- Department of Neurosurgery, Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, Delhi, India.
Correspondence Address:
Amit Kumar Sharma, Department of Neurosurgery, Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, Delhi, India.
DOI:10.25259/SNI_551_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Amit Kumar Sharma, Binita Dholakia, Anita Jagetia, Ghanshyam Das Singhal, Shaam Bodeliwala, Arvind Kumar Srivastava, Daljit Singh. Posterior ischemic optic neuropathy with acute monocular vision loss following clipping of anterior communicating artery aneurysm. A case report and review of literature. 20-Sep-2021;12:471
How to cite this URL: Amit Kumar Sharma, Binita Dholakia, Anita Jagetia, Ghanshyam Das Singhal, Shaam Bodeliwala, Arvind Kumar Srivastava, Daljit Singh. Posterior ischemic optic neuropathy with acute monocular vision loss following clipping of anterior communicating artery aneurysm. A case report and review of literature. 20-Sep-2021;12:471. Available from: https://surgicalneurologyint.com/surgicalint-articles/11121/
Abstract
Background: The acute postoperative monocular vision loss following anterior communicating artery aneurysm clipping secondary to posterior ischemic optic neuropathy (PION) a rare presentation.
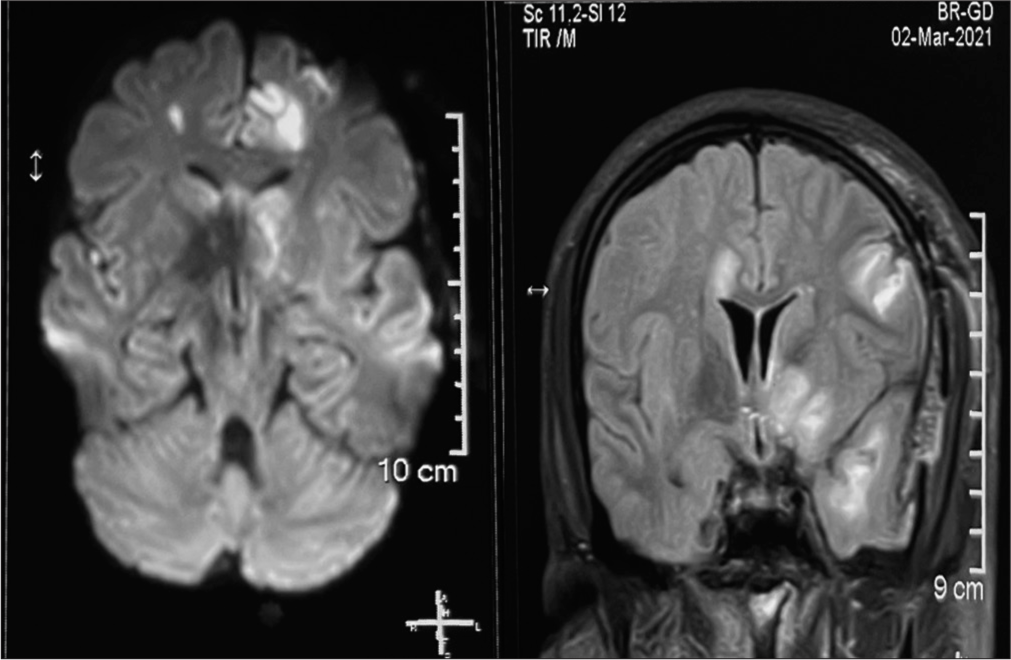
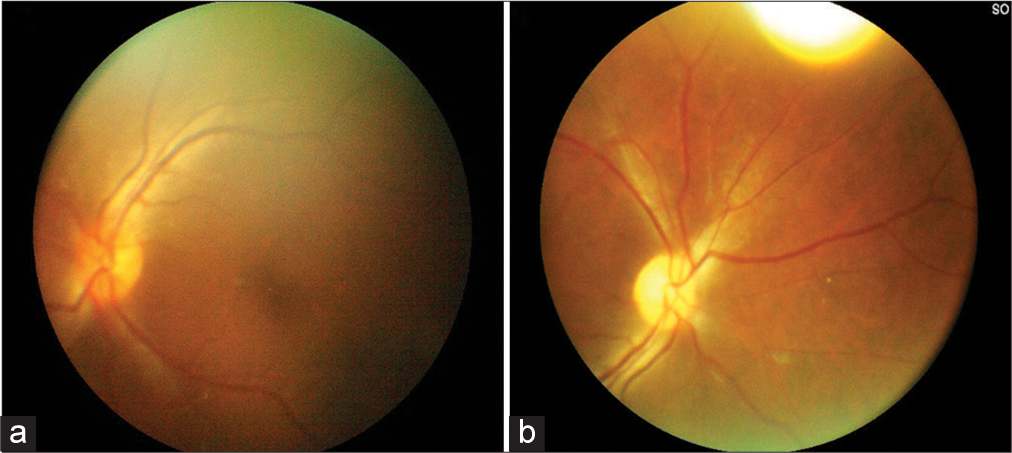
Case Description: A 32-year old patient presented with a spontaneous holocranial thunderclap headache for 7 days, associated with vomiting. The SAH was diagnosed with a tiny saccular aneurysm arising from the anterior communicating artery. A left pterional craniotomy