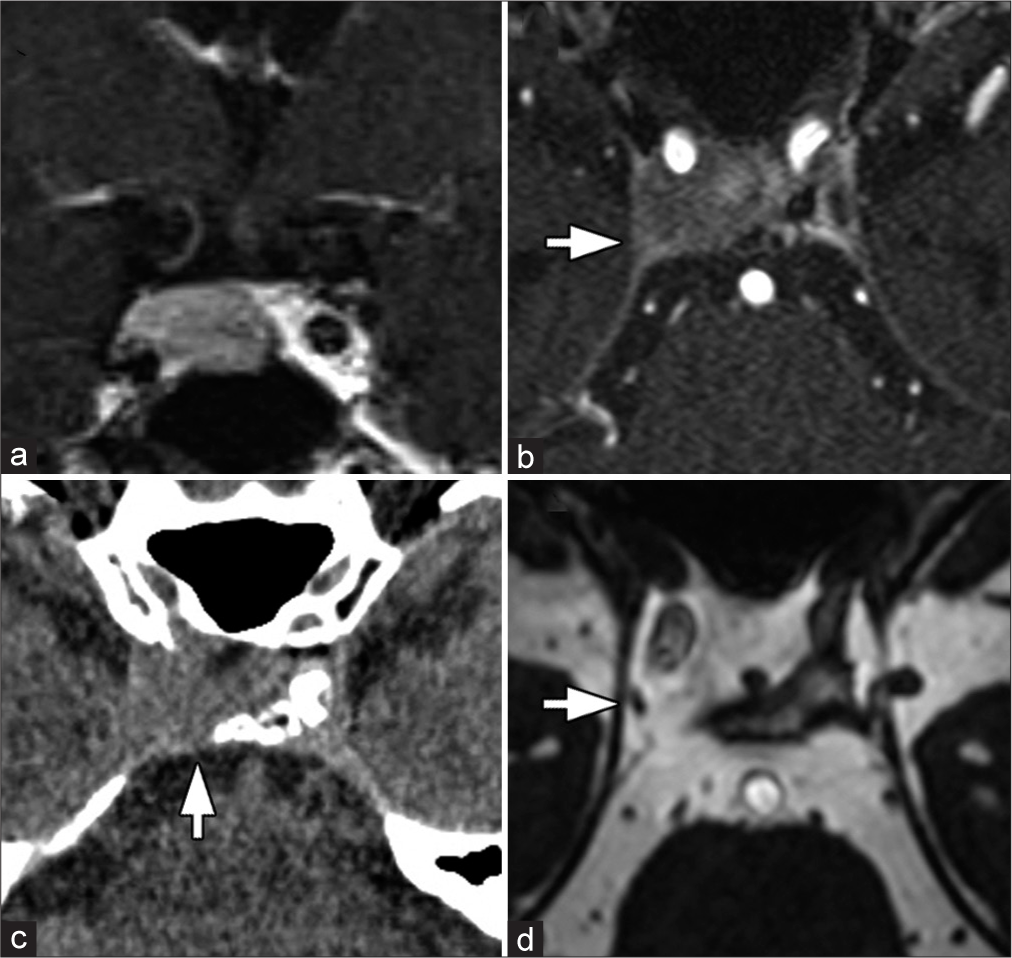
Figure 1:
(a) Coronal gadolinium-enhanced T1-weighted image (Gd-T1WI) on magnetic resonance (MR) imaging showing homogeneously enhancing pituitary tumor with no evidence of intratumoral hemorrhage. (b) Axial Gd-T1WI showing lateroposterior tumor extension to the right cavernous sinus (arrow). (c) Computed tomography scan showing erosion of the right posterior clinoid process (arrow). (d) Postoperative constructive interference in steady-state MR image showing the right oculomotor nerve at the oculomotor triangle (arrow).
