- Department of Neuro-Surgery, Govind Ballav Pant Institute of Postgraduate Medical Education and Research (GIPMER), New Delhi, India
Correspondence Address:
Gautam Dutta
Department of Neuro-Surgery, Govind Ballav Pant Institute of Postgraduate Medical Education and Research (GIPMER), New Delhi, India
DOI:10.4103/sni.sni_455_17
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Gautam Dutta, Daljit Singh, Hukum Singh, Arvind Kumar Srivastava, Anita Jagetia, Deepashu Sachdeva. Pituitary fossa chondrosarcoma: An unusual cause of a sellar suprasellar mass masquerading as pituitary adenoma. 09-Apr-2018;9:76
How to cite this URL: Gautam Dutta, Daljit Singh, Hukum Singh, Arvind Kumar Srivastava, Anita Jagetia, Deepashu Sachdeva. Pituitary fossa chondrosarcoma: An unusual cause of a sellar suprasellar mass masquerading as pituitary adenoma. 09-Apr-2018;9:76. Available from: http://surgicalneurologyint.com/surgicalint-articles/pituitary-fossa-chondrosarcoma-an-unusual-cause-of-a-sellar-suprasellar-mass-masquerading-as-pituitary-adenoma/
Abstract
Background:Chondrosarcoma is a mesenchymal malignant tumor composed of tumor cells producing cartilage. It is more commonly found in older age group and usually affects the axial skeleton. Intracranial chondrosarcoma is extremely rare, and chondrosarcoma arising from the sellar region are even rarer with only a few cases described in the literature. We report a case of chondrosarcoma mimicking a sellar suprasellar mass with parasellar extension.
Case Description:A 22-year old male presented with generalized intermittent headache along with diplopia and diminished visual acuity without any history of sexual dysfunction or galactorrhea. His endocrine tests were within normal limits. Magnetic resonance imaging of the brain revealed a large mass which was apparently arising from the sella with a significant suprasellar and left parasellar component with mild compression over the left optic chiasm and deviation of infundibulum to the right. The patient underwent pterional craniotomy and decompression of the mass. The pathologic diagnosis was chondrosarcoma. The patient received postoperative radiotherapy.
Conclusion:This case demonstrates that chondrosarcoma of the sellar region may mimic clinical, endocrinological, and radiological features of more commonly encountered lesions in this region such as nonfunctioning pituitary tumor, craniopharyngioma, meningioma, or chordoma. We discuss the origin, areas of involvement, management, and long-term prognosis of these rare tumors.
Keywords: Chondrosarcoma, parasellar, sellar, suprasellar
INTRODUCTION
Despite overwhelming variety of lesions occurring in the sellar region, at least 75–80% of all sellar/juxtasellar masses are due to one of the “Big Five:” macroadenoma, meningioma, aneurysm, craniopharyngioma, and astrocytoma. Of them, most are of pituitary origin, only approximately 10% are nonpituitary that includes benign and malignant neoplasms, vascular, granulomatous, and inflammatory lesions.[
CASE REPORT
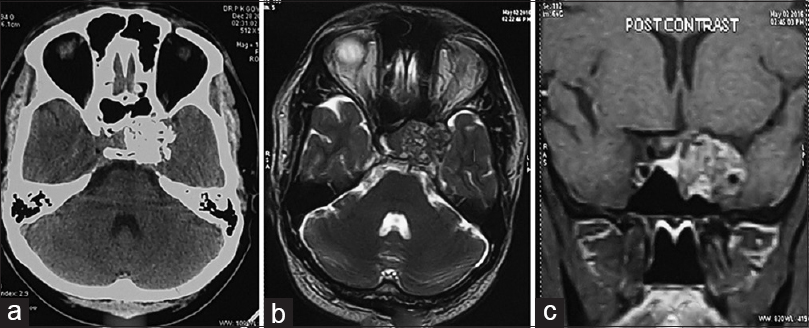