and clipping of aneurysm were done. On the 3rd postoperative day, he complained of left-sided complete blindness, and on the 5th postoperative day, his GCS dropped to E4V1M5 with right-sided hemiplegia. MRI brain showed normal optic apparatus with bilateral ACA and left MCA territory infarct.
Conclusion: The PION must be kept in the differential diagnosis of post-clipping sudden visual deterioration, especially following anterior communicating artery aneurysm rupture.
Keywords: Acomm aneurysm, Monocular blindness, Optic nerve, Posterior ischemic optic neuropathy
INTRODUCTION
Vision loss in aneurysmal SAH (aSAH) is primarily because of intraocular hemorrhage, direct compression of the optic pathway by the sac of the aneurysm, or iatrogenic trauma optic nerve chiasm during the dissection of clipping of the neck and rarely optic neuropathy following aSAH.
CASE REPORT
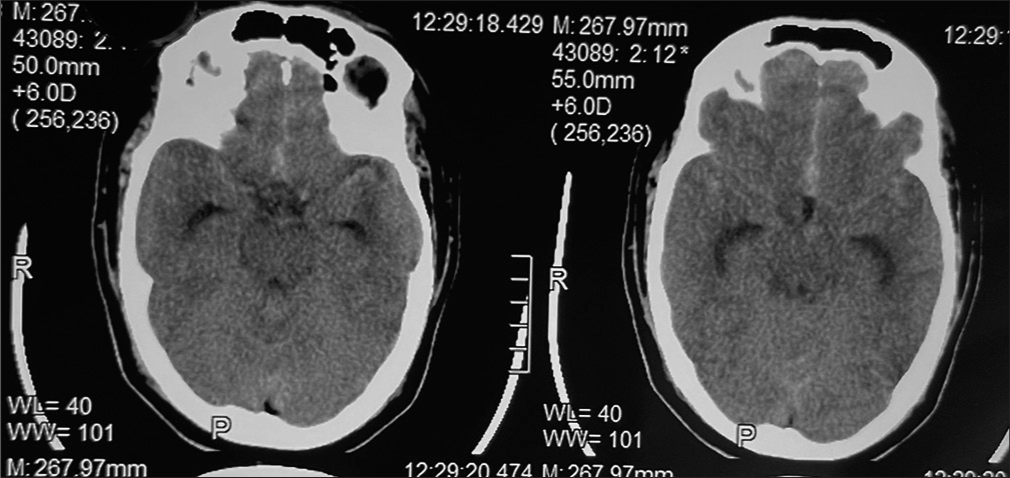
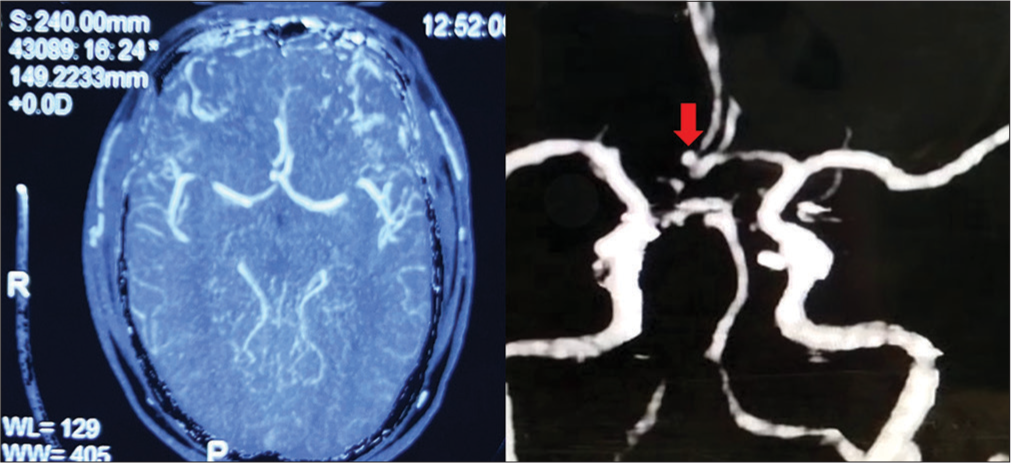
A 32-year-old hypertensive man with a history of alcohol intake for 8 years and was abstaining for 1 year; presented with a sudden holocranial thunderclap-like headache 7 days ago. It was associated with 3–4 episodes of projectile vomiting for 2–3 days without any relief in headache intensity. Neurological examination revealed no deficit. Non-contrast CT scan brain showed SAH in the interhemispheric fissure and bilateral Sylvian fissures (modified Fischer grade-2) with visible temporal horns suggestive of hydrocephalous [
DISCUSSION
After reviewing the available literature, there are only few case reports of postoperative monocular vision loss in anterior communicating artery aneurysm,[
