- Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, Cheonan, Chungcheongnam-do-Korea, South Korea.
DOI:10.25259/SNI_82_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jae-Min Ahn, Hyuk-Jin Oh, Jae-Sang Oh, Seok-Mann Yoon. Pituitary apoplexy causing acute ischemic stroke: Which treatment should be given priority. 16-May-2020;11:113
How to cite this URL: Jae-Min Ahn, Hyuk-Jin Oh, Jae-Sang Oh, Seok-Mann Yoon. Pituitary apoplexy causing acute ischemic stroke: Which treatment should be given priority. 16-May-2020;11:113. Available from: https://surgicalneurologyint.com/surgicalint-articles/10029/
Abstract
Background: Pituitary apoplexy is syndrome of sudden onset of headache, visual loss, pituitary dysfunction, and altered consciousness. Pituitary apoplexy followed by acute cerebral ischemia is extremely rare. Here, we introduced the case of successful surgical resection of pituitary adenoma which induced acute cerebral ischemia.
Case Description: A 78-year-old man with a known pituitary macroadenoma presented with decreased consciousness and left hemiparesis. Magnetic resonance image (MRI) and computed tomography (CT) showed large pituitary macroadenoma with hemorrhage and diffusion-perfusion mismatch of right internal carotid artery (ICA) territory. Conventional angiography was done and severe stenosis of bilateral ICA and prominent flow delay of left ICA were noted at paraclinoid segment. Microscopic tumor mass removal with transsphenoidal approach was performed. Final pathological diagnosis was pituitary adenoma with apoplexy. Immediately after surgery, his symptoms were disappeared. Follow-up image studies revealed much improved perfusion in right ICA territory and patency of bilateral ICAs.
Conclusion: Direct compression of ICA is rare complication of pituitary apoplexy, which caused cerebral ischemia. Conventional angiography should be necessary for accurate diagnosis and prompt surgical decompression should be the treatment of choice.
Keywords: Cerebral angiography, Cerebral infarction, Pituitary apoplexy
INTRODUCTION
Pituitary apoplexy is a clinical syndrome of sudden onset headache, visual disturbance, ophthalmoplegia, and even fetal symptoms such as altered consciousness and pituitary dysfunction, which can result from hemorrhage or infarction of the pituitary adenoma. Although there have been several reports, acute ischemic stroke associated with pituitary apoplexy is very rare.[
CASE DESCRIPTION
A 78 year-old man visited the emergency room due to decreased consciousness on the day of visit. He was in a stupor consciousness with left hemiparesis. His right pupil was dilated to 8 mm, and no light reflex was observed. He had no remarkable medical histories except hypertension.
One week before admission, he visited our outpatient clinic with a history of headache and visual disturbance. Brain computed tomography (CT) and visual field test at that time revealed bitemporal hemianopsia due to direct compression by pituitary macroadenoma, and he was scheduled for tumor mass removal through transsphenoidal approach.
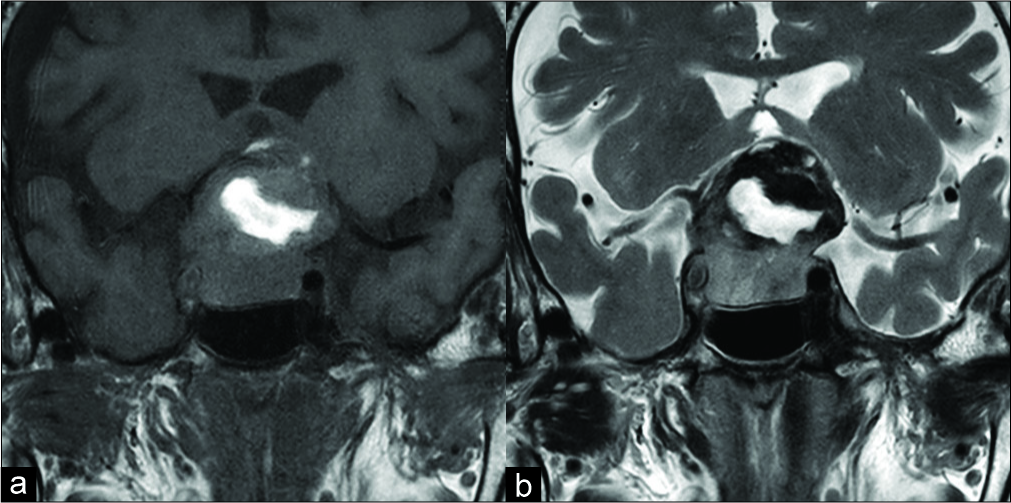
Brain magnetic resonance imaging (MRI) on admission showed about 38 mm × 28 mm sized large pituitary macroadenoma with hemorrhagic component inside the tumor [
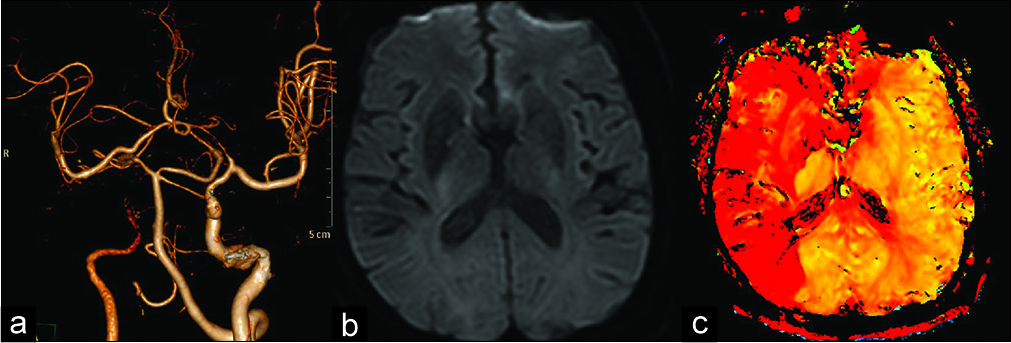
Figure 2:
Preoperative computed tomographic angiography and diffusion-perfusion images. (a) Disappeared right internal carotid artery flow near clinoid segment. (b) No definite acute infarction in the diffusion weighted magnetic resonance study. (c) Severe perfusion delays were identified on whole right internal carotid artery territory.