A 22-year-old male patient presented with complaints of generalized intermittent headache for past 2 years along with diplopia and diminished visual acuity for the past 3 months without any history of sexual dysfunction or galactorrhea. On physical examination, he was a healthy appearing male with normal male hair pattern and masculinization. Neuro-ophthalmologic examination including perimetry was suggestive of bilateral temporal hemianopia more prominent on the left side, diminution of vision (6/6 right side and 6/18 left side), along with features of early optic atrophy on the left side and left lateral rectus palsy. Basal endocrine investigations revealed normal prolactin (serum PRL 345 mU/L; normal < 360 mU/L), normal thyroid function [total serum T4 10.20 mcg/dL (normal range 3.20–12.6 mcg/dL); serum TSH 1.35 mIU/mL (normal range 0.35–5.50 mIU/mL); serum T3 115.1 ng/dL (normal range 60–181 ng/dL), normal serum cortisol (283 nmol/L; normal range at 0900 h, 200–600 nmol/L)]. Contrast-enhanced computed tomography (CECT) of the brain revealed an irregular contrast-enhancing calcified lesion at the sellar-suprasellar and left parasellar region with erosion of the posterior and anterior clinoid process and dorsum sellae. Magnetic resonance imaging (MRI) of the brain revealed a large mass which was apparently arising from the sella with a significant suprasellar and left parasellar component with mild compression over the left optic chiasm and deviation of infundibulum to the right. The lesion had heterogenous signal on T1/T2/fluid-attenuated inversion recovery (FLAIR) images with multiple gradient echo (GRE) hypointense area inside the lesion with no diffusion restriction, along with significant enhancement of the mass following administration of IV gadolinium [Figure
The patient underwent left pterional craniotomy and decompression of the mass. Intraoperatively, the mass was hard, pinkish, partly calcified, highly vascular, and engulfing the left carotid. The sellar floor was thin and partly deficient. Postoperative stay was uneventful. Repeat pituitary test (serum prolactin, TSH, T3, T4, and cortisol) performed 72 h post-surgery showed normal levels.
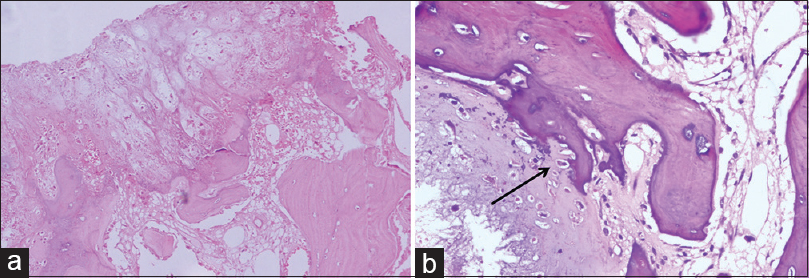
Histology revealed a cartilaginous tumor composed of minimally pleomorphic chondrocytes lying in a cartilaginous matrix with areas of ossification, permeation of bony trabeculae with hyperchromatic nuclei, and inconspicuous nucleoli consistent with well-differentiated chondrosarcoma [
Figure 2
(a) H and E (100×) shows the junction where the tumor is invading and destroying the intercellular lamellated bone (b) H and E 400×, arrow showing invasion and destruction by chondroid cells. The tumor is low grade and sparsely cellular. Prominent nucleoli and single lacunae having two cells were rarely recognized
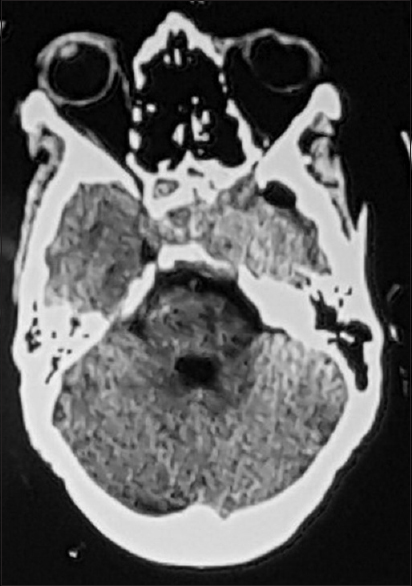
Patient was discharged on postoperative day 10. Postoperative CT brain showed that the tumor was completely removed [
DISCUSSION
Chondrosarcomas are malignant tumors of cartilage-forming cells that occur mainly in the axial part of the skeleton. The commonly involved intracranial areas are petrosal bone, occipital bone, clivus, and sphenoid bone.[