Ruben and Afshar reported a case of small Acomm. Artery aneurysm leading to complete and permanent monocular vision loss.[
CONCLUSION
The possibility of posterior ischemic optic neuropathy must be kept in the differential diagnosis of post-SAH sudden visual deterioration, especially following anterior communicating artery aneurysm rupture.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chung J, Cho YK, Lee YC. A case of orbital infarction syndrome after intracranial aneurysm surgery. J Korean Ophthalmol Soc. 1999. 40: 1684-8
2. Hara N, Mukuno K, Ohtaka H, Shimizu K. Ischemic optic neuropathy associated with subarachnoid hemorrhage after rupture of anterior communicating artery aneurysm. Ophthalmologica. 2003. 217: 79-84
3. Kang SD. Sudden unilateral blindness after intracranial aneurysm surgery. J Korean Neurosurg Soc. 1996. 25: 2438-44
4. Noh CH, Lee HJ, Yi JS, Yang JH, Lee IW, Kim DS. Five cases of orbital infarction syndrome caused by compression of surgical scalp flap. -case report-Korean J Cerebrovasc Surg. 2003. 5: 53-7
5. Park JS, Shin H. A case of bilateral blindness occurred during general anesthesia for anterior cerebral communicating artery aneurysm surgery. J Korean Ophthalmol Soc. 1987. 28: 219-21
6. Ruben S, Afshar F. Visual failure following subarachnoid hemorrhage from an anterior communicating artery aneurysm rupture. J Neurol Neurosurg Psychiatry. 1991. 54: 1017-8
7. Zimmerman CF, Van Patten PD, Golnik KC. Orbital infarction syndrome after surgery for intracranial aneurysms. Ophthalmology. 1995. 102: 594-8