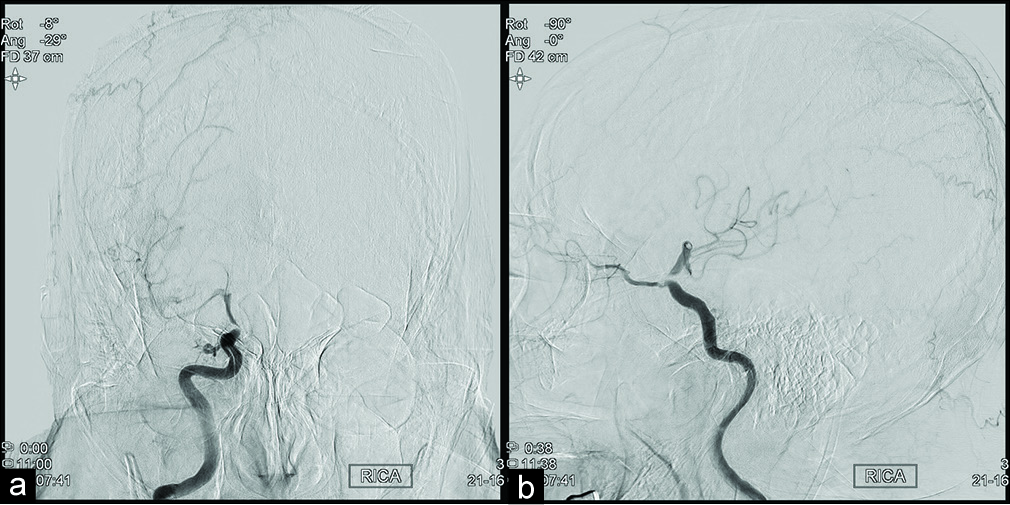
Emergency trans-femoral cerebral angiography was performed because very severe diffusion-perfusion mismatches and right internal carotid artery (ICA) occlusion were confirmed with associated acute ischemic symptoms. Right ICA angiogram showed severe stenosis in the paraclinoid segment with the minimal flow to the MCA. Left ICA angiogram also showed narrowed left ICA at the same segment [
Emergency mechanical thrombectomy with balloon angioplasty was done. Microcatheter was gently passed through the right ICA stenotic lesion and stent was deployed and retrieved. However, there was no thrombus in the retrieved stent or aspirated blood, and follow-up angiography showed only temporary improving of ICA flow. Balloon angioplasty was performed in consideration of direct compression by large parasellar mass, or in situ thrombosis due to right ICA stenosis. However, even after balloon angioplasty, only temporary improving of blood flow was noted. The procedure was terminated because the external direct compression lesion was considered the main cause rather than the intravascular lesion.
Microscopic transsphenoidal approach tumor removal was done. When the dural base was opened, mass was bulging out with a large amount of hematoma. Intra-capsular removal was performed on a grey colored suckable mass, and subtotal mass removal was achieved. After removal of tumor, Doppler ultrasonography was used for confirmed that the bilateral ICA flow was intact. During the operation, blood pressure was strictly maintained over mean arterial pressure 80 mmHg to prevent hypoperfusion. Final diagnosis was pituitary adenoma with apoplexy. The patient’s consciousness was completely restored immediately after surgery, and the left hemiparesis and pupil dilatation also improved.