Radiological examination of such tumors almost always shows bone destruction and variable calcification on CT imaging along with involvement of neural and vascular structures on MRI.[
Histologically, chondrosarcoma is classified from grades I to IV according to Evan's classification system.[
In 53% of neurosurgically treated patients, recurrence of the tumor was found with a mean interval of 32 months,[
CONCLUSION
This case demonstrates that chondrosarcoma, a very unusual tumor to arise in the sellar-suprasellar region, can mimic features of the more commonly encountered lesions in this region causing diagnostic dilemmas and resulting in intraoperative surprises. A near-complete resection of the tumor should be the primary goal because this is the most important predictor of outcome, along with regular follow-up to assess recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Allan CA, Kaltsas G, Evanson J, Geddes J, Lowe DG, Plowman PN. Pituitary chondrosarcoma: An unusual cause of a sellar mass presenting as a pituitary adenoma. J Clin Endocrinol Metab. 2001. 86: 386-91
2. Korten AG, Ter Berg HJ, Spincemaille GH, van der Laan RT, Van de Wel AM. Intracranial chondrosarcoma: review of the literature and report of 15 cases. J Neurol Neurosurg Psychiatry. 1998. 65: 88-92
3. Austin-Seymour M, Munzenrider J, Goitein M, Verhey L, Urie M, Gentry R. Fractionated proton radiation therpay of chordoma and low-grade chondrosarcoma of the base of the skull. J Neurosurg. 1989. 70: 13-7
4. Chung YS, Gwak HS, Jung HW, Park HJ, Paek HS, Kim DG. Intracranial chordomas and chondrosarcomas: The effectiveness of surgery and radiation therapy. J Korean Neurosurg Soc. 2000. 29: 910-7
5. Cianfriglia F, Pompili A, Occhipinti E. Intracranial malignant cartilaginous tumours Report of two cases and review of the literature. Acta Neurochir Wien. 1978. 45: 163-75
6. Freda PU, Wardlaw SL, Post KD. Unusual causes of sellar/parasellar masses in a large transsphenoidal surgical series. J Clin Endocrinol Metab. 1996. 81: 3455-9
7. Gay E, Sekhar LN, Rubinstein E, Wright DC, Sen C, Janecka IP. Chordomas and chondrosarcomas of the cranial base: Results and follow-up of 60 patients. Neurosurgery. 1995. 36: 887-96
8. Ishida T, Dorfman H. Chondroid chordoma versus low-grade chondrosarcoma of the base of the skull: Can immunohistochemistry resolve the controversy?. J Neurooncol. 1994. 18: 199-206
9. Kveton JF, Brackman DE, Glasscock ME, House WF, Hitselberger WE. Chondrosarcoma of the skull base. Otolaryngol Head Neck Surg. 1986. 94: 23-32
10. Rosenberg AE, Nielsen GP, Keel SB, Renard LG, Fitzek MM, Munzenrider JE. Chondrosarcoma of the base of the skull: A clinicopathologic study of 200 cases with emphasis on its distinction from chordoma. Am J Surg Pathol. 1999. 23: 1370-8
11. Russell DS, Rubinstein LJ.editors. Pathology of tumors of the nervous systems. London: Edward Arnold; 1989. p. 809-54
12. Salisbury JR, Isaacson PG. Distinguishing chordoma from chondrosarcoma by immunohistochemical techniques. J Pathol. 1986. 148: 251-2
13. Suit HD, Goitein M, Munzenrider J, Verhey L, Davis KR, Koehler A. Definitive radiation therapy for chordoma and chondrosarcoma of the base of skull and cervical spine. J Neurosurg. 1982. 56: 377-85