Case 2
A 75-year-old man presented with diplopia and drooping of the left eyelid for 2 weeks. He did not experience headaches or vomiting. Examination of the patient revealed mild ptosis with limited supraduction, adduction, and infraduction of the left eye. Anisocoria or abnormal pupillary light reflexes were not observed. The neurological diagnosis was an isolated left oculomotor nerve palsy. MRI revealed an 18 mm homogeneously enhanced pituitary tumor that extended latero-posteriorly on the left side [
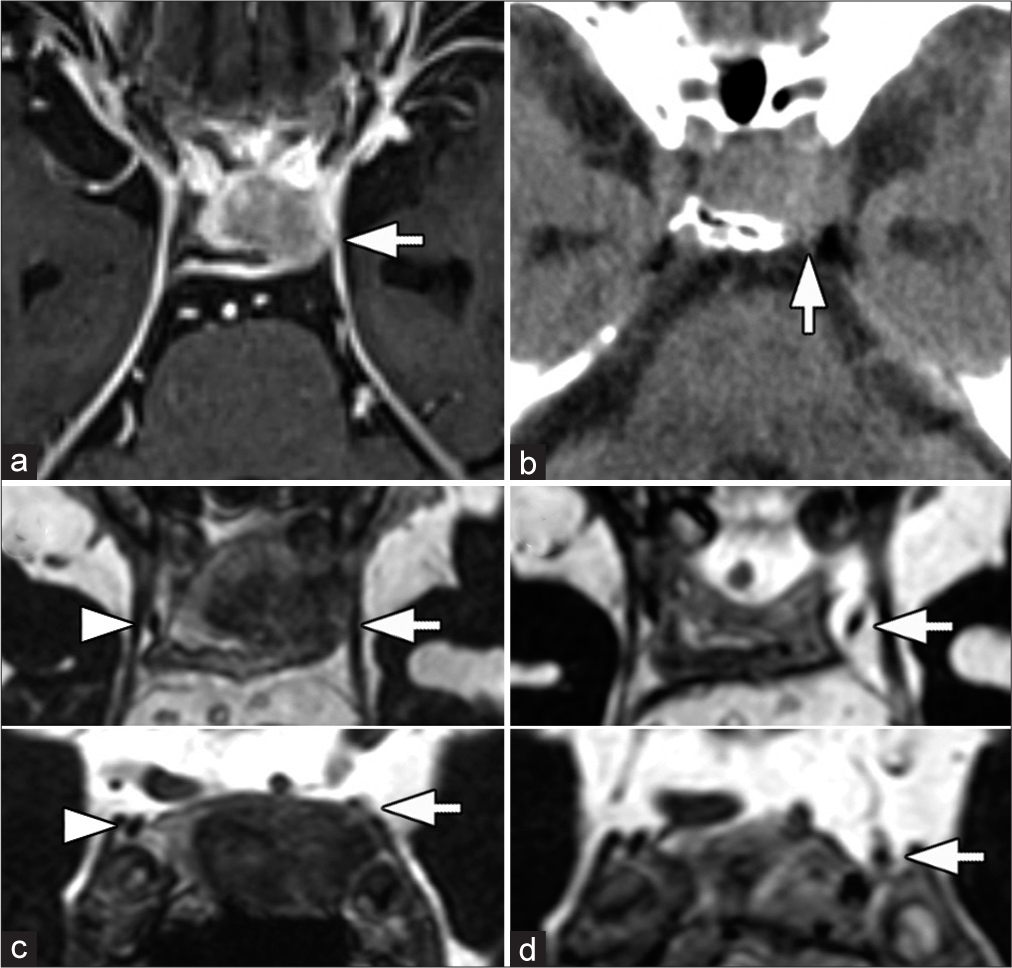
Figure 3:
(a) Axial gadolinium-enhanced T1-weighted magnetic resonance (MR) image showing homogenously enhancing pituitary tumor protruding latero-posteriorly to the left cavernous sinus (arrow) with no apparent findings of pituitary apoplexy. (b) Computed tomography scan showing erosion of the left posterior clinoid process (arrow). (c) Preoperative constructive interference in steady-state (CISS) MR images (axial and coronal views) showing compression of the left oculomotor nerve by the tumor (arrow). The right oculomotor nerve is visible (arrowhead). (d) Postoperative CISS MR images (axial and coronal views) showing the left oculomotor nerve at the oculomotor triangle (arrow).