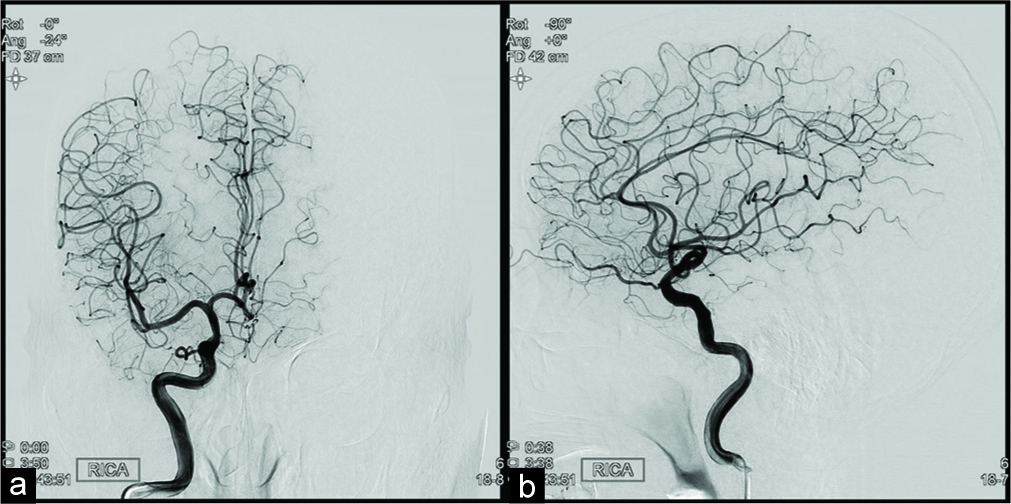
Follow-up image study showed full recovery of right ICA territory perfusion with no significant infarction except for some scattered asymptomatic embolic infarction with subtotal removal of tumor.
Follow-up conventional angiography was performed before discharge, and bilateral ICA maintained patency without stenosis [
DISCUSSION
Acute ischemic stroke is a very urgent and fatal disease that requiring accurate diagnosis and prompt treatment. In our case, ischemic stroke was caused by direct ICA compression of sudden mass increase due to pituitary apoplexy, but it was not a common case.
Direct compression or occlusion of the carotid artery due to pituitary adenoma is a very rare disease and usually asymptomatic. Most patients with symptomatic acute cerebral ischemia reported in the literature were secondary to pituitary apoplexy.[
In general, in the case of a stroke with suspected acute large vessel occlusion, the hemodynamic stroke due to stenosis or embolic infarction should be considered first. Therefore, patients who have large pituitary adenoma cannot give priority always to tumor surgery when an acute ischemic stroke symptom occurs. Moreover, it could be very confusing situation to both the vascular surgeon and the tumor surgeon. In the case of a primary vascular accident accompanied by an incidental finding pituitary adenoma, endovascular intervention should take precedence. Furthermore, in the case of ischemic stroke with vasospasm associated with pituitary adenoma, restoration of perfusion through endovascular intervention before tumor surgery might be more helpful in the patient’s prognosis. Therefore, if large pituitary mass and acute ischemic strokes were found through noninvasive studies, conventional angiography should be performed for accurate cause discrimination. In the case of direct compression of ICA by tumor mass, balloon angioplasty cannot provide a continuous radial force, thus only temporary effect can be achieved and can cause serious complications such as carotid artery dissection. If stent insertion is considered for a lasting radial force, due to dual anti-platelet therapy with stent insertion, it may be dangerous for tumor surgery to be performed later. Therefore, if conventional angiography is performed and direct compression by the tumor is considered to be the main cause of acute ischemic stroke, tumor resection should be preceded rather than endovascular treatment.
To the best of our knowledge, our case is the first time that perfusion study and endovascular intervention were performed before tumor surgery in an ischemic stroke associated with pituitary apoplexy.
CONCLUSION
Although there have been some reports, acute ischemic stroke along with pituitary apoplexy is still very rare. If acute ischemic stroke is associated with large pituitary adenoma, emergency conventional angiography is indispensable for accurate diagnosis. Moreover, emergency decompression surgery should be the first choice when the cause of acute ischemic stroke was thought to be direct compression due to parasellar mass.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahmed SK, Semple PL. Cerebral ischaemia in pituitary apoplexy. Acta Neurochir (Wien). 2008. 150: 1193-6
2. Akutsu H, Noguchi S, Tsunoda T, Sasaki M, Matsumura A. Cerebral infarction following pituitary apoplexy--case report. Neurol Med Chir (Tokyo). 2004. 44: 479-83
3. Pasha SA, Ranganthan LN, Setty VK, Reddy R, Ponnuru DA. Acute ischaemic stroke as a manifestation of pituitary apoplexy in a young lady. J Clin Diagn Res. 2017. 11: OD03-5
4. Rebeiz T, Cueva W, Ardelt A. Unusual case of bilateral caudate infarcts following pituitary apoplexy. JAMA Neurol. 2014. 71: 226-7
5. Rey-Dios R, Payner TD, Cohen-Gadol AA. Pituitary macroadenoma causing symptomatic internal carotid artery compression: Surgical treatment through transsphenoidal tumor resection. J Clin Neurosci. 2014. 21: 541-6
6. Yang SH, Lee KS, Lee KY, Lee SW, Hong YK. Pituitary apoplexy producing internal carotid artery compression: A case report. J Korean Med Sci. 2008. 23: 1113-