Two months after the onset of symptoms, the patient underwent endoscopic transsphenoidal surgery, and the tumor was completely resected. Intraoperatively, there was no evidence of CS invasion by the tumor. The pathological diagnosis was a nonfunctioning pituitary adenoma with no evidence of hemorrhage or necrosis. Immediately after surgery, the patient’s oculomotor nerve function recovered completely. Postoperative CISS MRI confirmed the presence of the left oculomotor nerve at the oculomotor triangle [
DISCUSSION
Chuang et al.[
The oculomotor triangle at the entrance of the CS is considered the main site of isolated oculomotor nerve palsy in patients with pituitary adenomas with apoplexy.[
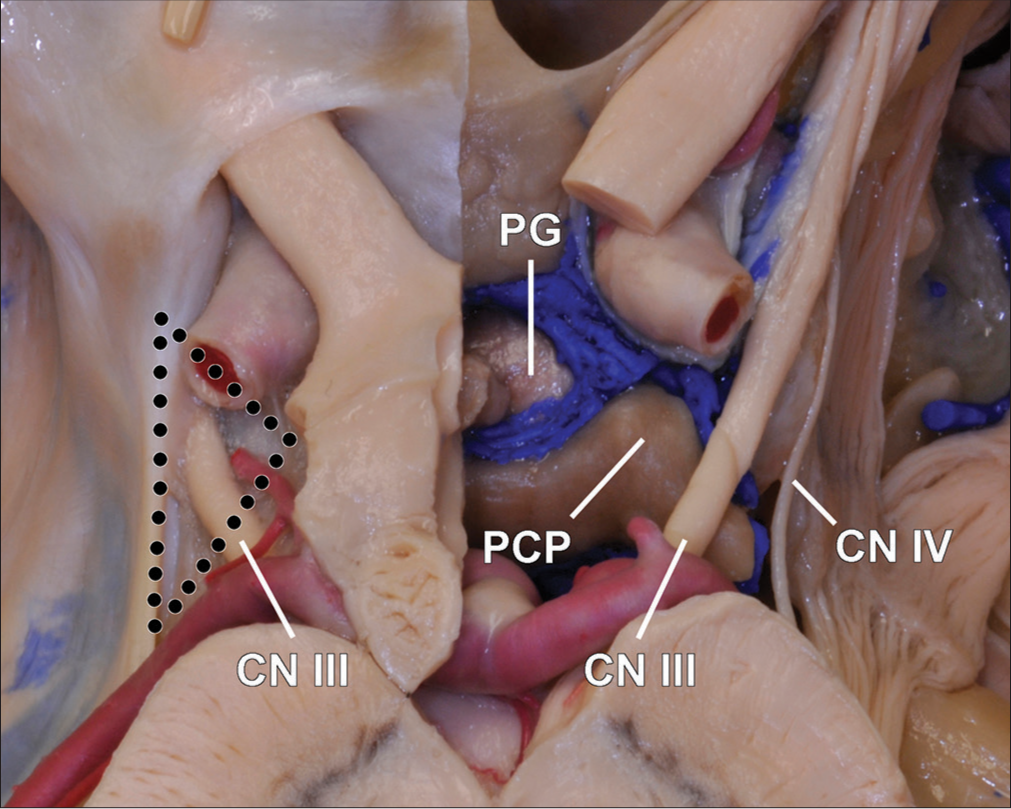
Figure 5:
Photograph of a cadaveric specimen showing the normal anatomy of the oculomotor nerves. The left oculomotor nerve enters the roof of the cavernous sinus through the oculomotor triangle (dotted line). The right cavernous sinus roof has been removed to expose the entire course of the oculomotor nerve. CN: Cranial nerve, PCP: Posterior clinoid process, PG: Pituitary gland.
The prognosis of patients with oculomotor nerve palsy mainly depends on: (1) the interval between the onset of palsy and operation and (2) the degree of preoperative deficit.[
Recently, the clinical importance of pituitary tumor extension into the oculomotor cistern has been advocated.[
CONCLUSION
These two cases illustrate the need to consider isolated oculomotor nerve palsy as the initial manifestation of a relatively small pituitary adenoma with neither apoplexy nor CS invasion. Based on the characteristic radiological findings in patients with lateroposterior extension of the tumor and compression of the oculomotor nerve at the oculomotor triangle, early surgical treatment is recommended to preserve good oculomotor function.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bruce BB, Biousse V, Newman NJ. Third nerve palsies. Semin Neurol. 2007. 27: 257-68
2. Chuang CC, Chen E, Huang YC, Tu PH, Chen YL, Pai PC. Surgical outcome of oculomotor nerve palsy in pituitary adenoma. J Clin Neurosci. 2011. 18: 1463-8
3. Hoang N, Tran DK, Herde R, Couldwell GC, Osborn AG, Couldwell WT. Pituitary macroadenomas with oculomotor cistern extension and tracking: Implications for surgical management. J Neurosurg. 2016. 125: 315-22
4. Kawase T, van Loveren H, Keller JT, Tew JM. Meningeal architecture of the cavernous sinus: Clinical and surgical implications. Neurosurgery. 1996. 39: 527-34
5. Kobayashi H, Kawabori M, Terasaka S, Murata J, Houkin K. A possible mechanism of isolated oculomotor nerve palsy by apoplexy of pituitary adenoma without cavernous sinus invasion: A report of two cases. Acta Neurochir (Wien). 2011. 153: 2453-6
6. Martins C, Yasuda A, Campero A, Rhoton AL. Microsurgical anatomy of the oculomotor cistern. Neurosurgery. 2006. 58: ONS-220-7 discussion ONS-227-8
7. Sasagawa Y, Aburano H, Ooiso K, Oishi M, Hayashi Y, Nakada M. Oculomotor nerve palsy in pituitary apoplexy associated with pituitary adenoma: A radiological analysis with fast imaging employing with steady-state acquisition. Acta Neurochir (Wien). 2021. 163: 383-9
8. Taniguchi M, Nakai T, Kimura H, Fujita Y, Uozumi Y, Kohta M. Endoscopic endonasal surgery for pituitary adenomas extending to the oculomotor cistern. Head Neck. 2017. 40: 536-43